Abstract
Insulin glargine (IGlar) 100 U/mL (IGlar-100) is widely used in East Asian countries for the treatment of type 2 diabetes mellitus (T2DM) and is the gold standard of basal insulin treatment. In this review we summarize key information about clinical experience with IGlar-100 in East Asian patients with T2DM, including findings from clinical trials and postmarketing studies. We also provide recommendations and opinions on the optimal use of IGlar-100 in this population. The findings from the studies highlighted in our review indicate that IGlar-100 can be a suitable treatment option for East Asians with T2DM, from initial therapy in combination with oral antihyperglycemic medications through to different combinations and intensification models.
Funding
Eli Lilly and Company.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global diabetes epidemic is particularly evident in East Asia, where estimates from the International Diabetes Federation are alarming [1]. In 2017, prevalence among adults ranged from 7.7% to 13.7% in this region with more than 1 million diabetes-related deaths [1]. In 2017, China was among the top 10 countries globally for number of people with diabetes (114 million), and both China and Japan were among the top 10 countries globally for total healthcare expenditure on diabetes [1]. Given the expected rise in prevalence in coming decades [2], evidence-based optimization of treatment will be critical for combating this epidemic in East Asia.
Type 2 diabetes mellitus (T2DM) treatment begins with lifestyle interventions, before progressing to pharmacological interventions with advancing disease. Despite the introduction of numerous antihyperglycemic medications, many patients with T2DM require insulin, and basal insulins continue to be frequently used either as first-line insulin treatment or as part of multiple daily injection regimens. The ideal basal insulin, including basal insulin analogs, should reproduce physiological basal insulin secretion, thereby restoring glycemic control, without hypoglycemia [3, 4]. Such therapy should have relatively flat/constant insulin concentration profile over time, no pronounced peak, duration of action of at least 24 h, low within-patient variability in fasting plasma glucose (FPG), a favorable safety profile, including low risk of hypoglycemia and weight gain, and be easy to administer and titrate.
Insulin glargine (IGlar) 100 U/mL (IGlar-100) (Lantus®, Sanofi-Aventis, Paris, France) [5, 6], the first basal insulin analog, came to market in 2000 [7] and was a breakthrough in the field of insulin therapy. Since that time, IGlar-100 has become one of the most widely studied, prescribed, and established diabetes medications globally [8, 9], including in East Asia. It continues to be a gold standard of basal insulin treatment and a benchmark for new injectable antihyperglycemic treatments, including newer basal insulin analogs.
East Asians with T2DM have distinct pathophysiological features vs their Caucasian counterparts [10], including lower age of disease onset, lower body mass index (BMI), predisposition to β-cell failure in the context of insulin resistance, higher postprandial hyperglycemia, and increased risk of renal complications/stroke [10]. These and other economic, cultural, and social factors might contribute to differences in the way antihyperglycemic medications, including insulins, are used in East Asians, as well as to treatment outcomes and overall clinical experience.
The objectives of this review were to summarize the following in East Asian patients with T2D: (1) pharmacokinetics and pharmacodynamics of IGlar 100 U/mL, (2) efficacy and safety data for clinical trials and observational studies of IGlar and oral antihyperglycemic medications (OAMs), (3) efficacy and safety data from clinical trials comparing IGlar with other injectable treatments, (4) efficacy and safety data from trials of patients switching to IGlar from other diabetes therapies, and (5) real-world use of IGlar. The final objective was to offer general treatment recommendations for East Asian patients with T2DM based on findings from studies reviewed, and on clinical experience of the authors. Database searches (Medline, Embase, the Cochrane Library, and the Ichushi database) were performed to identify studies of IGlar in East Asian patients relevant to each of the objectives listed above.
Consequently, this article is based on previously conducted studies and does not contain any new results of studies with human participants or animals performed by any of the authors.
Pharmacokinetics and Pharmacodynamics of Insulin Glargine 100 U/mL
When injected subcutaneously, the acidic IGlar solution is neutralized, leading to the formation of microprecipitates from which small amounts of IGlar are slowly released, resulting in a relatively constant concentration–time profile over 24 h with no pronounced peak [6]. IGlar is rapidly metabolized to two active metabolites M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin), of which only M1 is typically detectable in plasma [5]. Early pharmacokinetic/pharmacodynamics (PK/PD) studies involving Caucasian healthy volunteers [11] and patients with type 1 diabetes mellitus (T1DM) [12] demonstrated that in comparison with human insulin neutral protamine Hagedorn (NPH), IGlar had slower onset of action, flatter PK and action profile with no pronounced peak of insulin concentration and action, and prolonged action of approximately 24 h. Table 1 summarizes PK/PD studies of IGlar in East Asians [13,14,15,16]. A study involving 15 Japanese healthy volunteers, which used a similar protocol to the earlier trial involving Caucasians [11], showed that after subcutaneous injection of IGlar, time–action profiles in Japanese subjects were very similar to those in Caucasians [15]. In contrast to the action profiles of NPH, which had a distinct peak of action in both Caucasians and Asians, IGlar had a smooth profile with no distinct peak [15]. Further evidence for consistency of IGlar PK/PD profiles in East Asians and Caucasians comes from two studies comparing the PK/PD of IGlar-100 and IGlar 300 U/mL (IGlar-300) in Japanese and European patients with T1DM, respectively [16].
