Abstract
Background
Evidence suggests exercise may benefit patients with advanced progressive illness and some hospice day services now provide dedicated gym space. However, supporting data for such a service development are limited. We describe patient referrals, interventions, feedback, and potential impact of a nine-session, outpatient, hospice-based, circuit exercise programme.
Methods
Consecutive referrals to physiotherapy over a 6-month period commencing March 2013 were followed prospectively. Physical function (short physical performance battery (SPPB), grip strength), fatigue (Functional Assessment of Chronic Illness Therapy), psychological well-being (General Health Questionnaire), and patient satisfaction (FACIT-PS) were assessed pre- and post-programme.
Results
Of 212 referrals, 61 (29%) with a range of cancer and non-cancer diagnoses (median [inter-quartile range] survival 67 [50–137] days) were considered appropriate for the circuits of whom 54 (89%) started. There were no statistical differences between those completing and not-completing with regards to age, diagnosis, social status, or survival. In completers (n = 28), 4-m gait speed (mean Δ [95% confidence intervals] 0.23 [0.03, 0.44] m/seconds), five sit-to-stand time (mean Δ −5.44 [−10.43, −0.46] seconds) and overall SPPB score changed statistically, while grip strength did not (mean Δ 0.65 [−1.39, 2.96] kg). Psychological well-being, quality of life, and fatigue remained unchanged. Patients felt the physiotherapists gave clear explanations, understood their needs, and would recommend the service to others.
Conclusion
A hospice-based programme is one way to offer exercise to a range of patients with advanced progressive illness. Despite excellent feedback, only half of patients completed the nine-session programme in full and evidence of benefit was limited. Future work should explore the broader benefits of participation and whether delivering programmes or elements of them in shorter time frames is more beneficial.
Keywords: Exercise, Hospice, Palliative care, Rehabilitation, Service evaluation
Introduction
Therapeutic exercises improve physical fitness, psychological well-being, and quality of life in patients with early stage cancer and other chronic illness.1–3 Early evidence suggests patients with advanced progressive illness may also benefit from exercise.4 For example, patients with advanced cancer completing an 8-week group-based aerobic and resistance training programme demonstrated improved physical function and psychological well-being.5 In line with this, the provision of dedicated space for exercise within the hospice setting is growing.6 However, data to support service development in this area are limited, particularly with regard to components and outcomes of services, and which models of rehabilitation are most effective for which patients.
Physiotherapy services in palliative care have historically followed a one-to-one model of care. Group-based models potentially allow more patients to access supervised exercise, encourage peer support and encouragement, and are well established in palliative care in the form of day-care services. Locally, St Christopher's Hospice provides a proactive rehabilitation service with the aim of improving or maintaining physical and/or psychological functioning, quality of life, and patient well-being. This paper focuses on one component of the service; the circuit-based exercise groups. Using informative service evaluation data, our aims were to describe the patients referred, interventions provided, user feedback, and begin to explore the impact of this type of intervention.
Methods
Setting and patient referral
St Christopher's Hospice in southeast London provides specialist palliative care to over 2000 adults each year from a diverse population of 1.5 million people across five London boroughs. Founded in 1967 by Dame Cicely Saunders, it is widely regarded as the first modern hospice. Care is provided across three settings: the Anniversary Centre from where patients access day care and outpatient appointments; Homecare where patients are seen in their own homes; and the Inpatient Unit where patients are admitted for symptom control, psychosocial, and/or end-of-life care.
The current rehabilitation gym was built in 2007 and can be accessed by all patients under the hospice's care, with transport provided to outpatients where required. It is open on Monday to Friday and is the primary space for physiotherapy interventions, containing a variety of equipment appropriate for patients with a wide range of functional ability. Referral to physiotherapy can be for issues around mobility, reduced activity or exercise tolerance, or symptom management. Patients who are ambulatory, willing to travel to the gym on a weekly basis, and perceive themselves as able to attend an hour-long session are encouraged to join a gym-based circuit class for weekly exercise intervention.
