Abstract
Advanced prostate and bladder cancer are two outstanding unmet medical needs for urological oncologists. The high prevalence of these tumours, lack of effective biomarkers and limited effective treatment options highlight the importance of basic research in these diseases. Galectins are a family of β-galactoside-binding proteins that are frequently altered (upregulated or downregulated) in a wide range of tumours and have roles in different stages of tumour development and progression, including immune evasion. In particular, altered expression levels of different members of the galectin family have been reported in prostate and bladder cancers, which, together with the aberrant glycosylation patterns found in tumour cells and the constituent cell types of the tumour microenvironment, can result in malignant transformation and tumour progression. Understanding the roles of galectin family proteins in the development and progression of prostate and bladder cancer could yield key insights to inform the clinical management of these diseases.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 68, 7–30 (2018).
Risbridger, G. P., Toivanen, R. & Taylor, R. A. Preclinical models of prostate cancer: patient-derived xenografts, organoids, and other explant models. Cold Spring Harb. Perspect. Med. 8, a030536 (2018).
Fizazi, K. et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N. Engl. J. Med. 377, 352–360 (2017).
James, N. D. et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N. Engl. J. Med. 377, 338–351 (2017).
Shipley, W. U. et al. Radiation with or without antiandrogen therapy in recurrent prostate cancer. N. Engl. J. Med. 376, 417–428 (2017).
Sathianathen, N. J., Konety, B. R., Crook, J., Saad, F. & Lawrentschuk, N. Landmarks in prostate cancer. Nat. Rev. Urol. 15, 627–642 (2018).
Cotter, K. A. & Rubin, M. A. Sequence of events in prostate cancer. Nature 560, 557–559 (2018).
Arriaga, J. M. & Abate-Shen, C. Genetically engineered mouse models of prostate cancer in the postgenomic era. Cold Spring Harb. Perspect. Med. 9, a030528 (2019).
van der Toom, E. E. et al. Prostate-specific markers to identify rare prostate cancer cells in liquid biopsies. Nat. Rev. Urol. 16, 7–22 (2019).
Sved, P. D., Gomez, P., Manoharan, M., Kim, S. S. & Soloway, M. S. Limitations of biopsy Gleason grade: implications for counseling patients with biopsy Gleason score 6 prostate cancer. J. Urol. 172, 98–102 (2004).
Cohen, M. S. et al. Comparing the Gleason Prostate Biopsy and Gleason Prostatectomy Grading System: The Lahey Clinic Medical Center experience and an international meta-analysis. Eur. Urol. 54, 371–381 (2008).
Baciarello, G., Gizzi, M. & Fizazi, K. Advancing therapies in metastatic castration-resistant prostate cancer. Expert Opin. Pharmacother. 19, 1797–1804 (2018).
Xu, J. X. et al. FDA approval summary: nivolumab in advanced renal cell carcinoma after anti-angiogenic therapy and exploratory predictive biomarker analysis. Oncologist 22, 311–317 (2017).
Powles, T. et al. Updated European Association of Urology Guidelines recommendations for the treatment of first-line metastatic clear cell renal cancer. Eur. Urol. 73, 311–315 (2017).
Bellmunt, J. et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N. Engl. J. Med. 376, 1015–1026 (2017).
Balar, A. V. et al. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): a multicentre, single-arm, phase 2 study. Lancet Oncol. 18, 1483–1492 (2017).
Siefker-Radtke, A. & Curti, B. Immunotherapy in metastatic urothelial carcinoma: focus on immune checkpoint inhibition. Nat. Rev. Urol. 15, 112–124 (2017).
Carlo, M. I., Voss, M. H. & Motzer, R. J. Checkpoint inhibitors and other novel immunotherapies for advanced renal cell carcinoma. Nat. Rev. Urol. 13, 420–431 (2016).
Maia, M. C. & Hansen, A. R. A comprehensive review of immunotherapies in prostate cancer. Crit. Rev. Oncol. Hematol. 113, 292–303 (2017).
Matsumoto, K. et al. Late recurrence and progression in non-muscle–invasive bladder cancers after 5-year tumor-free periods. Urology 75, 1385–1390 (2010).
Tabayoyong, W. B. et al. Systematic review on the utilization of maintenance intravesical chemotherapy in the management of non-muscle-invasive bladder cancer. Eur. Urol. Focus 4, 512–521 (2018).
Türkölmez, K., Tokgöz, H., Reşorlu, B., Köse, K. & Bedük, Y. Muscle-invasive bladder cancer: predictive factors and prognostic difference between primary and progressive tumors. Urology 70, 477–481 (2007).
Marcq, G. et al. Contemporary best practice in the use of neoadjuvant chemotherapy in muscle-invasive bladder cancer. Ther. Adv. Urol. 11, 175628721882367 (2019).
Rodriguez-Vida, A., Perez-Gracia, J. L. & Bellmunt, J. Immunotherapy combinations and sequences in urothelial cancer: facts and hopes. Clin. Cancer Res. 24, 6115–6124 (2018).
Anastasiadis, A. & de Reijke, T. M. Best practice in the treatment of nonmuscle invasive bladder cancer. Ther. Adv. Urol. 4, 13–32 (2012).
Canesin, G. et al. Galectin-3 expression is associated with bladder cancer progression and clinical outcome. Tumour Biol. 31, 277–285 (2010).
