Abstract
Growing evidence supports that air pollution has become an important risk factor for developing diabetes mellitus. Understanding the contributing effect of air pollution in population studies, elucidating the potential mechanisms involved, and identifying the most responsible pollutants are all required in order to promulgate successful changes in policy and to help formulate preventive measures in an effort to reduce the risk for diabetes. This review summarizes recent findings from epidemiologic studies and mechanistic insights that provide links between exposure to air pollution and a heightened risk for diabetes.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60. doi:10.1016/S0140-6736(12)61766-8.
Brook RD, Rajagopalan S, Pope 3rd CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78. doi:10.1161/CIR.0b013e3181dbece1.
Mustafic H, Jabre P, Caussin C, Murad MH, Escolano S, Tafflet M, et al. Main air pollutants and myocardial infarction: a systematic review and meta-analysis. Jama. 2012;307(7):713–21. doi:10.1001/jama.2012.126.
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, et al. Long term exposure to ambient air pollution and incidence of acute coronary events: Prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014;348:f7412. doi:10.1136/bmj.f7412.
Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: Mechanistic insights. Diabetes. 2012;61(12):3037–45. doi:10.2337/db12-0190.
Zhao X, Sun Z, Ruan Y, Yan J, Mukherjee B, Yang F, et al. Personal black carbon exposure influences ambulatory blood pressure: Air pollution and cardiometabolic disease (AIRCMD-China) study. Hypertension. 2014;63(4):871–7. doi:10.1161/HYPERTENSIONAHA.113.02588.
Brook RD, Jerrett M, Brook JR, Bard RL, Finkelstein MM. The relationship between diabetes mellitus and traffic-related air pollution. J Occup Environ Med. 2008;50(1):32–8.
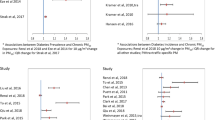
Pearson JF, Bachireddy C, Shyamprasad S, Goldfine AB, Brownstein JS. Association between fine particulate matter and diabetes prevalence in the USA. Diabetes Care. 2010;33(10):2196–201. doi:10.2337/dc10-0698.
Eze IC, Schaffner E, Fischer E, Schikowski T, Adam M, Imboden M, et al. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ Int. 2014;70:95–105. doi:10.1016/j.envint.2014.05.014. This work add further evidence showing an association between air pollution and diabetes. More importantly, the association could be observed even at low levels exposure which are below air quality guidelines.
Kramer U, Herder C, Sugiri D, Strassburger K, Schikowski T, Ranft U, et al. Traffic-related air pollution and incident type 2 diabetes: Results from the SALIA cohort study. Environ Health Perspect. 2010;118(9):1273–9. doi:10.1289/ehp.0901689.
Andersen ZJ, Raaschou-Nielsen O, Ketzel M, Jensen SS, Hvidberg M, Loft S, et al. Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care. 2012;35(1):92–8. doi:10.2337/dc11-1155.
Coogan PF, White LF, Jerrett M, Brook RD, Su JG, Seto E, et al. Air Pollution and Incidence of Hypertension and Diabetes in African American Women Living in Los Angeles. Circulation. 2012. doi:10.1161/CIRCULATIONAHA.111.052753.
Dijkema MB, Mallant SF, Gehring U, van den Hurk K, Alssema M, van Strien RT, et al. Long-term exposure to traffic-related air pollution and type 2 diabetes prevalence in a cross-sectional screening-study in the Netherlands. Environ Health. 2011;10:76. doi:10.1186/1476-069X-10-76.
Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F. Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect. 2011;119(3):384–9. doi:10.1289/ehp.1002344.
McConnell R, Shen E, Gilliland FD, Jerrett M, Wolch J, Chang CC et al. A longitudinal cohort study of body mass index and childhood exposure to secondhand tobacco smoke and air pollution: the southern California children’s health study. Environ Health Perspect. 2014.
Jerrett M, McConnell R, Wolch J, Chang R, Lam C, Dunton G, et al. Traffic-related air pollution and obesity formation in children: a longitudinal, multilevel analysis. Environ Health. 2014;13:49. doi:10.1186/1476-069X-13-49.
Wang Y, Eliot MN, Kuchel GA, Schwartz J, Coull BA, Mittleman MA, et al. Long-term exposure to ambient air pollution and serum leptin in older adults: Results from the MOBILIZE Boston study. J Occup Environ Med. 2014;56(9):e73–7. doi:10.1097/JOM.0000000000000253.