Exercise intervention
The circuits class is a rolling exercise programme over nine sessions, ideally on a weekly basis, conducted in groups of up to nine people. Each 1 hour class comprises a warm up, nine stations of exercise for approximately 3 minutes each, followed by a cool down and short educational talk. Topics for patient education are (a) strength stretching stamina and mobility, (b) balance and coordination, (c) home exercises, (d) fulfilling your potential, (e) breathing and pacing, and (f) falls prevention. The nine exercise stations cover a mixture of aerobic, resistance, and balance training as well as an element of fun; stair climbs, stationary cycling, treadmill walking, trampette bouncing or marching, overhead pulleys (with or without resistance), MOTOmed® arm bike, wall push ups, upper limb-free weights, and Nintendo Wii fitTM balance board. Patients are encouraged to exercise at moderate intensity with the instruction to ‘be able to talk but not sing’, ‘feel warmer’, or reach a modified Borg scale rating of 3–4. Patients are provided with a paper record to take round the circuits and self-record their performance. There is flexibility to modify or change the programme according to individual needs, for example, a patient who is unable or unwilling to manage the treadmill might replace that station with a sit-to-stand exercise using a chair. As far as possible though, patients are encouraged to complete the set circuit for continuity. Classes are offered every weekday and patients are encouraged to attend the same day each week where possible to maintain the group dynamic.
Measurements
Outcome measures were recorded at the start and end of the programme and took 10–20 minutes to complete in total. Patient reported measures were administered through questionnaires handed out by the rehabilitation team or posted to patients, and objective outcome measures were collected using simple physical tests administered by physiotherapists or a rehabilitation assistant who all received the same training in the use of the measures. For the purpose of this evaluation, basic demographic information was recorded at the date of the first class and attendance was recorded by the team member leading the group. As a clinical service undertaking assessments and providing care in line with national recommendations, formal ethics committee approval was not required.7 Approval was granted by the St Christopher's Research Committee.
Patient reported outcomes
Psychological well-being was assessed using the General Health Questionnaire (GHQ12), a 12-item measure focusing on the inability to carry out normal functions and the appearance of new and distressing experiences. Scores range from 0 to 36, with a higher score indicating greater level of physiological distress.8,9 Fatigue and health-related quality of life were assessed using the Functional Assessment of Chronic Illness Therapy (FACIT-F) which has physical, social, emotional, functional, and fatigue subscales. Scores for the Fatigue Subscale (FS) range from 0 to 52 and for quality of life range from 0 to 108, with higher scores indicating better quality of life and lower levels of fatigue.10 Patient satisfaction was assessed using questions from the Functional Assessment of Chronic Illness Therapy – Patient Satisfaction (FACIT-PS) questionnaire to explore perceptions of clinical explanations, trust, and overall experience. Permission was granted to modify the satisfaction questionnaire to ensure that selected questions pertained to the rehabilitation service and staff.
Performance-related outcomes
Physical function was measured using the short physical performance battery (SPPB), which tests balance, gait, and lower limb muscle function.11 Balance is tested in standing using side by side, semi-tandem and tandem stands, with a point scored for each position successfully held for 10 seconds or more. Gait speed is measured as the time taken to walk 4 m at a normal pace (with or without an aid). Lower limb muscle function is measured using the time taken to perform five sit-to-stand manoeuvres (5STS) from a chair without the use of the arms. As an indicator of global strength, hand grip strength was assessed in the preferred arm using a hand-held dynamometer.12 Patients were instructed to perform three maximum efforts over 2–3 seconds with verbal encouragement and the best of three attempts (kilograms; kg) was recorded.
Statistical analysis
Data were described by mean (standard deviation, SD) and median [inter-quartile range, IQR] as appropriate. Percentages with 95% confidence intervals (CI) were calculated for proportions of patients taking up the service on being approached and completing the programme. Student's t-test, Mann–Whitney U-tests of difference, or Pearson's chi-squared test were used as appropriate to compare for differences within patients pre- to post-programme and between those who completed the programme and those who did not. All calculations were performed using the Statistical Package for Social Sciences v18.0 and P values of <0.05 were regarded as statistically significant.
