Abstract
Purpose
The individual fall risk of a patient is often multifactorial. Polymedication contributes to an additional risk of fall-risk-increasing adverse reactions (FRIARs). Previous studies have not sufficiently investigated the complexity facing prescribers when balancing the therapeutic benefits of individual drugs against their potential fall risk.
Methods
An expert panel identified drugs with FRIARs based on the Summary of Product Characteristics (SmPC). These FRIARs and other parameters (such as the total number of drugs, dosage, dose adjustments, and drug changes) were then analyzed for their impact on falls in a case-control study using logistic regression.
Results
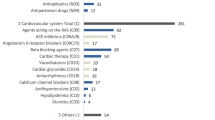
During a 1-year period, 112 (1%) of 11,481 hospital patients experienced at least one fall event. Complete data was available for evaluation from 87 of them (case group). We matched these patients to another 87 patients who had no fall events (control group). FRIAR drugs were more frequently prescribed in the case group (4.26 (Q25–Q75, 3.75–4.78) per patient; p = 0.033) than in the control group (3.48 (2.97–3.99)). Drugs with FRIARs (β = 0.137; p = 0.035) and the total number of FRIARs (β = 0.033; p = 0.031) increased the fall risk. The total number of drugs, dosage, dose adjustments, and drug changes showed no influence.
Conclusions
FRIARs were associated with a higher number of falls. To consider FRIARs offers a chance to address the complexity of the individual medication. This data can support future computerized physician order entries with clinical decision support.
Similar content being viewed by others
References
Schwendimann R, Bühler H, de Geest S, Milisen K (2008) Characteristics of hospital inpatient falls across clinical departments. Gerontology 54:342–348. https://doi.org/10.1159/000129954
Gale CR, Cooper C, Aihie Sayer A (2016) Prevalence and risk factors for falls in older men and women: the English Longitudinal Study of Ageing. Age Ageing 45:789–794
Talbot LA, Musiol RJ, Witham EK, Metter EJ (2005) Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 5:86
Blain H, Masud T, Dargent-Molina P, Martin FC, Rosendahl E, van der Velde N, Bousquet J, Benetos A, Cooper C, Kanis JA, Reginster JY, Rizzoli R, Cortet B, Barbagallo M, Dreinhöfer KE, Vellas B, Maggi S, Strandberg T, EUGMS Falls and Fracture Interest Group, IAGG-ER, EUMS, FFN, ESCEO, IOF (2016) A comprehensive fracture prevention strategy in older adults: the European Union Geriatric Medicine Society (EUGMS) statement. Aging Clin Exp Res 28(4):797–803. https://doi.org/10.1007/s40520-016-0588-4
Verma SK, Willetts JL, Corns HL, Marucci-Wellman HR, Lombardi DA, Courtney TK (2016) Falls and fall-related injuries among community-dwelling adults in the United States. PLoS One 11(3):e0150939. https://doi.org/10.1371/journal.pone.0150939
Scuffham P, Chaplin S, Legood R (2003) Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health 57(9):740–744
Auais M, Alvarado BE, Curcio CL, Garcia A, Ylli A, Deshpande N (2016) Fear of falling as a risk factor of mobility disability in older people at five diverse sites of the IMIAS study. Arch Gerontol Geriatr 66:147–153. https://doi.org/10.1016/j.archger.2016.05.012
Iliffe S, Kharicha K, Harari D, Swift C, Gillmann G, Stuck AE (2007) Health risk appraisal in older people 2: the implications for clinicians and commissioners of social isolation risk in older people. Br J Gen Pract 57(537):277–282
Abdel-Rahman EM, Yan G, Turgut F, Balogun RA (2011) Long-term morbidity and mortality related to falls in hemodialysis patients: role of age and gender - a pilot study. Nephron Clin Pract 118(3):c278–c284. https://doi.org/10.1159/000322275
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, Kerse N (2012) Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 12(12):CD005465. https://doi.org/10.1002/14651858.CD005465.pub3
de Jong MR, Van der Elst M, Hartholt KA (2013) Drug-related falls in older patients: implicated drugs, consequences, and possible prevention strategies. Ther Adv Drug Saf 4:147–154. https://doi.org/10.1177/2042098613486829