Sakaki, M. et al. Serum level of galectin-3 in human bladder cancer. J. Med. Invest. 55, 127–132 (2008).
Balan, V. et al. Galectin-3: a possible complementary marker to the PSA blood test. Onco_target 4, 542–549 (2013).
Wang, Y. et al. The significance of galectin-3 as a new basal cell marker in prostate cancer. Cell Death Dis. 4, e753 (2013).
Ahmed, H., Cappello, F., Rodolico, V. & Vasta, G. R. Evidence of heavy methylation in the galectin 3 promoter in early stages of prostate adenocarcinoma: development and validation of a methylated marker for early diagnosis of prostate cancer. Transl Oncol. 2, 146–156 (2009).
Wu, T.-F. et al. Galectin-1 dysregulation independently predicts disease specific survival in bladder urothelial carcinoma. J. Urol. 193, 1002–1008 (2015).
Kramer, M. W. et al. Decreased expression of galectin-3 predicts tumour recurrence in pTa bladder cancer. Oncol. Rep. 20, 1403–1408 (2008).
Langbein, S. et al. Gene-expression signature of adhesion/growth-regulatory tissue lectins (galectins) in transitional cell cancer and its prognostic relevance. Histopathology 51, 681–690 (2007).
Wu, M.-M. et al. Promoter hypermethylation of LGALS4 correlates with poor prognosis in patients with urothelial carcinoma. Onco_target 8, 23787–23802 (2017).
Liu, Y. et al. Galectin-9 as a prognostic and predictive biomarker in bladder urothelial carcinoma. Urol. Oncol. 35, 349–355 (2017).
Cummings, R. D., Liu, F.-T. & Vasta, G. R. in Essentials of Glycobiology [Internet] 3rd edn Ch. 36 (eds Varki, A. et al.) (Cold Spring Harbor Laboratory Press, 2017).
Tsai, C.-M. et al. Galectin-1 and galectin-8 have redundant roles in promoting plasma cell formation. J. Immunol. 187, 1643–1652 (2011).
Tribulatti, M. V., Figini, M. G., Carabelli, J., Cattaneo, V. & Campetella, O. Redundant and antagonistic functions of galectin-1, -3, and -8 in the elicitation of T cell responses. J. Immunol. 188, 2991–2999 (2012).
Vyakarnam, A., Dagher, S. F., Wang, J. L. & Patterson, R. J. Evidence for a role for galectin-1 in pre-mRNA splicing. Mol. Cell. Biol. 17, 4730–4737 (1997).
Munkley, J., Mills, I. G. & Elliott, D. J. The role of glycans in the development and progression of prostate cancer. Nat. Rev. Urol. 13, 324–333 (2016).
Ohyama, C. Glycosylation in bladder cancer. Int. J. Clin. Oncol. 13, 308–313 (2008).
Stowell, S. R., Ju, T. & Cummings, R. D. Protein glycosylation in cancer. Annu. Rev. Pathol. 10, 473–510 (2015).
Pinho, S. S. & Reis, C. A. Glycosylation in cancer: mechanisms and clinical implications. Nat. Rev. Cancer 15, 540–555 (2015).
Rabinovich, G. A. & Croci, D. O. Regulatory circuits mediated by lectin-glycan interactions in autoimmunity and cancer. Immunity 36, 322–335 (2012).
Croci, D. O. et al. Glycosylation-dependent lectin-receptor interactions preserve angiogenesis in anti-VEGF refractory tumors. Cell 156, 744–758 (2014).
Kasbaoui, L., Harb, J., Bernard, S. & Meflah, K. Differences in glycosylation state of fibronectin from two rat colon carcinoma cell lines in relation to tumoral progressiveness. Cancer Res. 49, 5317–5322 (1989).
Hakomori, S. & Kannagi, R. Glycosphingolipids as tumor-associated and differentiation markers. J. Natl Cancer Inst. 71, 231–251 (1983).
Varki, A., Kannagi, R., Toole, B. & Stanley, P. in Essentials of Glycobiology [Internet] 3rd edn Ch. 47 (eds Varki, A. et al.) (Cold Spring Harbor Laboratory Press, 2017).
Ihara, S. et al. Prometastatic effect of N-acetylglucosaminyltransferase V is due to modification and stabilization of active matriptase by adding beta 1–6 GlcNAc branching. J. Biol. Chem. 277, 16960–16967 (2002).
Seidenfaden, R., Krauter, A., Schertzinger, F., Gerardy-Schahn, R. & Hildebrandt, H. Polysialic acid directs tumor cell growth by controlling heterophilic neural cell adhesion molecule interactions. Mol. Cell. Biol. 23, 5908–5918 (2003).
English, N. M., Lesley, J. F. & Hyman, R. Site-specific de-N-glycosylation of CD44 can activate hyaluronan binding, and CD44 activation states show distinct threshold densities for hyaluronan binding. Cancer Res. 58, 3736–3742 (1998).
Marsico, G., Russo, L., Quondamatteo, F. & Pandit, A. Glycosylation and integrin regulation in cancer. Trends Cancer 4, 537–552 (2018).
Lavrsen, K. et al. Aberrantly glycosylated MUC1 is expressed on the surface of breast cancer cells and a _target for antibody-dependent cell-mediated cytotoxicity. Glycoconj. J. 30, 227–236 (2013).