Results
Patient flow and demographics
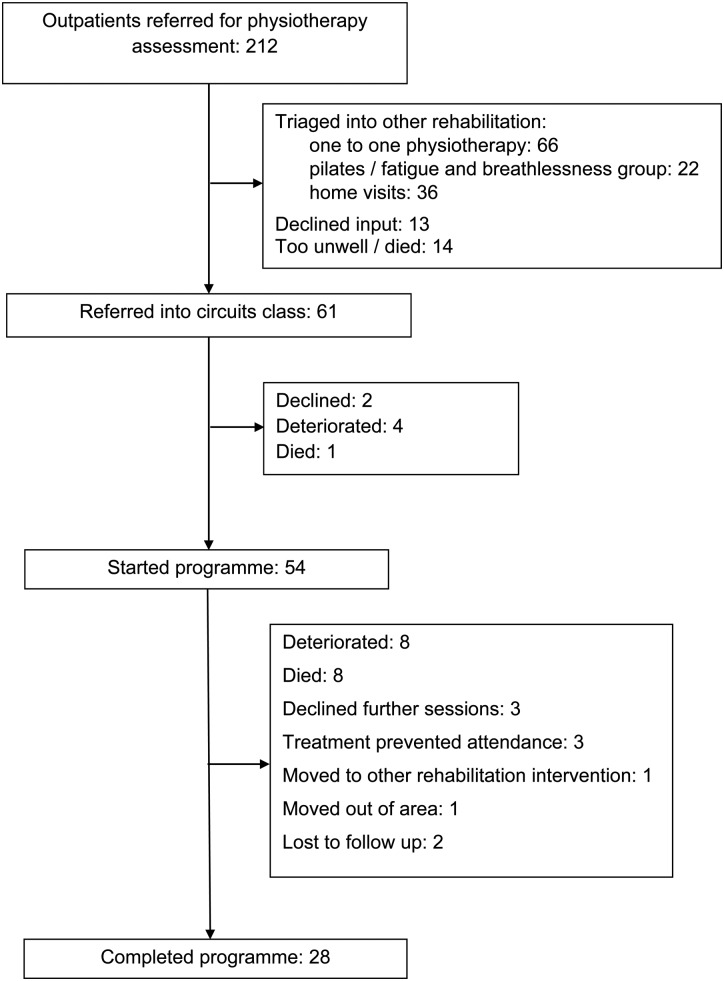
Between February and August 2013, a total of 212 outpatients were referred to the physiotherapy service for assessment. Of these, 61 were triaged into the circuits classes of whom 2 declined input, 4 deteriorated, and a further patient died prior to starting the programme (Fig. 1). The triaged group had a range of cancer and non-cancer diagnoses, one-third were non-Caucasian and one-quarter lived alone. As of 1 January 2014, nine patients referred to the programme had died (8%) with a median [IQR] survival of 67 [50–137] days (Table 1). Of the 54 patients who started the programme, 8 each deteriorated or died, and 3 each declined sessions or started treatment, and a further 4 patients did not complete the programme (Fig. 1). At the time of this evaluation, 28 patients (52%) who started the circuit classes completed the programme (Fig. 1). There were no statistical differences in age, gender, primary diagnosis, social status, or survival between those completing and not-completing the programme (Table 1).
Figure 1 .
Patient flow.
Table 1 .
Demographic and functional details of patients referred to circuit classes
| All patients | Completers | Non-completers | P value completers versus non-completers | |
|---|---|---|---|---|
| Number (%) | 61 (100) | 28 (46) | 33 (54) | |
| Gender: male, n (%) | 31 (51) | 13 (42) | 18 (58) | 0.53 |
| Mean (SD) age, years | 65 (14) | 66 (15) | 65 (13) | 0.61 |
| Primary diagnosis, n (%) | 0.52 | |||
| Cancer | ||||
| Lung | 9 (15) | 3 (11) | 6 (18) | |
| Breast | 7 (12) | 5 (18) | 2 (6) | |
| Upper gastroentestinal | 7 (12 | 3 (11) | 4 (13) | |
| 4 (7) | 1 (4) | 3 (9) | ||
| Urological | 13 (21) | 6 (21) | 7 (21) | |
| Gynaecological | 2 (3) | 1 (4) | 1 (3) | |
| Brain | 4 (7) | 2 (7) | 2 (6) | |
| Haematological | 6 (10) | 3 (11) | 3 (10) | |
| Unknown primary | 2 (3) | 1 (4) | 1 (3) | |
| Other | 3 (5) | 1 (6) | 2 (6) | |
| Non-cancer | ||||
| Cardiomyopathy | 1 (2) | 1 (4) | 0 (0) | |
| COPD | 1 (2) | 0 (0) | 1 (3) | |
| Interstitial lung disease | 1 (2) | 1 (4) | 0 (0) | |
| Alcoholic liver disease | 1 (2) | 0 (0) | 1 (3) | |
| Ethnic group, n (%) | 0.08 | |||
| White British | 36 (59) | 16 (57) | 20 (61) | |
| Other white | 3 (5) | 1 (4) | 2 (6) | |
| White Irish | 1 (2) | 1 (4) | 0 (0) | |
| Black Caribbean | 10 (16) | 2 (7) | 4 (12) | |
| Mixed white/black Caribbean | 1 (2) | 0 (0) | 1 (3) | |
| Indian | 2 (3) | 0 (0) | 2 (6) | |
| Black African | 3 (5) | 2 (7) | 1 (3) | |
| Chinese | 1 (2 | 0 (0) | 1 (3) | |
| Other Asian | 1 (2) | 1 (4) | 0 (0) | |
| Other | 1 (2) | 0 (0) | 1 (3) | |
| NS – not stated | 2 (3) | 1 (4) | 1 (3) | |
| Social status, n (%) | 0.15 | |||
| Living alone | 14 (23) | 7 (25) | 7 (21) | |
| Living with others | 47 (77) | 21 (75) | 26 (79) | |
