Abstract
Background
This study examines the epidemiological trends of oropharyngeal squamous cell carcinoma (OPSCC) and oral cavity squamous cell carcinoma (OCSCC) in Northern New England.
Methods
Data were obtained from the Maine, New Hampshire and Vermont cancer registries. The age-standardized incidence rates (ASIR), age-specific incidence rates, and annual percentage changes (APC) for OPSCC and OCSCC were calculated using Joinpoint regression.
Results
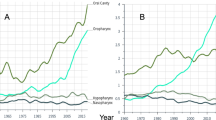
The overall ASIR for OPSCC in Northern New England increased by 54.2% from 2000 to 2013 with an increase of 61.5% and 27.3% in men and women, respectively. Overall ASIR for OCSCC, on the other hand, declined throughout 2000 to 2013 by 6% and among men by 11%. In joinpoint analyses, the overall ASIRs for OPSCC significantly increased at an APC of 3.15 from 2000 to 2013, whereas the ASIRs for OCSCC remained stable at an APC of − 0.26. In men, ASIRs for OPSCC significantly increased (APC: 3.46), while that of OCSCC remained stable at an APC of − 0.87. In women, the ASIRs remained stable for both OPSCC and OCSCC at an APC of 1.97 and 0.49, respectively. For patients in the 6th decade of life, the age-specific incidence rates for OPSCC increased significantly at an APC of 3.06, also among those in the 7th and 8th decade with a significant increase at an APC of 4.98 and 3.51 per year, respectively. There were no significant changes in the APC of patients with OCSCC with respect to age group.
Conclusion
The overall incidence of OPSCC is increasing in Northern New England, specifically among men. Given the etiological association between OPSCC and HPV, vaccination against HPV should be effectively encouraged among the populace. The efforts on tobacco cessation, abstinence, and alcohol abuse control should be continually expanded in order to bring about a decreasing trend in OCSCC.




Similar content being viewed by others
References
Secretan B, Straif K, Baan R, Grosse Y, El Ghissassi F, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V, Group WHOIAfRoCMW (2009) A review of human carcinogens—part E: tobacco, areca nut, alcohol, coal smoke, and salted fish. Lancet Oncol 10(11):1033–1034
Fioretti F, Bosetti C, Tavani A, Franceschi S, La Vecchia C (1999) Risk factors for oral and pharyngeal cancer in never smokers. Oral Oncol 35(4):375–378
Wheeler CM, Hunt WC, Joste NE, Key CR, Quint WG, Castle PE (2009) Human papillomavirus genotype distributions: implications for vaccination and cancer screening in the United States. J Natl Cancer Inst 101(7):475–487. https://doi.org/10.1093/jnci/djn510
Ouhoummane N, Steben M, Coutlee F, Vuong T, Forest P, Rodier C, Louchini R, Duarte E, Brassard P (2013) Squamous anal cancer: patient characteristics and HPV type distribution. Cancer Epidemiol 37(6):807–812. https://doi.org/10.1016/j.canep.2013.09.015
Miralles-Guri C, Bruni L, Cubilla AL, Castellsague X, Bosch FX, de Sanjose S (2009) Human papillomavirus prevalence and type distribution in penile carcinoma. J Clin Pathol 62(10):870–878. https://doi.org/10.1136/jcp.2008.063149
Gillison ML, Koch WM, Capone RB, Spafford M, Westra WH, Wu L, Zahurak ML, Daniel RW, Viglione M, Symer DE, Shah KV, Sidransky D (2000) Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. J Natl Cancer Inst 92(9):709–720
Steinau M, Saraiya M, Goodman MT, Peters ES, Watson M, Cleveland JL, Lynch CF, Wilkinson EJ, Hernandez BY, Copeland G, Saber MS, Hopenhayn C, Huang Y, Cozen W, Lyu C, Unger ER, Workgroup HPVToC (2014) Human papillomavirus prevalence in oropharyngeal cancer before vaccine introduction, United States. Emerg Infect Dis 20(5):822–828. https://doi.org/10.3201/eid2005.131311
Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER, Centers for Disease C, Prevention, Advisory Committee on Immunization P (2007) Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 56(RR-2):1–24
Koutsky LA, Galloway DA, Holmes KK (1988) Epidemiology of genital human papillomavirus infection. Epidemiol Rev 10:122–163
Koutsky L (1997) Epidemiology of genital human papillomavirus infection. Am J Med 102(5A):3–8
Wiest T, Schwarz E, Enders C, Flechtenmacher C, Bosch FX (2002) Involvement of intact HPV16 E6/E7 gene expression in head and neck cancers with unaltered p53 status and perturbed pRb cell cycle control. Oncogene 21(10):1510–1517. https://doi.org/10.1038/sj.onc.1205214