Drake, R. R., Jones, E. E., Powers, T. W. & Nyalwidhe, J. O. Altered glycosylation in prostate cancer. Adv. Cancer Res. 126, 345–382 (2015).
Llop, E. et al. Improvement of prostate cancer diagnosis by detecting PSA glycosylation-specific changes. Theranostics 6, 1190–1204 (2016).
Tanaka, T. et al. Aberrant N-glycosylation profile of serum immunoglobulins is a diagnostic biomarker of urothelial carcinomas. Int. J. Mol. Sci. 18, 2632 (2017).
Peracaula, R. et al. Altered glycosylation pattern allows the distinction between prostate-specific antigen (PSA) from normal and tumor origins. Glycobiology 13, 457–470 (2003).
Tabarés, G. et al. Different glycan structures in prostate-specific antigen from prostate cancer sera in relation to seminal plasma PSA. Glycobiology 16, 132–145 (2006).
Jia, G. et al. Alterations in expressed prostate secretion-urine PSA N-glycosylation discriminate prostate cancer from benign prostate hyperplasia. Onco_target 8, 76987–76999 (2017).
Dal Moro, F., Valotto, C., Guttilla, A. & Zattoni, F. Urinary markers in the everyday diagnosis of bladder cancer. Urol. J. 80, 265–275 (2013).
Hautmann, S. H. et al. Hyaluronic acid and hyaluronidase. 2 new bladder carcinoma markers [German]. Urologe. A 40, 121–126 (2001).
Cerliani, J. P., Blidner, A. G., Toscano, M. A., Croci, D. O. & Rabinovich, G. A. Translating the ‘sugar code’ into immune and vascular signaling programs. Trends Biochem. Sci. 42, 255–273 (2017).
Hirabayashi, J. & Kasai, K. The family of metazoan metal-independent beta-galactoside-binding lectins: structure, function and molecular evolution. Glycobiology 3, 297–304 (1993).
Di Lella, S. et al. When galectins recognize glycans: from biochemistry to physiology and back again. Biochemistry 50, 7842–7857 (2011).
Hirabayashi, J. et al. Oligosaccharide specificity of galectins: a search by frontal affinity chromatography. Biochim. Biophys. Acta 1572, 232–254 (2002).
Stowell, S. R. et al. Galectin-1, -2, and -3 exhibit differential recognition of sialylated glycans and blood group antigens. J. Biol. Chem. 283, 10109–10123 (2008).
Greenspan, N. S. Dimensions of antigen recognition and levels of immunological specificity. Adv. Cancer Res. 80, 147–187 (2001).
Rabinovich, G. A., Toscano, M. A., Jackson, S. S. & Vasta, G. R. Functions of cell surface galectin-glycoprotein lattices. Curr. Opin. Struct. Biol. 17, 513–520 (2007).
Stowell, S. R. et al. Ligand reduces galectin-1 sensitivity to oxidative inactivation by enhancing dimer formation. J. Biol. Chem. 284, 4989–4999 (2009).
Leppanen, A., Stowell, S., Blixt, O. & Cummings, R. D. Dimeric galectin-1 binds with high affinity to alpha2,3-sialylated and non-sialylated terminal N-acetyllactosamine units on surface-bound extended glycans. J. Biol. Chem. 280, 5549–5562 (2005).
Paz, A., Haklai, R., Elad-Sfadia, G., Ballan, E. & Kloog, Y. Galectin-1 binds oncogenic H-Ras to mediate Ras membrane anchorage and cell transformation. Oncogene 20, 7486–7493 (2001).
Elad-Sfadia, G., Haklai, R., Balan, E. & Kloog, Y. Galectin-3 augments K-Ras activation and triggers a Ras signal that attenuates ERK but not phosphoinositide 3-kinase activity. J. Biol. Chem. 279, 34922–34930 (2004).
Salomonsson, E. et al. Monovalent interactions of galectin-1. Biochemistry 49, 9518–9532 (2010).
Camby, I., Le Mercier, M., Lefranc, F. & Kiss, R. Galectin-1: a small protein with major functions. Glycobiology 16, 137R–157R (2006).
Voss, P. G. et al. Dissociation of the carbohydrate-binding and splicing activities of galectin-1. Arch. Biochem. Biophys. 478, 18–25 (2008).
Hughes, R. C. Secretion of the galectin family of mammalian carbohydrate-binding proteins. Biochim. Biophys. Acta 1473, 172–185 (1999).
Leffler, H., Carlsson, S., Hedlund, M., Qian, Y. & Poirier, F. Introduction to galectins. Glycoconj. J. 19, 433–440 (2004).
Compagno, D. et al. Galectins: major signaling modulators inside and outside the cell. Curr. Mol. Med. 14, 630–651 (2014).
Balan, V., Nangia-Makker, P. & Raz, A. Galectins as cancer biomarkers. Cancers (Basel). 2 592–610 (2010).
Jones, J. L. et al. Galectin-3 is associated with prostasomes in human semen. Glycoconj. J. 27, 227–236 (2010).
Thijssen, V. L., Heusschen, R., Caers, J. & Griffioen, A. W. Galectin expression in cancer diagnosis and prognosis: a systematic review. Biochim. Biophys. Acta 1855, 235–247 (2015).
Thijssen, V. L. et al. Tumor cells secrete galectin-1 to enhance endothelial cell activity. Cancer Res. 70, 6216–6224 (2010).