| Physical function | ||||
| SPPB score | 8 [6–10] | 8 [6–10] | 9 [7–10] | 0.75 |
| Gait speed (m/s) | 0.63 (0.79) | 0.60 (0.87) | 0.66 (0.61) | 0.59 |
| Five sit-to-stand time (s) | 19.84 (13.90) | 20.52 (14.26) | 19.23 (13.81) | 0.76 |
| Unable to perform sit-to stand, n (%) | 10 (16) | 5 (18) | 5 (15) | |
| Grip strength (kg) | 24.78 (9.61) | 25.15 (8.62) | 24.44 (10.56) | 0.73 |
| Psychological well-being | ||||
| GHQ | 13 [7–17] | 13 [7–19] | 13 [8–17] | 0.99 |
| FACT-G | 70.9 (14.5) | 73.7 (13.7) | 68.6 (14.9) | 0.15 |
| Fatigue (FS) | 29.5 (10.9) | 32.0 (9.8) | 27.3 (11.5) | 0.11 |
| Survival (from first assessment) | ||||
| Days | 67 [50–137] | 143 [78–177] | 86 [58–115] | 0.09 |
| At 90 days, n (%) | 52 (85) | 28 (100) | 25 (76) | 0.41 |
Values are mean (SD) or median [IQR] unless specified otherwise.
Impact of gym class intervention
No adverse events associated with exercise were reported during the exercise classes throughout the evaluation period. In patients completing the circuit classes in full (n = 28), changes in measures of physical function were towards benefit with significant improvements in overall SPPB score, gait speed (mean difference [95% CI] 0.23 [0.03, 0.44] m/seconds, P = 0.03), five sit-to-stand time (−5.44 [−10.43, −0.46] seconds), P = 0.03), but not grip strength (0.65 [−1.39, 2.96] kg). Psychological well-being improved but not significantly (P = 0.08) and there were no apparent changes in quality-of-life sub-scales, overall scores or fatigue (Table 2).
Table 2 .
Absolute and percentage change in outcome measures in patients completing the circuit programme (n = 28)
| Pre-programme | Post-programme | Mean change [95% CI] | P value | |
|---|---|---|---|---|
| SPPB total score | 8 [6–10] | 8 [6–11] | – | 0.04 |
| Balance score | 4 [3–4] | 4 [3–4] | – | 0.57 |
| Gait speed (m/s) | 0.60 (0.87) | 0.72 (1.27) | 0.23 [0.03, 0.44] | 0.03 |
| Five sit-to-stand (s) | 20.52 (14.26) | 16.72 (5.97) | −5.44 [−10.43, −0.46] | 0.03 |
| Grip strength (kg) | 25.15 (8.62) | 26.10 (9.43) | 0.65 [−1.39, 2.96] | 0.52 |
| GHQ-12 | 13 [7–19] | 7 [6–11] | – | 0.08 |
| Physical well-being | 20.8 (5.0) | 20.7 (5.4) | 0.46 [−2.36, 1.34] | 0.62 |
| Social/family well-being | 21.8 (4.7) | 21.2 (5.2) | −0.64 [−2.06, 0.77] | 0.36 |
| Emotional well-being | 17.7 (4.6) | 17.9 (4.2) | −0.23 [−1.65, 2.12] | 0.78 |
| Functional well-being | 15.3 (5.2) | 14.6 (4.2) | −0.85 [−2.98, 1.27] | 0.41 |
| Fatigue subscale | 32.0 (9.8) | 32.7 (11.3) | 0.77 [−3.10, 4.64] | 0.68 |
| FACT-G | 73.7 (13.7) | 74.5 (11.7) | 0.62 [−4.91, 3.67] | 0.76 |
Values are mean (SD) or median [IQR] unless specified otherwise. Abbreviations: SPPB, short physical performance battery; GHQ12, General Health Questionnaire; FACIT-G, Functional Assessment of Chronic Illness Therapy.