Xu X, Yavar Z, Verdin M, Ying Z, Mihai G, Kampfrath T, et al. Effect of early particulate air pollution exposure on obesity in mice: Role of p47phox. Arterioscler Thromb Vasc Biol. 2010;30(12):2518–27. doi:10.1161/ATVBAHA.110.215350.
Sun Q, Yue P, Deiuliis JA, Lumeng CN, Kampfrath T, Mikolaj MB, et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation. 2009;119(4):538–46.
Muoio DM, Newgard CB. Mechanisms of disease: molecular and metabolic mechanisms of insulin resistance and beta-cell failure in type 2 diabetes. Nat Rev Mol Cell Biol. 2008;9(3):193–205. doi:10.1038/nrm2327.
Marx J. Unraveling the causes of diabetes. Science. 2002;296(5568):686–9. doi:10.1126/science.296.5568.686.
Kelishadi R, Mirghaffari N, Poursafa P, Gidding SS. Lifestyle and environmental factors associated with inflammation, oxidative stress and insulin resistance in children. Atherosclerosis. 2009;203(1):311–9. doi:10.1016/j.atherosclerosis.2008.06.022.
Kim JH, Hong YC. GSTM1, GSTT1, and GSTP1 polymorphisms and associations between air pollutants and markers of insulin resistance in elderly Koreans. Environ Health Perspect. 2012;120(10):1378–84. doi:10.1289/ehp.1104406.
Thiering E, Cyrys J, Kratzsch J, Meisinger C, Hoffmann B, Berdel D, et al. Long-term exposure to traffic-related air pollution and insulin resistance in children: Results from the GINIplus and LISAplus birth cohorts. Diabetologia. 2013;56(8):1696–704. doi:10.1007/s00125-013-2925-x.
Brook RD, Xu X, Bard RL, Dvonch JT, Morishita M, Kaciroti N, et al. Reduced metabolic insulin sensitivity following sub-acute exposures to low levels of ambient fine particulate matter air pollution. Sci Total Environ. 2013;448:66–71. doi:10.1016/j.scitotenv.2012.07.034.
Zanobetti A, Dominici F, Wang Y, Schwartz JD. A national case-crossover analysis of the short-term effect of PM2.5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ Health. 2014;13(1):38. doi:10.1186/1476-069X-13-38.
Dales RE, Cakmak S, Vidal CB, Rubio MA. Air pollution and hospitalization for acute complications of diabetes in Chile. Environ Int. 2012;46:1–5. doi:10.1016/j.envint.2012.05.002.
Tamayo T, Rathmann W, Kramer U, Sugiri D, Grabert M, Holl RW. Is particle pollution in outdoor air associated with metabolic control in type 2 diabetes? PLoS One. 2014;9(3):e91639. doi:10.1371/journal.pone.0091639.
Zanobetti A, Luttmann-Gibson H, Horton ES, Cohen A, Coull BA, Hoffmann B, et al. Brachial artery responses to ambient pollution, temperature, and humidity in people with type 2 diabetes: a repeated-measures study. Environ Health Perspect. 2014;122(3):242–8. doi:10.1289/ehp.1206136.
O'Neill MS, Veves A, Zanobetti A, Sarnat JA, Gold DR, Economides PA, et al. Diabetes enhances vulnerability to particulate air pollution-associated impairment in vascular reactivity and endothelial function. Circulation. 2005;111(22):2913–20. doi:10.1161/CIRCULATIONAHA.104.517110.
Vora R, Zareba W, Utell MJ, Pietropaoli AP, Chalupa D, Little EL, et al. Inhalation of ultrafine carbon particles alters heart rate and heart rate variability in people with type 2 diabetes. Part Fibre Toxicol. 2014;11(1):31. doi:10.1186/s12989-014-0031-y.
Brook RD, Cakmak S, Turner MC, Brook JR, Crouse DL, Peters PA, et al. Long-term fine particulate matter exposure and mortality from diabetes mellitus in Canada. Diabetes Care. 2013. doi:10.2337/dc12-2189. This is a study demonstrating long-term air pollution exposure, even at low levels, is associated with an increased risk of diabetes mortality.
Raaschou-Nielsen O, Sorensen M, Ketzel M, Hertel O, Loft S, Tjonneland A, et al. Long-term exposure to traffic-related air pollution and diabetes-associated mortality: a cohort study. Diabetologia. 2013;56(1):36–46. doi:10.1007/s00125-012-2698-7.