Marur S, D’Souza G, Westra WH, Forastiere AA (2010) HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol 11(8):781–789. https://doi.org/10.1016/S1470-2045(10)70017-6
Nasman A, Attner P, Hammarstedt L, Du J, Eriksson M, Giraud G, Ahrlund-Richter S, Marklund L, Romanitan M, Lindquist D, Ramqvist T, Lindholm J, Sparen P, Ye W, Dahlstrand H, Munck-Wikland E, Dalianis T (2009) Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int J Cancer 125(2):362–366. https://doi.org/10.1002/ijc.24339
Bhosale PG, Pandey M, Desai RS, Patil A, Kane S, Prabhash K, Mahimkar MB (2016) Low prevalence of transcriptionally active human papilloma virus in Indian patients with HNSCC and leukoplakia. Oral Surg Oral Med Oral Pathol Oral Radiol 122(5):609–618. https://doi.org/10.1016/j.oooo.2016.06.006
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386. https://doi.org/10.1002/ijc.29210
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, Razzaghi H, Saraiya M (2016) Human papillomavirus-associated cancers—United States, 2008–2012. MMWR Morb Mortal Wkly Rep 65(26):661–666. https://doi.org/10.15585/mmwr.mm6526a1
Chaturvedi AK, Engels EA, Anderson WF, Gillison ML (2008) Incidence trends for human papillomavirus-related and -unrelated oral squamous cell carcinomas in the United States. J Clin Oncol 26(4):612–619. https://doi.org/10.1200/JCO.2007.14.1713
Mourad M, Jetmore T, Jategaonkar AA, Moubayed S, Moshier E, Urken ML (2017) Epidemiological trends of head and neck cancer in the United States: a SEER population study. J Oral Maxillofac Surg 75(12):2562–2572. https://doi.org/10.1016/j.joms.2017.05.008
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, Liu L, Lynch CF, Wentzensen N, Jordan RC, Altekruse S, Anderson WF, Rosenberg PS, Gillison ML (2011) Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol 29(32):4294–4301. https://doi.org/10.1200/JCO.2011.36.4596
Forte T, Niu J, Lockwood GA, Bryant HE (2012) Incidence trends in head and neck cancers and human papillomavirus (HPV)-associated oropharyngeal cancer in Canada, 1992–2009. Cancer Causes Control 23(8):1343–1348. https://doi.org/10.1007/s10552-012-0013-z
Monteiro LS, Antunes L, Bento MJ, Warnakulasuriya S (2013) Incidence rates and trends of lip, oral and oro-pharyngeal cancers in Portugal. J Oral Pathol Med 42(4):345–351. https://doi.org/10.1111/jop.12010
Blomberg M, Nielsen A, Munk C, Kjaer SK (2011) Trends in head and neck cancer incidence in Denmark, 1978–2007: focus on human papillomavirus associated sites. Int J Cancer 129(3):733–741. https://doi.org/10.1002/ijc.25699
Boscolo-Rizzo P, Zorzi M, Del Mistro A, Da Mosto MC, Tirelli G, Buzzoni C, Rugge M, Polesel J, Guzzinati S, Group AW (2018) The evolution of the epidemiological landscape of head and neck cancer in Italy: Is there evidence for an increase in the incidence of potentially HPV-related carcinomas? PLoS ONE 13(2):e0192621. https://doi.org/10.1371/journal.pone.0192621
Jehannin-Ligier K, Belot A, Guizard AV, Bossard N, Launoy G, Uhry Z, Network F (2017) Incidence trends for potentially human papillomavirus-related and -unrelated head and neck cancers in France using population-based cancer registries data: 1980–2012. Int J Cancer 140(9):2032–2039. https://doi.org/10.1002/ijc.30631
van Monsjou HS, Schaapveld M, van den Brekel MW, Balm AJ (2015) The epidemiology of head and neck squamous cell carcinoma in the Netherlands during the era of HPV-related oropharyngeal squamous cell carcinoma. Is there really evidence for a change? Oral Oncol 51(10):901–907. https://doi.org/10.1016/j.oraloncology.2015.06.011
Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S (2017) National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep 66(33):874–882. https://doi.org/10.15585/mmwr.mm6633a2
Johnson KL, Lin MY, Cabral H, Kazis LE, Katz IT (2017) Variation in human papillomavirus vaccine uptake and acceptability between female and male adolescents and their caregivers. J Community Health 42(3):522–532. https://doi.org/10.1007/s10900-016-0284-5
Gilkey MB, Malo TL, Shah PD, Hall ME, Brewer NT (2015) Quality of physician communication about human papillomavirus vaccine: findings from a national survey. Cancer Epidemiol Biomark Prev 24(11):1673–1679. https://doi.org/10.1158/1055-9965.EPI-15-0326
Perkins RB, Clark JA (2012) Providers’ attitudes toward human papillomavirus vaccination in young men: challenges for implementation of 2011 recommendations. Am J Mens Health 6(4):320–323. https://doi.org/10.1177/1557988312438911