Combining Insulin Glargine 100 U/mL with OAMs in Patients with T2DM
In T2DM, first-line insulin therapy is typically started after failure of therapy with 1–3 OAMs [17]. Basal supported oral therapy (BOT) is widely used for T2DM and involves adding basal insulin to an OAM regimen. This strategy of combining therapies with different modes of action offers an opportunity to address distinct pathophysiological mechanisms of the disease [18]. IGlar is frequently used for BOT. Various combinations of 1–2 OAMs with IGlar have been evaluated in global studies which demonstrated similar glycemic efficacy to NPH with similar/lower risk of hypoglycemia [19,20,21].
BOT with IGlar has also been evaluated in East Asian populations. Table 2 summarizes some of the key efficacy and safety data for randomized controlled trials (RCTs) [22,23,24,25,26] and observational studies [27,28,29,30,31,32,33,34,35,36,37] of IGlar and OAMs in East Asian patients with T2DM. The studies varied in design, population size, duration, and quality, but generally involved patients with inadequate glycemic control on OAMs subsequently initiating insulin therapy with ongoing OAM treatment. Specific combinations examined, mostly in RCTs, included metformin, sulfonylureas, glinides, α-glucoside inhibitors, and dipeptidyl peptidase-4 inhibitors (DPP-4i). As results of the Add-on Lantus to Oral Hypoglycemic Agents 2 (ALOHA2) Japanese surveillance study reported in 2014 showed, IGlar was used for BOT in the vast majority of patients, with approximately 29% of patients using it in combination with one OAM, 30% with two OAMs, and 21% with three OAMs [32]. Sulfonylureas were the most commonly used concomitant OAMs (70% at baseline, 71% during study) followed by DPP-4i (54% at baseline, 61% during study). Biguanides (45% at baseline, 49% during study) and α-glucosidase inhibitors (27% at baseline, 30% during study) were also commonly prescribed. No information on the combination of sodium/glucose cotransporter-2 (SGLT-2) inhibitors with IGlar was reported [32].
Results of the Observational Registry of Basal Insulin Treatment (ORBIT) observational study in China indicate that before insulin initiation, metformin was the most commonly used OAM (65%) followed by sulfonylureas (46%) and α-glucosidase inhibitors (24%) [38]. Use of DPP-4i was uncommon. IGlar was the most commonly chosen basal insulin in ORBIT (71% vs 13% using insulin detemir, 16% using NPH) [39].
Clinical outcomes of combination therapy with specific OAMs used were not reported in most observational studies (Table 2). Regardless of OAM combination or type/length of study, and consistent with global studies, improved glycemic control was observed, with one study also reporting similar outcomes between younger and older patients [27] and another (JUN-LAN Study 7) finding that the addition of step-up bolus insulin to combination therapy with IGlar and sulfonylurea improved glycemic control [35]. Safety findings were consistent between studies, with hypoglycemia and some weight gain commonly observed (Table 2). The remaining paragraphs in this section provide more detailed descriptions of IGlar BOT studies with various classes of OAMs in different East Asian populations.
Biguanides
The combination of IGlar and biguanide (e.g., metformin) is commonly used in Western populations, in combination with other OAMs, and also with other insulins because of its efficacy, reduced body weight gain, insulin requirements, and potentially also lower risk of hypoglycemia when compared to insulin monotherapy, or insulin combined with sulfonylurea [40, 41]. In East Asians, metformin is frequently used in combination with IGlar in T2DM [23,24,25, 27].
Sulfonylureas
In insulin-naïve Japanese patients with T2DM, adding IGlar to failing sulfonylurea therapy effectively improved glycemic control and maintained intrinsic basal insulin secretion while postprandial insulin secretion did not change [34]. Adding IGlar to sulfonylurea not only improved glycemic control but also seemed to restore markers of β-cell function [42]. Sulfonylurea dose might be reduced after IGlar is added without affecting glycemic control or insulin requirements [42].