Manzi, M. et al. Galectin-1 controls the proliferation and migration of liver sinusoidal endothelial cells and their interaction with hepatocarcinoma cells. J. Cell. Physiol. 231, 1522–1533 (2016).
Yamaoka, K. et al. Expression of galectin-1 mRNA correlates with the malignant potential of human gliomas and expression of antisense galectin-1 inhibits the growth of 9 glioma cells. J. Neurosci. Res. 59, 722–730 (2000).
Orozco, C. A. et al. _targeting galectin-1 inhibits pancreatic cancer progression by modulating tumor–stroma crosstalk. Proc. Natl Acad. Sci. USA 115, E3769–E3778 (2018).
Rabinovich, G. A. et al. Specific inhibition of T cell adhesion to extracellular matrix and proinflammatory cytokine secretion by human recombinant galectin-1. Immunology 97, 100–106 (1999).
Rabinovich, G. A., Toscano, M. A., Ilarregui, J. M. & Rubinstein, N. Shedding light on the immunomodulatory properties of galectins: novel regulators of innate and adaptive immune responses. Glycoconj. J. 19, 565–573 (2004).
Liu, F. T. & Rabinovich, G. A. Galectins as modulators of tumour progression. Nat. Rev. Cancer 5, 29–41 (2005).
Gao, X., Liu, J., Liu, X., Li, L. & Zheng, J. Cleavage and phosphorylation: important post-translational modifications of galectin-3. Cancer Metastasis Rev. 36, 367–374 (2017).
Mazurek, N., Conklin, J., Byrd, J. C., Raz, A. & Bresalier, R. S. Phosphorylation of the beta-galactoside-binding protein galectin-3 modulates binding to its ligands. J. Biol. Chem. 275, 36311–36315 (2000).
Yoshii, T. et al. Galectin-3 phosphorylation is required for its anti-apoptotic function and cell cycle arrest. J. Biol. Chem. 277, 6852–6857 (2002).
Danguy, A., Camby, I. & Kiss, R. Galectins and cancer. Biochim. Biophys. Acta 1572, 285–293 (2002).
van den, B. F., Califice, S. & Castronovo, V. Expression of galectins in cancer: a critical review. Glycoconj. J. 19, 537–542 (2004).
Yang, R. Y., Rabinovich, G. A. & Liu, F. T. Galectins: structure, function and therapeutic potential. Expert. Rev. Mol. Med. 10, e17 (2008).
Teichberg, V. I., Silman, I., Beitsch, D. D. & Resheff, G. A beta-D-galactoside binding protein from electric organ tissue of Electrophorus electricus. Proc. Natl Acad. Sci. USA 72, 1383–1387 (1975).
Raz, A. & Lotan, R. Endogenous galactoside-binding lectins: a new class of functional tumor cell surface molecules related to metastasis. Cancer Metastasis Rev. 6, 433–452 (1987).
Raz, A. & Lotan, R. Lectin-like activities associated with human and murine neoplastic cells. Cancer Res. 41, 3642–3647 (1981).
Elad-Sfadia, G., Haklai, R., Ballan, E., Gabius, H. J. & Kloog, Y. Galectin-1 augments Ras activation and diverts Ras signals to Raf-1 at the expense of phosphoinositide 3-kinase. J. Biol. Chem. 277, 37169–37175 (2002).
Andre, S. et al. Galectins-1 and -3 and their ligands in tumor biology. J. Cancer Res. Clin. Oncol. 125, 461–474 (1999).
Gu, M., Wang, W., Song, W. K., Cooper, D. N. & Kaufman, S. J. Selective modulation of the interaction of alpha 7 beta 1 integrin with fibronectin and laminin by L-14 lectin during skeletal muscle differentiation. J. Cell Sci. 107, 175–181 (1994).
Shimura, T. et al. Implication of galectin-3 in Wnt signaling. Cancer Res. 65, 3535–3537 (2005).
Shimura, T. et al. Galectin-3, a novel binding partner of β-catenin. Cancer Res. 64, 6363–6367 (2004).
Martinez-Bosch, N. et al. Galectin-1 drives pancreatic carcinogenesis through stroma remodeling and hedgehog signaling activation. Cancer Res. 74, 3512–3524 (2014).
Rabinovich, G. A. et al. Induction of allogenic T cell hyporesponsiveness by galectin-1-mediated apoptotic and non-apoptotic mechanisms. Cell Death. Differ. 9, 661–670 (2002).
He, J. & Baum, L. G. Presentation of galectin-1 by extracellular matrix triggers T cell death. J. Biol. Chem. 279, 4705–4712 (2004).
Ebrahim, A. H. et al. Galectins in cancer: carcinogenesis, diagnosis and therapy. Ann. Transl Med. 2, 88 (2014).
Rabinovich, G. A. & Conejo-García, J. R. Shaping the immune landscape in cancer by galectin-driven regulatory pathways. J. Mol. Biol. 428, 3266–3281 (2016).
Colnot, C., Fowlis, D., Ripoche, M. A., Bouchaert, I. & Poirier, F. Embryonic implantation in galectin 1/galectin 3 double mutant mice. Dev. Dyn. 211, 306–313 (1998).