Patient feedback
Feedback was obtained from patients completing the programme in full. All patients reported that the physiotherapist gave explanations they could understand and understood their needs. When asked if they had confidence in their physiotherapist and whether they trusted their suggestions, all but one reported ‘yes, completely’ and the remaining patient ‘yes, for the most part’. Overall, when asked how they rated the care they received half of the patients replied ‘excellent’ and the other ‘very good’. All respondents said they would recommend the group to others and would choose the group again. Free text comments were all positive and expressed gratitude, including: ‘The team have helped me a great deal’, ‘Good environment to be in and relaxing place to come to, easy to make friends’, ‘Kind and friendly, responsive to my personal needs and suggestions’, ‘I benefited hugely from the circuits, I gained confidence and fitness’.
Discussion
When evaluating an outpatient, hospice-based, circuit exercise programme in patients with advanced progressive illness in a ‘real-world’ setting, our main findings are that: (a) almost one-third referrals to physiotherapy are considered appropriate for this element of the rehabilitation service; (b) half of all patients that commence the programme do not complete nine sessions; (c) physical function and psychological well-being appear to be improved or maintained in the half that complete the programme; (d) feedback from patients is excellent and all would recommend the service to others. Our data also provide an indication of the elements and functioning of the service and the associated physiotherapy workload.
There are no directly comparable studies but others have examined similar programmes in the context of research. In a large randomized controlled trial (n = 231) Oldervoll and colleagues examined an 8-week, twice weekly, supervised centre-based aerobic and resistance circuit training programme offered to patients with advanced cancer.5 The exercise group demonstrated greater improvements in hand-grip strength, shuttle walk distance, and quality of life compared to the control group, whilst fatigue remained unchanged.5 There was a reasonable attrition rate given the population (∼35%) and a marked difference in survival between those completing and non-completing the programme (median 6.2 versus 16.3 months), which suggests that benefit was restricted to a select group of patients.13 Comparatively, our group of patients had cancer and non-cancer diagnoses, represented a wide range of ethnicities, and were all under hospice care with incurable disease and a limited life expectancy (median 2.3 months). Our programme was also less demanding with once as opposed to twice weekly sessions. Another recent study examined a broader rehabilitation approach incorporating a systematic assessment, psychological, and complementary therapies in people with advanced cancer using a goal-based intervention.14 The intervention reduced the unmet needs for support and was associated with a significant reduction in health service resource use in this group.14
This study adds to the evidence base examining the role of physical activity and exercise as an intervention for patients in the palliative care setting.4 We provide the first evaluation of an exercise-led clinical service in an unselected group of patients from a leading UK hospice. Our findings help support others developing services in this area. Almost one-third of referrals to our physiotherapy service were triaged into the circuit classes which enabled a small team (2.5 full-time physiotherapists and 1 therapy assistant) to offer regular contact to patients, with 310 face-to-face contacts over a period of 6 months. The majority of patients starting the programme did not complete it as described; nine sessions over 9 weeks. The clinical emphasis is on sessions, as opposed to weeks, and where patients could not attend, for example because of a hospital appointment, the timing of the programme was delayed to allow equity of access. As such, most patients took longer to finish (mean (range) duration 12 (9–23) weeks) which would have increased the likelihood of disease progression and could account for the high non-completion rate.