Lee JY, Holbrook A (2017) The efficacy of fall-risk-increasing drug (FRID) withdrawal for the prevention of falls and fall-related complications: protocol for a systematic review and meta-analysis. Syst Rev 6(1):33. https://doi.org/10.1186/s13643-017-0426-6
Kragh Ekstam A, Elmståhl S (2016) Do fall-risk-increasing drugs have an impact on mortality in older hip fracture patients? A population-based cohort study. Clin Interv Aging 11:489–496. https://doi.org/10.2147/CIA.S101832
de Groot MH, van Campen JP, Moek MA, Tulner LR, Beijnen JH, Lamoth CJ (2013) The effects of fall-risk-increasing drugs on postural control: a literature review. Drugs Aging 30(11):901–920. https://doi.org/10.1007/s40266-013-0113-9
Milos V, Bondesson Å, Magnusson M, Jakobsson U, Westerlund T, Midlöv P (2014) Fall risk-increasing drugs and falls: a cross-sectional study among elderly patients in primary care. BMC Geriatr 27(14):40. https://doi.org/10.1186/1471-2318-14-40
Rojas-Fernandez C, Dadfar F, Wong A, Brown SG (2015) Use of fall risk increasing drugs in residents of retirement villages: a pilot study of long term care and retirement home residents in Ontario, Canada. BMC Res Notes 8:568. https://doi.org/10.1186/s13104-015-1557-2
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH (2013) The risk of falls on initiation of antihypertensive drugs in the elderly. Osteoporos Int 24(10):2649–2657. https://doi.org/10.1007/s00198-013-2369-7
Ensrud KE, Blackwell TL, Mangione CM, Bowman PJ, Whooley MA, Bauer DC, Schwartz AV, Hanlon JT, Nevitt MC, Study of Osteoporotic Fractures Research Group (2002) Central nervous system-active medications and risk for falls in older women. J Am Geriatr Soc 50(10):1629–1637
Hill KD, Wee R (2012) Psychotropic drug-induced falls in older people: a review of interventions aimed at reducing the problem. Drugs Aging 29(1):15–30. https://doi.org/10.2165/11598420-000000000-00000
Kerse N, Flicker L, Pfaff JJ, Draper B, Lautenschlager NT, Sim M, Snowdon J, Almeida OP (2008) Falls, depression and antidepressants in later life: a large primary care appraisal. PLoS One 3:e2423. https://doi.org/10.1371/journal.pone.0002423
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 47(1):30–39
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc 47(1):40–50
Préville M, Hébert R, Boyer R, Bravo G (2001) Correlates of psychotropic drug use in the elderly compared to adults aged 18-64: results from the Quebec health survey. Aging Ment Health 5(3):216–224
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, Marra CA (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960. https://doi.org/10.1001/archinternmed.2009.357
American Geriatrics Society 2015 Beers Criteria Update Expert Panel (2015) American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 63(11):2227–2246. https://doi.org/10.1111/jgs.13702
Pohl-Dernick K, Meier F, Maas R, Schöffski O, Emmert M (2016) Potentially inappropriate medication in the elderly in Germany: an economic appraisal of the PRISCUS list. BMC Health Serv Res 16:109. https://doi.org/10.1186/s12913-016-1366-x
Holt S, Schmiedl S, Thürmann PA (2011) Priscus list – potentially inadequate medication for the elderly. IOP Publishing PhysicsWeb. http://priscus.net/download/PRISCUS-Liste_PRISCUS-TP3_2011.pdf. Accessed 20 June 2018
Renom-Guiteras A, Meyer G, Thürmann PA (2015) The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol 71(7):861–875. https://doi.org/10.1007/s00228-015-1860-9
Darowski A, Chambers SA, Chambers DJ (2009) Antidepressants and falls in the elderly. Drugs Aging 26(5):381–394. https://doi.org/10.2165/00002512-200926050-00002
Souchet E, Lapeyre-Mestre M, Montastruc JL (2005) Drug related falls: a study in the French pharmacovigilance database. Pharmacoepidemiol Drug Saf 14(1):11–16
Campbell N, Boustani M, Limbil T, Ott C, Fox C, Maidment I, Schubert CC, Munger S, Fick D, Miller D, Gulati R (2009) The cognitive impact of anticholinergics: a clinical review. Clin Interv Aging 4:225–233
Ciorba A, Bianchini C, Scanelli G, Pala M, Zurlo A, Aimoni C (2017) The impact of dizziness on quality-of-life in the elderly. Eur Arch Otorhinolaryngol 274(3):1245–1250. https://doi.org/10.1007/s00405-016-4222-z
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R (2012) Medication-related falls in the elderly: causative factors and preventive strategies. Drugs Aging 29(5):359–376. https://doi.org/10.2165/11599460-000000000-00000