The combination of IGlar and sulfonylurea has also been compared with other treatment options in East Asian patients. In Chinese patients with newly diagnosed T2DM and high HbA1c, treatment with IGlar plus OAMs (metformin and/or glimepiride) or treatment with OAMs (metformin and glimepiride alone/in combination) was very effective in achieving normoglycemia [25]. However, more patients achieved _target glycemic control in less time in the OAM + insulin group than in the OAM group. Moreover when treatment was stopped, significantly more patients maintained _target glycemia without OAMs and had greater recovery of β-cell function in the OAM + IGlar group vs the OAM group [25]. No episodes of hypoglycemia were reported during the intensive intervention period and body weight was unchanged after treatment in both groups [25].
The efficacy and safety of adding IGlar to either metformin + glimepiride or to glimepiride alone was evaluated in Korean patients with T2DM poorly controlled with OAMs [23]. Adding IGlar to glimepiride + metformin was more effective than adding to glimepiride alone in reducing HbA1c and postprandial glucose despite the lower insulin dose required and similar hypoglycemia incidence [23].
The combination of glimepiride + IGlar was effective and safe in ethnic Japanese patients with T2DM living in Brazil not adequately controlled with OAMs [43]. Consistent with studies in Caucasians, Japanese patients required IGlar doses greater than 30 U/day for significantly improved glycemic control [43].
Real-world data from Japan confirm an increased risk of hypoglycemia in patients using IGlar + sulfonylurea vs non-sulfonylurea users. However, risk of any hypoglycemia reported in the observational study was low overall (5%) [32].
Dipeptidyl Peptidase-4 Inhibitors
DPP-4i improve glycemic control with low risk of hypoglycemia and neutral body weight effects [44]. They effectively lower postprandial glycemia [44] and are a frequently chosen treatment option in East Asian patients with T2DM using combination therapy with IGlar [32]. Real-world evidence from Japan showed that using DPP-4i with IGlar does not increase hypoglycemia risk compared to use of IGlar without DPP-4i [32]. In Chinese patients with newly diagnosed T2DM, both IGlar monotherapy and combination therapy with IGlar plus the DPP-4i saxagliptin were highly effective over 3 months with very little hypoglycemia [22]. The efficacy of combination therapy with saxagliptin and IGlar was superior to monotherapy with IGlar. Insulin doses were not reported [22].
The real-world combination of IGlar and DPP-4i was highly effective in Japanese patients, with similar efficacy to the combination of IGlar + metformin. The efficacy of different multiple OAM combinations, including DPP-4i, with IGlar was similar, and there were no differences between different cohorts regarding hypoglycemia. However, incidence and rates of hypoglycemia were low in all sub-cohorts [37].
Glinides and α-Glucosidase Inhibitors
Postprandial glucose excursions can also be _targeted by treatment with glinides or α-glucosidase inhibitors [26], and their use in Asia is more popular than in Western countries [26]. A 20-week Korean study compared the safety and efficacy of the glinide mitiglinide and the α-glucosidase inhibitor voglibose in combination with once-daily IGlar in patients with T2DM with HbA1c > 7.0% (53 mmol/mol) despite treatment with a combination of OAMs or monotherapy with IGlar [26]. Switching to both treatments resulted in improved glycemic control with HbA1c decreases of 0.7–0.9% (8–10 mmol/mol). Both treatments exhibited similar glycemic efficacy and were well tolerated. Very few patients experienced hypoglycemia and patients treated with mitiglinide + IGlar experienced moderate weight gain (0.93 kg) [26]. Japanese studies compared short-term [45] and long-term [46] effects of mitiglinide combined with once-daily IGlar after switching from a multiple daily insulin regimen of insulin aspart and IGlar. Short-term use of mitiglinide + IGlar was effective in lowering both fasting and postprandial hyperglycemia in a subpopulation of Japanese patients with T2DM. Patients who responded well to this regimen were younger and heavier (larger BMI) than those not responding well [45]. In a subsequent study some of the responsive patients from the short-term study continuing the regimen were followed for 6 months [46]. In these patients the mitiglinide + IGlar regimen provided effective and comparable glycemic control to the insulin aspart and IGlar regimen.
Insulin Glargine vs Other Injectable Treatments in Patients with Type 2 Diabetes Mellitus
IGlar vs NPH
Until basal insulin analogs became available, NPH was frequently used as a substitute for basal insulin secretion in both T1DM and T2DM. This intermediate-acting insulin has a number of limitations, including variable absorption, high interindividual and intraindividual variation, discernible peak plasma insulin concentrations, and activity of less than 24 h duration [47].
Several global studies compared IGlar with NPH as initial insulin therapy in T2DM [20, 48, 49]. Similar glycemic efficacy was observed between IGlar and NPH. In the Treat-to-_target trial, patients with T2DM added IGlar or NPH to oral therapy and titrated to a FPG ≤ 100 mg/dl [20]. Most (approx. 60%) patients achieved HbA1c ≤ 7% (53 mmol/mol) with each insulin. However, significantly more patients treated with IGlar attained this without documented nocturnal hypoglycemia, and rates of other categories of symptomatic hypoglycemia were lower with IGlar [20]. Several meta-analyses confirmed similar glycemic efficacy between IGlar and NPH and lower rates of hypoglycemia with IGlar vs NPH [50,51,52].