Wang, W., Park, J. W., Wang, J. L. & Patterson, R. J. Immunoprecipitation of spliceosomal RNAs by antisera to galectin-1 and galectin-3. Nucleic Acids Res. 34, 5166–5174 (2006).
Demydenko, D. & Berest, I. Expression of galectin-1 in malignant tumors. Exp. Oncol. 31, 74–79 (2009).
Blanchard, H., Bum-Erdene, K., Bohari, M. H. & Yu, X. Galectin-1 inhibitors and their potential therapeutic applications: a patent review. Expert Opin. Ther. Pat. 26, 537–554 (2016).
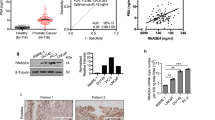
Laderach, D. J. et al. A unique galectin signature in human prostate cancer progression suggests galectin-1 as a key _target for treatment of advanced disease. Cancer Res. 73, 86–96 (2013).
Compagno, D. et al. Glycans and galectins in prostate cancer biology, angiogenesis and metastasis. Glycobiology 24, 899–906 (2014).
Ellerhorst, J., Troncoso, P., Xu, X. C., Lee, J. & Lotan, R. Galectin-1 and galectin-3 expression in human prostate tissue and prostate cancer. Urol. Res. 27, 362–367 (1999).
Ellerhorst, J., Nguyen, T., Cooper, D. N., Lotan, D. & Lotan, R. Differential expression of endogenous galectin-1 and galectin-3 in human prostate cancer cell lines and effects of overexpressing galectin-1 on cell phenotype. Int. J. Oncol. 14, 217–224 (1999).
Clausse, N., van den Brûle, F., Waltregny, D., Garnier, F. & Castronovo, V. Galectin-1 expression in prostate tumor-associated capillary endothelial cells is increased by prostate carcinoma cells and modulates heterotypic cell-cell adhesion. Angiogenesis 3, 317–325 (1999).
van den Brûle, F. A., Waltregny, D. & Castronovo, V. Increased expression of galectin-1 in carcinoma-associated stroma predicts poor outcome in prostate carcinoma patients. J. Pathol. 193, 80–87 (2001).
He, J. & Baum, L. G. Endothelial cell expression of galectin-1 induced by prostate cancer cells inhibits T cell transendothelial migration. Lab. Invest. 86, 578–590 (2006).
Valenzuela, H. F. et al. O-glycosylation regulates LNCaP prostate cancer cell susceptibility to apoptosis induced by galectin-1. Cancer Res. 67, 6155–6162 (2007).
Petrosyan, A., Holzapfel, M. S., Muirhead, D. E. & Cheng, P.-W. Restoration of compact Golgi morphology in advanced prostate cancer enhances susceptibility to galectin-1-induced apoptosis by modifying mucin O-glycan synthesis. Mol. Cancer Res. 12, 1704–1716 (2014).
Shih, T.-C. et al. _targeting galectin-1 impairs castration-resistant prostate cancer progression and invasion. Clin. Cancer Res. 24, 4319–4331 (2018).
Andersen, H., Jensen, O. N., Moiseeva, E. P. & Eriksen, E. F. A proteome study of secreted prostatic factors affecting osteoblastic activity: galectin-1 is involved in differentiation of human bone marrow stromal cells. J. Bone Miner. Res. 18, 195–203 (2003).
Jaworski, F. M. et al. In VivoHemin conditioning _targets the vascular and immunologic compartments and restrains prostate tumor development. Clin. Cancer Res. 23, 5135–5148 (2017).
Corapi, E., Carrizo, G., Compagno, D. & Laderach, D. Endogenous galectin-1 in T lymphocytes regulates anti-prostate cancer immunity. Front. Immunol. 9, 2190 (2018).
Pacis, R. A. et al. Decreased galectin-3 expression in prostate cancer. Prostate 44, 118–123 (2000).
Merseburger, A. S. et al. Involvement of decreased galectin-3 expression in the pathogenesis and progression of prostate cancer. Prostate 68, 72–77 (2008).
Wang, Y. et al. Regulation of prostate cancer progression by galectin-3. Am. J. Pathol. 174, 1515–1523 (2009).
de Melo-Júnior, M. R., Araújo-Filho, J. L. S., Lins, C. A. B., de Pontes-Filho, N. T. & de Carvalho, L. B. Immobilization of anti-galectin-3 onto polysiloxane-polyvinyl alcohol disks for tumor prostatic diseases diagnosis. Appl. Biochem. Biotechnol. 160, 2198–2207 (2010).
Knapp, J. S. et al. Galectin-3 expression in prostate cancer and benign prostate tissues: correlation with biochemical recurrence. World J. Urol. 31, 351–358 (2013).
Geisler, C. et al. Identification and validation of potential new biomarkers for prostate cancer diagnosis and prognosis using 2D-DIGE and MS. Biomed. Res. Int. 2015, 454256 (2015).
van den Brûle, F. A., Waltregny, D., Liu, F. T. & Castronovo, V. Alteration of the cytoplasmic/nuclear expression pattern of galectin-3 correlates with prostate carcinoma progression. Int. J. Cancer 89, 361–367 (2000).
Ahmed, H., Banerjee, P. P. & Vasta, G. R. Differential expression of galectins in normal, benign and malignant prostate epithelial cells: silencing of galectin-3 expression in prostate cancer by its promoter methylation. Biochem. Biophys. Res. Commun. 358, 241–246 (2007).