Lu PJ, Yankey D, Jeyarajah J, O’Halloran A, Elam-Evans LD, Smith PJ, Stokley S, Singleton JA, Dunne EF (2015) HPV vaccination coverage of male adolescents in the United States. Pediatrics 136(5):839–849. https://doi.org/10.1542/peds.2015-1631
Winer RL, Hughes JP, Feng Q, Stern JE, Xi LF, Koutsky LA (2016) Incident detection of high-risk human papillomavirus infections in a cohort of high-risk women aged 25–65 years. J Infect Dis 214(5):665–675. https://doi.org/10.1093/infdis/jiw074
Han JJ, Beltran TH, Song JW, Klaric J, Choi YS (2017) Prevalence of genital human papillomavirus infection and human papillomavirus vaccination rates among US adult men: National Health and Nutrition Examination Survey (NHANES) 2013–2014. JAMA Oncol 3(6):810–816. https://doi.org/10.1001/jamaoncol.2016.6192
Daley EM, Thompson EL, Vamos CA, Griner SB, Vazquez-Otero C, Best AL, Kline NS, Merrell LK (2016) HPV-related knowledge among dentists and dental hygienists. J Cancer Educ. https://doi.org/10.1007/s13187-016-1156-5
Vazquez-Otero C, Vamos CA, Thompson EL, Merrell LK, Griner SB, Kline NS, Catalanotto FA, Giuliano AR, Daley EM (2018) Assessing dentists’ human papillomavirus-related health literacy for oropharyngeal cancer prevention. J Am Dent Assoc 149(1):9–17. https://doi.org/10.1016/j.adaj.2017.08.021
American Dental Association Statement on human papilomavirus and cancers of the oral cavity and oropharynx. https://www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/statement-on-human-papillomavirus-and-squamous-cel. Accessed 18 May 2018
U.S. Department of Health and Human Services (2014) The health consequences of smoking-50 years of progress: a report of the surgeon general. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta
U.S. Department of Health and Human Services (2016) E-cigarette use among youth and young adults: a report of the surgeon general-executive summary. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, Atlanta
Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, Stone MD, Khoddam R, Samet JM, Audrain-McGovern J (2015) Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA 314(7):700–707. https://doi.org/10.1001/jama.2015.8950
Haughwout SP, LaVallee RA, Castle IP (2016) Apparent per Capita Alcohol Consumption: National, State, and Regional Trends, 1977–2014 (SURVEILLANCE REPORT #104). National Institute on Alcohol Abuse and Alcoholism Division of Epidemiology and Prevention Research Alcohol Epidemiologic Data System
Bien TH, Burge R (1990) Smoking and drinking: a review of the literature. Int J Addict 25(12):1429–1454
Grucza RA, Bierut LJ (2006) Co-occurring risk factors for alcohol dependence and habitual smoking: update on findings from the Collaborative Study on the Genetics of Alcoholism. Alcohol Res Health 29(3):172–178
Morgen CS, Bove KB, Larsen KS, Kjaer SK, Gronbaek M (2008) Association between smoking and the risk of heavy drinking among young women: a prospective study. Alcohol Alcohol 43(3):371–375. https://doi.org/10.1093/alcalc/agn001
Acknowledgments
This project was supported in part by the Centers for Disease Control and Prevention’s National Program of Cancer Registries, cooperative agreement 5U58DP003930 awarded to the New Hampshire Department of Health and Human Services, Division of Public Health Services, Bureau of Public Health Statistics and Informatics, Office of Health Statistics and Data Management. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the New Hampshire Department of Health and Human Services. This project was also supported in part by the cooperative agreement 1NU58DP006297 funded by the Centers for Disease Control and Prevention awarded to the Maine Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Maine Centers for Disease Control and Prevention or the Department of Health and Human Services. We would like to thank Maine, New Hampshire and Vermont Cancer Registries for sharing the states data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no financial conflicts associated with this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Owosho, A.A., Velez, M., Tyburski, A. et al. Epidemiological trends of oropharyngeal and oral cavity squamous cell carcinomas in Northern New England, 2000–2013. Cancer Causes Control 30, 291–299 (2019). https://doi.org/10.1007/s10552-019-1136-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-1136-2