Although fewer trials have been carried out in East Asian populations, results were consistent with global studies—similar glycemic efficacy to NPH and may be associated with reduced risk of hypoglycemia (Table 3) [53, 54]. A 28-week study carried out in Japan compared the efficacy and safety of IGlar to NPH, both concurrent with OAM use, in patients with T2DM [53]. After 28 weeks, reduction in HbA1c was similar in both groups, as were the incidences of symptomatic, severe, and nocturnal hypoglycemia. However, there was a significantly greater decrease in FPG at 28 weeks in the IGlar vs NPH group (Table 3) [53].
In a Chinese continuous glucose monitoring study (CGMS) the efficacy and safety of IGlar in patients with T2DM inadequately controlled on sulfonylurea was evaluated [54]. Patients were randomized to the combination treatment of extended-release glipizide with either IGlar or NPH. At week 12, FPG and HbA1c decreased similarly in both groups. CGMS data showed that IGlar was associated with significantly lower glycemic variability. While the incidence of total hypoglycemia was comparable between the two groups, the incidence of nocturnal hypoglycemia was significantly lower in the IGlar vs NPH group (Table 3). No serious hypoglycemia was reported [54].
An open-label, 24-week, noninferiority study randomized patients with T2DM inadequately controlled on OAMs from 10 countries in Asia [55]. This study investigated the safety and efficacy of once-daily IGlar vs once-daily NPH, both with once-daily glimepiride. After 24 weeks, IGlar was superior to NPH in HbA1c reduction, and number of hypoglycemic episodes (symptomatic, severe, and nocturnal) was significantly lower with IGlar vs NPH [55].
IGlar vs Premixed Insulin
Premixed insulins, including both premixed human insulin and insulin analogs, are used for both initiation and intensification in various insulin treatment models [56]. Results of numerous comparator trials indicate that when used as a starter insulin added to OAMs in patients with T2DM, premixed insulin formulations might have similar/greater efficacy vs IGlar, but may increase the risk of non-severe hypoglycemia and trigger greater body weight gain [57,58,59,60].
Use of premixed formulations for initiation of insulin therapy is particularly common in East Asian patients with T2DM as a result of the higher prevalence of postprandial hyperglycemia vs Caucasians with T2DM [61]. A number of RCTs compared the efficacy and safety of IGlar (with/without prandial insulin) with that of premixed human and analog insulins for initiation [62,63,64,65,66,67] or intensification [68,69,70] of insulin therapy in East Asians with T2DM (Table 3). Overall, IGlar (with/without prandial insulin, in combination with OAM) and premixed insulin formulations (with/without OAM) compared in RCTs seem to be similarly effective in East Asians with similar safety profiles (Table 3). However, few trials comparing these treatment options in East Asians had comparable designs, population sizes, and durations which would allow firm conclusions for clinical practice. In several of these studies, some of which adopted structured titration algorithms, insulin treatment did not lower mean HbA1c levels to 7% (53 mmol/mol) and significant proportions of patients did not achieve HbA1c < 7% (53 mmol/mol) (Table 3). This might reflect a general problem of suboptimal insulin use in T2DM in East Asia, suboptimal use of combination therapies, self-monitoring blood glucose, or other barriers to achievement of better glycemic control without hypoglycemia.
IGlar vs Newer Basal Insulin Analogs
Global studies demonstrated that newer basal insulin analogs, with longer durations of action than IGlar-100, including IGlar-300 and insulin degludec (IDeg), have similar efficacy to IGlar-100 in patients with T2DM, but may lower the risk of hypoglycemia in some patient populations [71,72,73], particularly in those at higher risk of hypoglycemia [74].
Japanese RCTs have also compared the efficacy and safety of IGlar-100 and IGlar-300 in patients previously treated with basal insulin [75] and IDeg in insulin-naïve patients [76] (Table 3). Consistent with findings from global studies [75], IGlar-100 and IGlar-300 had similar efficacy in patients previously treated with basal insulin and the risk of hypoglycemia, particularly nocturnal, was reduced with IGlar-300. However, a higher dose of IGlar-300 was required to achieve similar efficacy. The increase in body weight was also less pronounced with IGlar-300 [75], a finding also observed in a global study involving patients previously treated with basal insulin [77]. Unfortunately, no data are available concerning the efficacy and safety of IGlar-100 vs IGlar-300 in East Asian patients new to insulin. For most hypoglycemia categories, treatment of insulin-naïve patients with IGlar-300 vs IGlar-100 did not result in significantly lower risk in the global EDITION-3 trial despite the trend [78, 79], and it would be of interest if similar findings would be applicable to East Asians.