Califice, S., Castronovo, V., Bracke, M. & van den Brûle, F. Dual activities of galectin-3 in human prostate cancer: tumor suppression of nuclear galectin-3 versus tumor promotion of cytoplasmic galectin-3. Oncogene 23, 7527–7536 (2004).
Fukumori, T. et al. Galectin-3 regulates mitochondrial stability and antiapoptotic function in response to anticancer drug in prostate cancer. Cancer Res. 66, 3114–3119 (2006).
Wang, Y., Nangia-Makker, P., Balan, V., Hogan, V. & Raz, A. Calpain activation through galectin-3 inhibition sensitizes prostate cancer cells to cisplatin treatment. Cell Death Dis. 1, e101 (2010).
Dondoo, T.-O. et al. Galectin-3 is implicated in tumor progression and resistance to anti-androgen drug through regulation of androgen receptor signaling in prostate cancer. Anticancer Res. 37, 125–134 (2017).
Guha, P. et al. Cod glycopeptide with picomolar affinity to galectin-3 suppresses T cell apoptosis and prostate cancer metastasis. Proc. Natl Acad. Sci. USA 110, 5052–5057 (2013).
Glinsky, V. V. et al. The role of Thomsen-Friedenreich antigen in adhesion of human breast and prostate cancer cells to the endothelium. Cancer Res. 61, 4851–4857 (2001).
Glinsky, V. V. et al. Intravascular metastatic cancer cell homotypic aggregation at the sites of primary attachment to the endothelium. Cancer Res. 63, 3805–3811 (2003).
Meng, F., Joshi, B. & Nabi, I. R. Galectin-3 overrides PTRF/Cavin-1 reduction of PC3 prostate cancer cell migration. PLOS ONE 10, e0126056 (2015).
Farhad, M., Rolig, A. S. & Redmond, W. L. The role of Galectin-3 in modulating tumor growth and immunosuppression within the tumor microenvironment. Oncoimmunology 7, e1434467 (2018).
Lee, Y.-C. et al. Secretome analysis of an osteogenic prostate tumor identifies complex signaling networks mediating cross-talk of cancer and stromal cells within the tumor microenvironment. Mol. Cell. Proteomics 14, 471–483 (2015).
Nakajima, K. et al. Galectin-3 cleavage alters bone remodeling: different outcomes in breast and prostate cancer skeletal metastasis. Cancer Res. 76, 1391–1402 (2016).
Pienta, K. J. et al. Inhibition of spontaneous metastasis in a rat prostate cancer model by oral administration of modified citrus pectin. J. Natl Cancer Inst. 87, 348–353 (1995).
Glinskii, O. V. et al. Inhibition of prostate cancer bone metastasis by synthetic TF antigen mimic/galectin-3 inhibitor lactulose-L-leucine. Neoplasia 14, 65–73 (2012).
Nakajima, K. et al. Positive associations between galectin-3 and PSA levels in prostate cancer patients: a prospective clinical study-I. Onco_target 7, 82266–82272 (2016).
Nakajima, K. et al. The influence of PSA autoantibodies in prostate cancer patients: a prospective clinical study-II. Onco_target 8, 17643–17650 (2017).
Ochieng, J. et al. Galectin-3 is a novel substrate for human matrix metalloproteinases-2 and -9. Biochemistry 33, 14109–14114 (1994).
Saraswati, S. et al. Galectin-3 is a substrate for prostate specific antigen (PSA) in human seminal plasma. Prostate 71, 197–208 (2011).
Yang, Y. et al. Treatment of prostate carcinoma with (galectin-3)-_targeted HPMA copolymer-(G3-C12)-5-Fluorouracil conjugates. Biomaterials 33, 2260–2271 (2012).
Glinsky, V. V. & Raz, A. Modified citrus pectin anti-metastatic properties: one bullet, multiple _targets. Carbohydr. Res. 344, 1788–1791 (2009).
Conti, S. et al. Modified citrus pectin as a potential sensitizer for radiotherapy in prostate cancer. Integr. Cancer Ther. 17, 1225–1234 (2018).
Tsai, C.-H. et al. Metastatic progression of prostate cancer is mediated by autonomous binding of galectin-4- O -glycan to cancer cells. Cancer Res. 76, 5756–5767 (2016).
Tzeng, S.-F. et al. O-Glycosylation-mediated signaling circuit drives metastatic castration-resistant prostate cancer. FASEB J. 32, fj201800687 (2018).
Labrie, M. et al. A mutation in the carbohydrate recognition domain drives a phenotypic switch in the role of galectin-7 in prostate cancer. PLOS ONE 10, e0131307 (2015).
Su, Z. Z. et al. Surface-epitope masking and expression cloning identifies the human prostate carcinoma tumor antigen gene PCTA-1 a member of the galectin gene family. Proc. Natl Acad. Sci. USA 93, 7252–7257 (1996).
Gopalkrishnan, R. V. et al. Molecular characterization of prostate carcinoma tumor antigen-1, PCTA-1, a human galectin-8 related gene. Oncogene 19, 4405–4416 (2000).
Danguy, A. et al. Immunohistochemical profile of galectin-8 expression in benign and malignant tumors of epithelial, mesenchymatous and adipous origins, and of the nervous system. Histol. Histopathol. 16, 861–868 (2001).