The emphasis placed on completion or non-completion is worth considering. In a clinical trial, completion is often a pre-requisite for outcome data and as such is viewed as a key marker of success.15 In contrast, a clinical service must adapt and be responsive to patients’ needs. There is often some apprehension about commencing exercise on the part of patients. The communication during the initial assessment of this service focuses on trying the classes out, taking a week at a time, reviewing how they feel after exercising, and re-evaluating over time. The emphasis is not on ‘finishing’ the programme, rather, exercise is promoted as an on-going opportunity. In line with this, patients who stop attending are offered one-to-one physiotherapy and patients who reach nine sessions are offered continued access to the gym. Whilst our outcome measures did not demonstrate change at the group level, patient satisfaction was high, and participation in group-based activities may be beneficial in the broadest sense. For example, they provide social interaction, a sense of accomplishment, peer support and motivation, education, information sharing, and may improve patient confidence, self-efficacy, adaption, or coping.16,17 This group support naturally evolves from a shared experience and, while encouraged by the physiotherapists, is primarily initiated and sustained by the patients.18 These aspects may be better explored by qualitative interviews, which we are currently conducting in this setting.
Nonetheless, services must still demonstrate their effectiveness and cost-effectiveness requiring assessment of outcome. When selecting our current outcome measures we screened tools on the basis of sound psychometric properties but thereafter focused on clinical utility. Our assessment battery could be completed in 10–20 minutes in total. The physical measures were easy to carry out, with a set space designated in the gym for them. Patients generally understood what they were for and responded positively to having physical attributes like strength and balance tested. Similarly, the brief psychological measures were not unduly burdensome for the majority and patients could appreciate why they were being asked to complete them. The questionnaires also provided an opportunity to explore psychological issues if appropriate and prompt onward referral to other professionals. More data to guide appropriate outcome selection in this field are required.
Limitations to this study include the uncontrolled nature of the intervention, which could mask an effect towards maintaining physical function and psychological well-being where it may have deteriorated. As such, outcome data in those completing the programme are primarily provided to inform work around the effectiveness of this type of intervention. Follow-up outcome data in non-completers may also have helped understand how this group differed from those completing the programme and the extent of the suspected deterioration. We did not capture feedback from those patients not completing the programme as this was not usual practice. Our impression was of a uniform level of satisfaction from session to session, but it would be useful to elicit the views of this group at the point of discontinuing exercise. Further, whilst we assessed a range of domains with our outcome measures, we did not explore symptom burden or relief, which may have been affected in the short term whilst exercising, and as a result of the programme.
These data provide a strong basis for further work. Given the gap between the excellent patient feedback and limited changes in physical function or quality of life, it would be worthwhile to explore the broader benefits of participation, for example, through patient interviews at various points through the programme. This would also provide an opportunity to explore the reasons for patients’ attending despite their open recognition of physical deterioration. The high non-completion rate could be addressed through the use of adjuncts which allow patients to benefit or get positive feedback in a shorter timeframe. For example, a goal setting element may be useful to shape exercises for the individual patients, or a group-based session to share achievements may encourage patients to verbalize their successes to enhance peer support. Finally, the role of home-based exercise needs unpicking in this population given recent reports of benefit and the preferences of some patients due to difficulties with time and travel demands.19,20
In conclusion, a hospice-based circuits class is one means to offer exercise to a range of patients with advanced progressive illness. Despite excellent feedback, only half of all patients completed the nine-session programme in full and evidence of benefit was limited. Future work should explore the broader benefits of group participation in this setting and whether delivering programmes, or elements of them, in shorter time frames is helpful.
Disclaimer statements
Contributors The original study conception was by HTR & MM. HTR, LM, KN, AJ, KL, GP & DM contributed to data acquisition. HTR, LM, KM, AJ, KL, GP & DM undertook the initial analysis of data which was then reviewed by HTR & MM. HTR & MM produced a first draft of the manuscript. All authors critically revised the manuscript and approved the submitted version.
Funding St Christopher's Hospice.
Conflict-of-Interest None.
Ethics Approval None.