In a Japanese subgroup analysis of the BEGIN ONCE ASIA trial involving insulin-naïve patients and comparing IDeg and IGlar-100, IGlar-100 and IDeg had similar efficacy [76]. A numerically lower incidence of overall and nocturnal hypoglycemia was reported with IDeg vs IGlar, but these differences were not statistically significant [76]. Similar efficacy and hypoglycemia risk with IDeg and IGlar-100 were also found in a small RCT involving insulin-naïve Japanese patients with T2DM [80].
IGlar vs/+ Glucagon-Like Peptide-1 Receptor Agonists
Glucagon-like peptide-1 receptor agonists (GLP-1RAs) have been used as an alternative first-line injectable therapy in T2DM, and in global studies had similar/slightly better efficacy, a potentially lower risk of hypoglycemia, and greater body weight reduction vs IGlar + OAMs [81]. GLP-1RAs have also been used as add-on therapy in patients with inadequate glycemic control on basal insulin regimens, with global studies demonstrating this combination to be at least as effective as adding rapid-acting insulin to basal insulin regimens, and is associated with weight loss and decreased hypoglycemia [82]. Of note, treatment with GLP-1RAs was associated with a higher incidence of gastrointestinal adverse events [81], which might preclude their use in some patients. Furthermore, GLP-1RAs should be used cautiously in insulin-dependent patients (i.e., with advanced disease who are not able to produce insulin/have β-cell failure) [83].
Several RCTs carried out in Japan or other Asian countries have compared the efficacy and safety of IGlar with that of GLP-1RAs [84,85,86,87] (Table 3). Consistent with global findings, GLP-1RAs had similar/slightly better efficacy to IGlar as first-line injectable therapy, and were associated with a lower incidence of hypoglycemia, weight loss (vs weight gain with IGlar), and increased incidence of gastrointestinal symptoms [84, 85, 88]. Other trials have shown that add-on GLP-1RAs can improve glycemic control in Japanese or mostly East Asian patients with inadequate glycemic control on insulin regimens [86, 87].
Switching to Insulin Glargine from Other Diabetes Therapies
Several mostly prospective cohort studies carried out in China and Japan have reported on the efficacy and safety of switching from NPH [89,90,91] or premixed insulin [92,93,94,95,96,97,98] to IGlar in patients with inadequate glycemic control (Table 4). The NPH switch studies generally demonstrated significant improvement in HbA1c and fasting glucose concentrations after 26–78 weeks of IGlar, with weight gain (Table 4). Premixed insulin switch studies also generally demonstrated significant HbA1c and fasting glucose improvements after 12–156 weeks of IGlar + OAMs, with no effect on/improvement in body weight (Table 4). The findings from these mostly prospective studies, however, should be considered with caution as the improvement in glycemic control might be attributable to factors other than IGlar alone.
Two Japanese studies also reported findings in which patients were switched from IGlar + glimepiride to IGlar + sitagliptin [99], and from GLP-1RAs to IGlar [100], respectively. In the first of these studies [99], mean blood glucose (BG) fluctuation significantly decreased from baseline after 2 months of treatment with IGlar + sitagliptin, while in the second [100], there were significant improvements in HbA1c and FPG after 24 weeks of IGlar treatment.
Real-World Use of Insulin Glargine in East Asians
Two Japanese prospective 24-week postmarketing surveillance studies provided important evidence for real-world effectiveness and safety of IGlar in East Asian patients with T2DM. The ALOHA (Add-on Lantus to Oral Hypoglycemic Agents) study was conducted between 2007 and 2009 and involved 5223 subjects [101, 102]. Most were treated with a combination of IGlar + sulfonylurea, either alone or in combination with other OAMs including metformin, α-glucosidase inhibitors, or thiazolidinediones [101, 102]. The second study (ALOHA2) was conducted in 2012 and involved 2630 patients, of whom approximately 60% used DPP-4i, which has become a popular therapeutic option in Japan [32]. Both studies showed that basal insulin therapy initiation is delayed in Japan. Mean HbA1c in insulin-naïve patients starting their insulin therapy and enrolled in the two studies was greater than 9% (75 mmol/mol) and approximately half of ALOHA subjects had microvascular complications of diabetes at baseline [32, 33, 103]. Insulin therapy in combination with OAMs significantly improved glycemic control in study subjects, yet only 15.5% and 26.3% achieved HbA1c < 7.0% (53 mmol/mol) in ALOHA and ALOHA2, respectively [103, 104], a proportion much lower than typically reported in RCTs. This might be explained by insufficient insulin dosing and titration. Initial IGlar doses were lower in the ALOHA cohort than doses recommended and used in Europe and North America [17, 33], while the study provided evidence that use of higher doses and titration aimed at the effective lowering of FPG to below 110 mg/dL is key for treatment success [105]. Using FPG alone to guide titration of IGlar was shown to be the most successful way of BG monitoring among patients not only in terms of achievement of the HbA1c _target of less than 7.0% (53 mmol/mol) but also reported hypoglycemia rate and highest compliance [106]. Incidence and rates of hypoglycemia were low (incidence of 1% and 5.59%, incidence rate of 0.035 and 0.2332 episodes/patients-years in ALOHA and ALOHA2, respectively) [104, 107]. While these studies have limitations and may not provide a comprehensive assessment of hypoglycemia risk, the low hypoglycemia rates reported do not explain suboptimal insulin dosage in patients not achieving optimal glycemic control. Similarly, increases in body weight which typically are associated with effective insulin treatment in T2DM [108] were only moderate in the ALOHA (up to 1.2 kg) and ALOHA2 studies (0.5 kg) [32] and do not explain conservative dosage and titration of insulin.