Nguyen, M. C. et al. Antibody responses to galectin-8, TARP and TRAP1 in prostate cancer patients treated with a GM-CSF-secreting cellular immunotherapy. Cancer Immunol. Immunother. 59, 1313–1323 (2010).
Gentilini, L. D. et al. Stable and high expression of galectin-8 tightly controls metastatic progression of prostate cancer. Onco_target 8, 44654–44668 (2017).
GuhaThakurta, D. et al. Humoral immune response against non_targeted tumor antigens after treatment with Sipuleucel-T and its association with improved clinical outcome. Clin. Cancer Res. 21, 3619–3630 (2015).
Cindolo, L. et al. Galectin-1 and galectin-3 expression in human bladder transitional-cell carcinomas. Int. J. Cancer 84, 39–43 (1999).
Chuang, C.-H. et al. Lab on a chip for multiplexed immunoassays to detect bladder cancer using multifunctional dielectrophoretic manipulations. Lab. Chip 15, 3056–3064 (2015).
Shen, K.-H. et al. Role of galectin-1 in urinary bladder urothelial carcinoma cell invasion through the JNK pathway. Cancer Sci. 107, 1390–1398 (2016).
Li, C.-F. et al. Proteomic identification of the galectin-1-involved molecular pathways in urinary bladder urothelial carcinoma. Int. J. Mol. Sci. 19, 1242 (2018).
Fang, T. et al. Modified citrus pectin inhibited bladder tumor growth through downregulation of galectin-3. Acta Pharmacol. Sin. 39, 1885–1893 (2018).
Matsui, Y. et al. Sensitizing effect of galectin-7 in urothelial cancer to cisplatin through the accumulation of intracellular reactive oxygen species. Cancer Res. 67, 1212–1220 (2007).
Kramer, M. W. et al. Decreased galectin-8 is a strong marker for recurrence in urothelial carcinoma of the bladder. Urol. Int. 87, 143–150 (2011).
Griffioen, A. W. & Thijssen, V. L. Galectins in tumor angiogenesis. Ann. Transl Med. 2, 90 (2014).
Méndez-Huergo, S. P., Blidner, A. G. & Rabinovich, G. A. Galectins: emerging regulatory checkpoints linking tumor immunity and angiogenesis. Curr. Opin. Immunol. 45, 8–15 (2017).
Tsuboi, S. et al. A novel strategy for evasion of NK cell immunity by tumours expressing core2 O-glycans. EMBO J. 30, 3173–3185 (2011).
Wang, W. et al. Tumor-released galectin-3, a soluble inhibitory ligand of human NKp30, plays an important role in tumor escape from NK cell attack. J. Biol. Chem. 289, 33311–33319 (2014).
Li, H. et al. Tim-3/galectin-9 signaling pathway mediates T cell dysfunction and predicts poor prognosis in patients with hepatitis B virus-associated hepatocellular carcinoma. Hepatology 56, 1342–1351 (2012).
Kang, C.-W. et al. Apoptosis of tumor infiltrating effector TIM-3+CD8+ T cells in colon cancer. Sci. Rep. 5, 15659 (2015).
Dardalhon, V. et al. Tim-3/galectin-9 pathway: regulation of Th1 immunity through promotion of CD11b+Ly-6G+ myeloid cells. J. Immunol. 185, 1383–1392 (2010).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01724320 (2012).
Delord, J.-P. et al. A first-in-man phase I study of the galectin-1 (gal-1) inhibitor OTX008 given subcutaneously as a single agent to patients with advanced solid tumors [abstract]. Mol. Cancer Ther. 12 (Suppl. 11), A72 (2013).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT054977 (2012).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT00110721 (2012).
Klyosov, A., Zomer, E. & Platt, D. in Glycobiology and Drug Design (ed. Klyosov, A. A.) 89–130 (American Chemical Society, 2012).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT01723813 (2019).
Linch, S. et al. Galectin-3 inhibition using novel inhibitor GR-MD-02 improves survival and immune function while reducing tumor vasculature. J. Immunother. Cancer 3, 306 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02117362 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02575404 (2018).
Pérez, C. V. et al. Dual roles of endogenous and exogenous galectin-1 in the control of testicular immunopathology. Sci. Rep. 5, 12259 (2015).
Paclik, D. et al. Galectin-2 induces apoptosis of lamina propria T lymphocytes and ameliorates acute and chronic experimental colitis in mice. J. Mol. Med. 86, 1395–1406 (2008).
López, E. et al. Inhibition of chronic airway inflammation and remodeling by galectin-3 gene therapy in a murine model. J. Immunol. 176, 1943–1950 (2006).
Watanabe, M. et al. Clinical significance of circulating galectins as colorectal cancer markers. Oncol. Rep. 25, 1217–1226 (2011).
Verschuere, T. et al. Altered galectin-1 serum levels in patients diagnosed with high-grade glioma. J. Neurooncol. 115, 9–17 (2013).
Ouyang, J. et al. Galectin-1 serum levels reflect tumor burden and adverse clinical features in classical Hodgkin lymphoma. Blood 121, 3431–3433 (2013).
Aggarwal, S., Sharma, S. C. & Das, S. N. Galectin-1 and galectin-3: plausible tumour markers for oral squamous cell carcinoma and suitable _targets for screening high-risk population. Clin. Chim. Acta 442, 13–21 (2015).