Goldberg SL, Chen L, Guerin A, Macalalad AR, Liu N, Kaminsky M, et al. Association between molecular monitoring and long-term outcomes in chronic myelogenous leukemia patients treated with first line imatinib. Curr Med Res Opin. 2013;29(9):1075–82. doi:10.1185/03007995.2013.812034.
Janghorbani M, Momeni F, Mansourian M. Systematic review and meta analysis of air pollution exposure and risk of diabetes. Eur J Epidemiol. 2014;29(4):231–42. doi:10.1007/s10654-014-9907-2.
Rioux CL, Tucker KL, Brugge D, Gute DM, Mwamburi M. Traffic exposure in a population with high prevalence type 2 diabetes—do medications influence concentrations of C-reactive protein? Environ Pollut. 2011;159(8–9):2051–60. doi:10.1016/j.envpol.2010.12.025.
Khafaie MA, Salvi SS, Ojha A, Khafaie B, Gore SS, Yajnik CS. Systemic inflammation (C-reactive protein) in type 2 diabetic patients is associated with ambient air pollution in Pune City. India Diabetes Care. 2013;36(3):625–30. doi:10.2337/dc12-0388.
Teichert T, Vossoughi M, Vierkotter A, Sugiri D, Schikowski T, Schulte T, et al. Association between traffic-related air pollution, subclinical inflammation and impaired glucose metabolism: Results from the SALIA study. PLoS One. 2013;8(12):e83042. doi:10.1371/journal.pone.0083042.
Xu X, Liu C, Xu Z, Tzan K, Zhong M, Wang A, et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci. 2011;124(1):88–98. doi:10.1093/toxsci/kfr211.
Liu C, Xu X, Bai Y, Wang TY, Rao X, Wang A, et al. Air pollution-mediated susceptibility to inflammation and insulin resistance: Influence of CCR2 pathways in mice. Environ Health Perspect. 2014;122(1):17–26. doi:10.1289/ehp.1306841.
Zheng Z, Xu X, Zhang X, Wang A, Zhang C, Huttemann M, et al. Exposure to ambient particulate matter induces a NASH-like phenotype and impairs hepatic glucose metabolism in an animal model. J Hepatol. 2013;58(1):148–54. doi:10.1016/j.jhep.2012.08.009.
Liu C, Bai Y, Xu X, Sun L, Wang A, Wang TY, et al. Exaggerated effects of particulate matter air pollution in genetic type II diabetes mellitus. Part Fibre Toxicol. 2014;11:27. doi:10.1186/1743-8977-11-27.
Bass V, Gordon CJ, Jarema KA, MacPhail RC, Cascio WE, Phillips PM, et al. Ozone induces glucose intolerance and systemic metabolic effects in young and aged Brown Norway rats. Toxicol Appl Pharmacol. 2013;273(3):551–60. doi:10.1016/j.taap.2013.09.029.
Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–7. doi:10.1038/nature05485.
Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–7. doi:10.1038/nature05488.
Horng T, Hotamisligil GS. Linking the inflammasome to obesity-related disease. Nat Med. 2011;17(2):164–5. doi:10.1038/nm0211-164.
Dostert C, Petrilli V, Van Bruggen R, Steele C, Mossman BT, Tschopp J. Innate immune activation through Nalp3 inflammasome sensing of asbestos and silica. Science. 2008;320(5876):674–7. doi:10.1126/science.1156995.
Bauer RN, Diaz-Sanchez D, Jaspers I. Effects of air pollutants on innate immunity: the role of Toll-like receptors and nucleotide-binding oligomerization domain-like receptors. J Allergy Clin Immunol. 2012;129(1):14–24. doi:10.1016/j.jaci.2011.11.004. quiz 5–6.
Kampfrath T, Maiseyeu A, Ying Z, Shah Z, Deiuliis JA, Xu X, et al. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ Res. 2011;108(6):716–26. doi:10.1161/CIRCRESAHA.110.237560.
Goto Y, Ishii H, Hogg JC, Shih CH, Yatera K, Vincent R, et al. Particulate matter air pollution stimulates monocyte release from the bone marrow. Am J Respir Crit Care Med. 2004;170(8):891–7. doi:10.1164/rccm.200402-235OC.