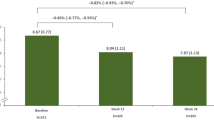
The ORBIT prospective study, conducted in China between 2011 and 2013, provided insight into results of basal insulin treatment in a large cohort (16,341 patients completed 6 months follow-up) of Chinese patients with T2DM inadequately treated with OAMs [30, 39]. Baseline HbA1c levels were high [mean HbA1c among patients starting basal insulin therapy was 9.6% (81 mmol/mol)] [30]. Among patients with available data after 3 and 6 months of therapy, glycemic control improved significantly at 6 months with an overall reduction in HbA1c of 2.1% (23 mmol/mol) [2.2% (24 mmol/mol) in the IGlar cohort]. However, these results may not be generalizable to other populations as a large proportion of patients, whose results were likely less positive, were lost to follow-up. While the starting dose of basal insulin (mean ± SD) of 0.18 ± 0.07 IU/kg/day was consistent with current recommendations, there was only a minimal increase in dose over 6 months of treatment (0.03 IU/kg/day). Among uncontrolled patients, more than 30% did not report dose titration between consecutive visits [39]. The study results indicate that initiation of basal insulins in a real-world setting was associated with minor weight gain (0.10 kg over 6 months in the entire study cohort, 0.09 kg in an IGlar cohort [30]) and no significant increase in hypoglycemia risk from before basal insulin initiation to 6 months after initiation [39]. The rate of general hypoglycemia was significantly lower in patients treated with IGlar vs insulin detemir or NPH insulin [30]. Similar to the Japanese ALOHA findings, low risk of hypoglycemia and low weight gain do not explain the lack of effective insulin titration in Chinese participants of this study.
Smaller observational studies evaluated use of IGlar after switching from NPH in Japanese patients with T1DM and T2DM using basal-bolus therapy (JUN-LAN Study) [89]. Over 18 months, patients with T2DM experienced sustained improvement of glycemic control as reflected by change of HbA1c and fasting BG while the incidence rate of mild-to-moderate hypoglycemia did not change significantly. As expected, patients with T2DM experienced increased body weight, albeit moderate. However, mean HbA1c at endpoint was still 7.7% (61 mmol/mol), and total daily insulin dose and daily basal insulin dose were relatively low. Another small observational study provided similar reassuring safety data on using IGlar in elderly (≥ 65 years) Taiwanese patients with T2DM vs younger (< 65 years) Taiwanese patients [27].
No unexpected safety findings were reported from these observational studies. Taken together, these findings show that while IGlar is well tolerated and safe for treating patients with T2DM, its full therapeutic potential might remain unrealized. Earlier insulinization and more effective dosing may further increase the value of this insulin product for patients in East Asia.
Insulin Glargine 100 U/mL: Recommendations
Clearly, the use of IGlar-100 for the treatment of East Asians with T2DM should be determined on a case-by-case basis, and other factors should be considered when making prescribing decisions such as patient’s preference for a dosing device and price. We offer the following general recommendations based on findings from studies involving East Asians and on our clinical experience.
Initiation: Guidelines and Timing
Consistent with other guidelines, initiation of insulin therapy in East Asian patients with T2DM is recommended when BG concentrations cannot be controlled with diet and lifestyle modifications and with other therapies [109,110,111,112]. Basal IGlar may be used as first-line insulin treatment in combination with OAMs, as is common in Western countries [17]. The guidelines for initiating insulin vary somewhat between the main East Asian countries (Table 5). For instance, Japanese and Taiwanese guidelines do not specify the type of insulin(s) that may be used for initiation, whereas Chinese and Korean guidelines state that basal or premixed insulins may be used for initiation [109, 111].