Kaneko, N. et al. Potential tumor markers of renal cell carcinoma: α-Enolase for postoperative follow up, and galectin-1 and galectin-3 for primary detection. Int. J. Urol. 20, 530–535 (2013).
Waalkes, S., Merseburger, A. S., Simon, A., Serth, J. & Kuczyk, M. A. Galectin-expression an urologischen tumoren [German]. Urologe 49, 387–391 (2010).
El Gendy, H. et al. Galectin 3 for the diagnosis of bladder cancer. Arab J. Urol. 12, 178–181 (2014).
Poirier, F. & Robertson, E. J. Normal development of mice carrying a null mutation in the gene encoding the L14 S-type lectin. Development 119, 1229–1236 (1993).
Sundblad, V., Morosi, L. G., Geffner, J. R. & Rabinovich, G. A. Galectin-1: a jack-of-all-trades in the resolution of acute and chronic inflammation. J. Immunol. 199, 3721–3730 (2017).
Arthur, C. M., Baruffi, M. D., Cummings, R. D. & Stowell, S. R. Evolving mechanistic insights into galectin functions. Methods Mol. Biol. 1207, 1–35 (2015).
Croci, D. O. et al. Disrupting galectin-1 interactions with N-glycans suppresses hypoxia-driven angiogenesis and tumorigenesis in Kaposi’s sarcoma. J. Exp. Med. 209, 1985–2000 (2012).
Ouyang, J. et al. Viral induction and _targeted inhibition of galectin-1 in EBV+ posttransplant lymphoproliferative disorders. Blood 117, 4315–4322 (2011).
Becher, O. J. & Holland, E. C. Genetically engineered models have advantages over xenografts for preclinical studies. Cancer Res. 66, 3355–3358 (2006).
Day, C.-P., Merlino, G. & Van Dyke, T. Preclinical mouse cancer models: a maze of opportunities and challenges. Cell 163, 39–53 (2015).
Grabowska, M. M. et al. Mouse models of prostate cancer: picking the best model for the question. Cancer Metastasis Rev. 33, 377–397 (2014).
Rea, D. et al. Mouse models in prostate cancer translational research: from xenograft to PDX. Biomed. Res. Int. 2016, 9750795 (2016).
Kobayashi, T., Owczarek, T. B., McKiernan, J. M. & Abate-Shen, C. Modelling bladder cancer in mice: opportunities and challenges. Nat. Rev. Cancer 15, 42–54 (2015).
Eisenstein, M. Organoids: the body builders. Nat. Methods 15, 19–22 (2018).
Vela, I. & Chen, Y. Prostate cancer organoids: a potential new tool for testing drug sensitivity. Expert Rev. Anticancer Ther. 15, 261–263 (2015).
Gao, D. et al. Organoid cultures derived from patients with advanced prostate cancer. Cell 159, 176–187 (2014).
Karthaus, W. R. et al. Identification of multipotent luminal progenitor cells in human prostate organoid cultures. Cell 159, 163–175 (2014).
Lee, S. H. et al. Tumor evolution and drug response in patient-derived organoid models of bladder cancer. Cell 173, 515–528 (2018).
Yoshida, T., Singh, A. K., Bishai, W. R., McConkey, D. J. & Bivalacqua, T. J. Organoid culture of bladder cancer cells. Investig. Clin. Urol. 59, 149 (2018).
Wang, S., Gao, D. & Chen, Y. The potential of organoids in urological cancer research. Nat. Rev. Urol. 14, 401–414 (2017).
Kantoff, P. W. et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N. Engl. J. Med. 363, 411–422 (2010).
Goswami, S., Aparicio, A. & Subudhi, S. K. Immune checkpoint therapies in prostate cancer. Cancer J. 22, 117–120 (2016).
Beer, T. M. et al. Randomized, double-blind, phase III trial of ipilimumab versus placebo in asymptomatic or minimally symptomatic patients with metastatic chemotherapy-naive castration-resistant prostate cancer. J. Clin. Oncol. 35, 40–47 (2017).
Fakhrejahani, F. et al. Avelumab in metastatic castration-resistant prostate cancer (mCRPC). J. Clin. Oncol. 35, 159–159 (2017).
Acknowledgements
This work was supported by grants from the Spanish Ministry of Economy and Competitiveness/ISCIII-FEDER (PI14/00125 and PI17/00199), an AECC-Cataluña 2015 grant and the Generalitat de Catalunya (2014/SGR/143 and 2017/SGR/225) grant to P.N. The authors thank V. A. Raker for valuable comments and input on language.
Reviewer information
Nature Reviews Urology thanks V. V. Glinsky, P. Nangia-Makker and other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, made substantial contributions to discussion of the article contents and reviewed and/or edited the manuscript before submission. P.N. and N.M.-B. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martínez-Bosch, N., Rodriguez-Vida, A., Juanpere, N. et al. Galectins in prostate and bladder cancer: tumorigenic roles and clinical opportunities. Nat Rev Urol 16, 433–445 (2019). https://doi.org/10.1038/s41585-019-0183-5
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-019-0183-5
This article is cited by
-
Galectins as potential therapeutic _targets in STIs in the female genital tract
Nature Reviews Urology (2022)
-
Galactose specific lectins from prostate tissue with different pathologies: biochemical and cellular studies
Molecular Biology Reports (2022)