Deiuliis JA, Kampfrath T, Zhong J, Oghumu S, Maiseyeu A, Chen LC, et al. Pulmonary T cell activation in response to chronic particulate air pollution. Am J Physiol Lung Cell Mol Physiol. 2011. doi:10.1152/ajplung.00261.2011.
Dominici F, Peng RD, Ebisu K, Zeger SL, Samet JM, Bell ML. Does the effect of PM10 on mortality depend on PM nickel and vanadium content? A reanalysis of the NMMAPS data. Environ Health Perspect. 2007;115(12):1701–3. doi:10.1289/ehp.10737.
Liberda EN, Cuevas AK, Gillespie PA, Grunig G, Qu Q, Chen LC. Exposure to inhaled nickel nanoparticles causes a reduction in number and function of bone marrow endothelial progenitor cells. Inhal Toxicol. 2010;22 Suppl 2:95–9. doi:10.3109/08958378.2010.515269.
Liu C, Ying Z, Harkema J, Sun Q, Rajagopalan S. Epidemiological and experimental links between air pollution and type 2 diabetes. Toxicol Pathol. 2013;41(2):361–73. doi:10.1177/0192623312464531.
Watterson TL, Hamilton B, Martin R, Coulombe Jr RA. Urban particulate matter causes ER stress and the unfolded protein response in human lung cells. Toxicol Sci. 2009;112(1):111–22. doi:10.1093/toxsci/kfp186.
Laing S, Wang G, Briazova T, Zhang C, Wang A, Zheng Z, et al. Airborne particulate matter selectively activates endoplasmic reticulum stress response in the lung and liver tissues. Am J Physiol Cell Physiol. 2010;299(4):C736–49. doi:10.1152/ajpcell.00529.2009.
Mendez R, Zheng Z, Fan Z, Rajagopalan S, Sun Q, Zhang K. Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am J Transl Res. 2013;5(2):224–34.
Xu Z, Xu X, Zhong M, Hotchkiss IP, Lewandowski RP, Wagner JG, et al. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part Fibre Toxicol. 2011;8:20. doi:10.1186/1743-8977-8-20.
Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122(1):153–62. doi:10.1172/JCI59660.
Nakane H. Translocation of particles deposited in the respiratory system: a systematic review and statistical analysis. Environ Health Prev Med. 2012;17(4):263–74. doi:10.1007/s12199-011-0252-8.
Block ML, Elder A, Auten RL, Bilbo SD, Chen H, Chen JC, et al. The outdoor air pollution and brain health workshop. Neurotoxicology. 2012;33(5):972–84. doi:10.1016/j.neuro.2012.08.014.
Fonken LK, Xu X, Weil ZM, Chen G, Sun Q, Rajagopalan S et al. Air pollution impairs cognition, provokes depressive-like behaivors and alters hippocampal cytokine expression and morphology. Mol Psychiatry. 2011;16(10):987–95, 73. doi:10.1038/mp.2011.76
Ying Z, Xu X, Bai Y, Zhong J, Chen M, Liang Y, et al. Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect. 2014;122(1):79–86. doi:10.1289/ehp.1307151. This study demonstrated sympathetic activation in CNS mediates hypertensive action of chronic PM2.5 exposure.
Acknowledgments
This work was supported by the United States Environmental Protection Agency grant RD83479701 (S. Rajagopalan and R. Brook) and R01ES015146-06, R01ES019616-04, and R01ES017290-05 (S. Rajagopalan). J. Montresor-Lopez’ and R. Puett’s work was partially supported by grant R01ES019168 from the National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIEHS, NIH. The authors acknowledge Jessica Green-Barnes for her assistance with tables.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Xiaoquan Rao, Jessica Montresor-Lopez, Robin Puett, Sanjay Rajagopalan, and Robert D. Brook declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
No original research was performed for or presented in this review paper. Therefore, this article does not contain any studies with human or animal subjects performed by any of the authors. With regard to the authors’ human research cited in this paper, all procedures were followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. With regard to the authors’ animal study cited in this paper, all applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pathogenesis of Type 2 Diabetes and Insulin Resistance
Rights and permissions
About this article
Cite this article
Rao, X., Montresor-Lopez, J., Puett, R. et al. Ambient Air Pollution: An Emerging Risk Factor for Diabetes Mellitus. Curr Diab Rep 15, 33 (2015). https://doi.org/10.1007/s11892-015-0603-8
Published:
DOI: https://doi.org/10.1007/s11892-015-0603-8