According to the findings of the First Basal Insulin Evaluation (FINE) Asia study, initiation of insulin is being overly delayed in many Asian, including East Asian, countries [113]. Evidence from Japan suggests that this may, at least in part, be due physician reluctance to initiate insulin [114]. These findings of clinical inertia are alarming in light of an ALOHA subanalysis showing that patients with a disease duration < 1 year and those with HbA1c < 8.5% (69 mmol/mol) on initiation of IGlar were most likely to attain HbA1c _targets [103]. These results were not unexpected and are consistent with findings in the follow-up ALOHA2 study that patients with shorter disease duration and those with lower HbA1c levels at baseline were more likely to achieve HbA1c _targets when treated with IGlar [104]. Clearly, early initiation of insulin therapy is critical to optimize treatment outcomes; physicians in East Asia should consider immediately starting insulin therapy in patients not achieving glycemic control with other therapeutic approaches. Therefore, IGlar-100 can be an appropriate choice for use in insulin-naïve patients in combination with OAMs, and in multiple injection therapy models involving mealtime insulin.
Initiation Dose, Titration, and Combination with OAMs
For patients not achieving glycemic control with OAMs and lifestyle interventions, we recommend initiating IGlar-100 at a dose of 0.15 U/kg, with subsequent titration to achieve a _target FPG of 110 mg/dL or less [101, 105]. An FPG _target of 110 mg/dL or less may be considered for patient-led titration, which, although less commonly applied in Asian countries than in Western countries, has been demonstrated to be as effective as physician-led titration [115]. IGlar may be combined with commonly used OAMs (individual/multiple). Treating physicians should consider the characteristics of patients and choose the most appropriate OAMs on a case-by-case basis.
Intensification of Therapy
Patients on IGlar-100 who are not maintaining glycemic control require intensification of therapy. A recent pooled analysis of data from 16 RCTs compared outcomes between Asian and non-Asian patients with T2DM initiating IGlar-100 [116]. This analysis showed that Asian patients are less likely to achieve _target HbA1c despite similar FPG reduction and similar hypoglycemia incidence vs non-Asian patients. This finding may reflect greater postprandial hyperglycemia in Asian patients and may indicate that timely intensification of therapy is of particular importance among Asian patients.
The intensification strategy should be determined on the basis of each patient’s clinical characteristics and preferences. Options for insulin intensification include basal plus, basal-bolus, and premixed insulin analog regimens. For basal plus regimens, a rapid-acting insulin is added before the largest meal with a starting dose of 4 units, 0.1 U/kg, or 10% of basal insulin dose [17]. For basal-bolus regimens, it is important to consider the basal IGlar to total daily insulin ratio for effective glycemic control and to reduce the risk of hypoglycemia. Specifically, IGlar should be titrated first before titrating the bolus insulin; a ratio of approximately 0.5 is optimal [117]. After basal insulin failure, prandial insulin might be added and options include use of premixed formulations once-, twice-, or thrice-daily [56, 69]. In the case of the commonly used option of twice-daily dosing, the dose should be split 50:50 [56]. Sulfonylureas should be discontinued while metformin should be continued if not contraindicated [118]. Add-on treatment with GLP-1RAs [86, 87] or SGLT-2 inhibitors [119,120,121] may also be considered for intensifying basal IGlar-100 treatment.
Conclusions
IGlar-100 is the benchmark basal insulin and may continue to be an important part of treating T2DM in East Asia for the foreseeable future. The PK/PD profiles of IGlar in East Asians were very similar to those in Caucasians. Clinical trials and real-world studies have examined the efficacy and safety of IGlar in different clinical settings in East Asian populations. The findings show that in East Asian populations, IGlar can be used safely and effectively across all injectable therapy lines, from initial basal insulin therapy in combination with OAMs through to different combinations and intensification models, and in combination with mealtime insulins or GLP-1RAs. The findings from clinical trials involving East Asians are generally consistent with global clinical trials and inform clinical practice decisions. Real-world evidence suggests that earlier insulinization and more effective titration may further increase the value of IGlar for patients in East Asia.
In East Asian patients with T2DM, basal IGlar may be used as first-line insulin treatment in combination with OAMs. Early initiation of insulin therapy is critical and physicians in East Asia should immediately consider it in patients not achieving glycemic control with other therapies. Therapy should be intensified in IGlar patients not maintaining glycemic control and the intensification strategy should be individualized. Insulin intensification options include basal plus, basal-bolus, and premixed insulin analog regimens. Addition of GLP-1RAs or SGLT-2 inhibitors may also be considered for intensifying basal IGlar-100 treatment in East Asian patients with T2DM.
References
International Diabetes Federation. Brussels, Belgium: IDF; 2017. IDF diabetes atlas—8th edition. https://idf.org/e-library/welcome.html. Accessed 10 Jun 2018.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49.