Haefeli WE (2018) Dosing – dose adjustment of renal eliminated drugs in patients with renal insufficiency. IOP Publishing PhysicsWeb. http://dosing.de Accessed 20 June 2018
Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL (1990) Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 19(2):136–141
Bennett A, Gnjidic D, Gillett M, Carroll P, Matthews S, Johnell K, Fastbom J, Hilmer S (2014) Prevalence and impact of fall-risk-increasing drugs, polypharmacy, and drug-drug interactions in robust versus frail hospitalised falls patients: a prospective cohort study. Drugs Aging 31(3):225–232. https://doi.org/10.1007/s40266-013-0151-3
Park H, Satoh H, Miki A, Urushihara H, Sawada Y (2015) Medications associated with falls in older people: systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol 71(12):1429–1440. https://doi.org/10.1007/s00228-015-1955-3
Church S, Robinson TN, Angles EM, Tran ZV, Wallace JI (2011) Postoperative falls in the acute hospital setting: characteristics, risk factors, and outcomes in males. Am J Surg 201(2):197–202. https://doi.org/10.1016/j.amjsurg.2009.12.013
Stel VS, Pluijm SM, Deeg DJ, Smit JH, Bouter LM, Lips P (2003) A classification tree for predicting recurrent falling in community-dwelling older persons. J Am Geriatr Soc 51(10):1356–1364
Bates DW, Pruess K, Souney P, Platt R (1995) Serious falls in hospitalized patients: correlates and resource utilization. Am J Med 99(2):137–143
Iihara N, Bando Y, Ohara M, Yoshida T, Nishio T, Okada T, Kirino Y (2016) Polypharmacy of medications and fall-related fractures in older people in Japan: a comparison between driving-prohibited and driving-cautioned medications. J Clin Pharm Ther 41(3):273–278
Callisaya ML, Sharman JE, Close J, Lord SR, Srikanth VK (2014) Greater daily defined dose of antihypertensive medication increases the risk of falls in older people--a population-based study. J Am Geriatr Soc 62:1527–1533. https://doi.org/10.1111/jgs.12925
Chen Y, Zhu LL, Zhou Q (2014) Effects of drug pharmacokinetic/pharmacodynamic properties, characteristics of medication use, and relevant pharmacological interventions on fall risk in elderly patients. Ther Clin Risk Manag 10:437–448. https://doi.org/10.2147/TCRM.S63756
Sterke CS, Ziere G, van Beeck EF, Looman CW, van der Cammen TJ (2012) Dose-response relationship between selective serotonin re-uptake inhibitors and injurious falls: a study in nursing home residents with dementia. Br J Clin Pharmacol 73(5):812–820. https://doi.org/10.1111/j.1365-2125.2011.04124.x
Herr M, Sirven N, Grondin H, Pichetti S, Sermet C (2017) Frailty, polypharmacy, and potentially inappropriate medications in old people: findings in a representative sample of the French population. Eur J Clin Pharmacol 73(9):1165–1172. https://doi.org/10.1007/s00228-017-2276-5
Acknowledgments
We thank all physicians and nurses in the participating departments for their helpful support in this study and Professor Benjamin R. Auer, Ph.D., for statistical guidance and Katharine Worthington, Jena M. Gaines, and Professor Astrid Bertsche, M.D., for language editing.
Funding
This study was financed by the institutions as mentioned above and was performed without third party funding.
Author information
Authors and Affiliations
Contributions
Susanne Schiek contributed to the study conception, analyzed and interpreted the data, and wrote the manuscript.
Katja Hildebrandt contributed to the study conception, collected and analyzed the data, and revised the manuscript.
Olaf Zube initiated the study, contributed to the study conception, and revised the manuscript.
Thilo Bertsche contributed to the study conception, interpreted the data, and wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study (retrospective case-control study), formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 227 kb)
Rights and permissions
About this article
Cite this article
Schiek, S., Hildebrandt, K., Zube, O. et al. Fall-risk-increasing adverse reactions—is there value in easily accessible drug information? A case-control study. Eur J Clin Pharmacol 75, 849–857 (2019). https://doi.org/10.1007/s00228-019-02628-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02628-x