Acknowledgements
This work was supported by funding from the Executive Committee at St Christopher's Hospice, who had no role in the study design, collection, analysis and interpretation of data, or decision to submit the manuscript for publication. Dr Matthew Maddocks is funded by an NIHR Post-Doctoral Fellowship award. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1.Lacasse Y, Goldstein R, Lasserson T, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;4(4):CD003793. [DOI] [PubMed] [Google Scholar]
- 2.Rees K, Taylor RR, Singh S, Coats AJ, Ebrahim S. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev 2004. (3):CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knols R, Aaronson NK, Uebelhart D, Fransen J, Aufdemkampe G. Physical exercise in cancer patients during and after medical treatment: a systematic review of randomized and controlled clinical trials. J Clin Oncol 2005;23(16):3830–42. [DOI] [PubMed] [Google Scholar]
- 4.Lowe SS, Watanabe SM, Courneya KS. Physical activity as a supportive care intervention in palliative cancer patients: a systematic review. J Support Oncol 2009;7(1):27–34. [PubMed] [Google Scholar]
- 5.Oldervoll LM, Loge JH, Lydersen S, Paltiel H, Asp MB, Nygaard UV, et al. Physical exercise for cancer patients with advanced disease: a randomized controlled trial. Oncologist 2011;16(11):1649–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly CM, Lowe-Strong A, Rankin JP, Campbell A, Allen JM, Gracey JH. Physiotherapy management of cancer-related fatigue: a survey of UK current practice. Support Care Cancer 2010;18(7):817–25. [DOI] [PubMed] [Google Scholar]
- 7.Service NRE. Defining research: NRES guidance to help you decide if your project requires review by a research ethics committee. London: Health Research Authority 2013. [Google Scholar]
- 8.Goldberg DP, Gater R, Sartorius N, Ustun T, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27(01):191–7. [DOI] [PubMed] [Google Scholar]
- 9.Gao W, Bennett MI, Stark D, Murray S, Higginson IJ. Psychological distress in cancer from survivorship to end of life care: prevalence, associated factors and clinical implications. Eur J Cancer 2010;46(11):2036–44. [DOI] [PubMed] [Google Scholar]
- 10.Cella D, Eton DT, Lai J-S, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage 2002;24(6):547–61. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49(2):M85–94. [DOI] [PubMed] [Google Scholar]
- 12.Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, et al. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing 2011;40(4):423–9. [DOI] [PubMed] [Google Scholar]
- 13.Maddocks M, Mockett S, Wilcock A. Is exercise an acceptable and practical therapy for people with or cured of cancer? A systematic review. Cancer Treat Rev 2009;35(4):383–90. [DOI] [PubMed] [Google Scholar]
- 14.Jones L, Fitzgerald G, Leurent B, Round J, Eades J, Davis S, et al. Rehabilitation in advanced, progressive, recurrent cancer: a randomized controlled trial. J Pain Symptom Manage 2013;46(3):315–325. [DOI] [PubMed] [Google Scholar]
- 15.Higginson IJ, Evans CJ, Grande G, Preston N, Morgan M, McCrone P, et al. Evaluating complex interventions in end of life care: the MORECare Statement on good practice generated by a synthesis of transparent expert consultations and systematic reviews. BMC Med 2013;11(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paltiel H, Solvoll E, Loge JH, Kaasa S, Oldervoll L. ‘The healthy me appears’: palliative cancer patients’ experiences of participation in a physical group exercise program. Palliat Support Care 2009;7(4):459. [DOI] [PubMed] [Google Scholar]
- 17.Midtgaard J, Rorth M, Stelter R, Adamsen L. The group matters: an explorative study of group cohesion and quality of life in cancer patients participating in physical exercise intervention during treatment. Eur J Cancer Care 2006;15(1):25–33. [DOI] [PubMed] [Google Scholar]
- 18.Midtgaard J, Stelter R, Rorth M, Adamsen L. Regaining a sense of agency and shared self-reliance: the experience of advanced disease cancer patients participating in a multidimensional exercise intervention while undergoing chemotherapy – analysis of patient diaries. Scand J Psychol 2007;48(2):181–90. [DOI] [PubMed] [Google Scholar]
- 19.Maddocks M, Armstrong S, Wilcock A. Exercise as a supportive therapy in incurable cancer: exploring patient preferences. Psycho-Oncology 2011;20(2):173–8. [DOI] [PubMed] [Google Scholar]
- 20.Cheville AL, Kollasch J, Vandenberg J, Shen T, Grothey A, Gamble G, et al. A home-based exercise program to improve function, fatigue, and sleep quality in patients with stage IV lung and colorectal cancer: a randomized controlled trial. J Pain Symptom Manage 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]