Pettus J, Santos Cavaiola T, Tamborlane WV, Edelman S. The past, present, and future of basal insulins. Diabetes Metab Res Rev. 2016;32:478–96.
Rossetti P, Ampudia-Blasco FJ, Ascaso JF. Old and new basal insulin formulations: understanding pharmacodynamics is still relevant in clinical practice. Diabetes Obes Metab. 2014;16:695–706.
European Medicines Agency. London, UK: EMA; 2009. Lantus summary of product characteristics; 2009 May 8. https://www.ema.europa.eu/documents/product-information/lantus-epar-product-information_en.pdf. Accessed 23 Jan 2018.
Food and Drug Administration. Silver Spring, MD: FDA; 2015. Lantus prescribing information; 2015 Jul. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/021081s063lbl.pdf. Accessed 23 Jan 2018.
Bolli GB, Owens DR. Insulin glargine. Lancet. 2000;356:443–5.
Lindsley CW. 2014 global prescription medication statistics: strong growth and CNS well represented. ACS Chem Neurosci. 2015;6:505–6.
Philippidis A. The top 15 best-selling drugs of 2016. Genet Eng Biotechnol News. 2017 Mar 6. https://www.genengnews.com/the-lists/the-top-15-best-selling-drugs-of-2016/77900868. Accessed 23 Jan 2018.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci. 2013;1281:64–91.
Heinemann L, Linkeschova R, Rave K, Hompesch B, Sedlak M, Heise T. Time-action profile of the long-acting insulin analog insulin glargine (HOE901) in comparison with those of NPH insulin and placebo. Diabetes Care. 2000;23:644–9.
Lepore M, Pampanelli S, Fanelli C, et al. Pharmacokinetics and pharmacodynamics of subcutaneous injection of long-acting human insulin analog glargine, NPH insulin, and ultralente human insulin and continuous subcutaneous infusion of insulin lispro. Diabetes. 2000;49:2142–8.
Jinnouchi H, Koyama M, Amano A, et al. Continuous glucose monitoring during basal-bolus therapy using insulin glargine 300 U mL (− 1) and glargine 100 U mL (− 1) in Japanese people with type 1 diabetes mellitus: a crossover pilot study. Diabetes Ther. 2015;6:143–52.
Kaku K, Kakuma T, Kono S, Uchimaru H, Shiramoto M, Irie S. Pharmacokinetic and pharmacodynamic analyses on insulin glargine biosimilar in healthy male volunteers using euglycaemic clamp technique. Jpn J Dev Pharmacol Ther. 2016;44:25–34.
Rave K, Nosek L, Heinemann L, Frick A, Becker R. Time-action profile of the long-acting insulin analogue insulin glargine in comparison to NPH insulin in Japanese volunteers. Diabetes Metab. 2003;29:430–1.
Shiramoto M, Eto T, Irie S, et al. Single-dose new insulin glargine 300 U/ml provides prolonged, stable glycaemic control in Japanese and European people with type 1 diabetes. Diabetes Obes Metab. 2015;17:254–60.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38:140–9.
Levin PA. Practical combination therapy based on pathophysiology of type 2 diabetes. Diabetes Metab Syndr Obes. 2016;9:355–69.
Fritsche A, Schweitzer MA, Häring MU. Glimepiride combined with morning insulin glargine, bedtime neutral protamine hagedorn insulin, or bedtime insulin glargine in patients with type 2 diabetes. A randomized, controlled trial. Ann Intern Med. 2003;138:952–9.
Riddle MC, Rosenstock J, Gerich J. The treat-to-_target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26:3080–6.
Yki-Jarvinen H, Dressler A, Ziemen M. Less nocturnal hypoglycemia and better post-dinner glucose control with bedtime insulin glargine compared with bedtime NPH insulin during insulin combination therapy in type 2 diabetes. HOE 901/3002 Study Group. Diabetes Care. 2000;23:1130–6.
Ju H, Zhao Q, Guo Y, Sun Y, Li C, Huang H. The efficacy of treating newly diagnosed type 2 diabetes with insulin glargine combined with saxagliptin and their effects on function of β-pancreatic cells. Int J Clin Exp Med. 2016;9:4650–4.
Lee JM, Park KS, Park SH, et al. A multi-center, open, randomized, parallel-group, 2-arm study to compare the efficacy and safety of insulin add-on to glimepiride/metformin 1/500 mg b.i.d vs. to glimepiride 4 mg qd in type 2 DM patients with inadequate glycemic control. Diabetes. 2012;61:A280–1.
Moon JS, Ha KS, Yoon JS, Lee HW, Lee HC, Won KC. The effect of glargine vs glimepiride on pancreatic β-cell function in patients with type 2 diabetes uncontrolled on metformin monotherapy: open-label, randomized, controlled study. Acta Diabetol. 2014;51:277–85.
Mu PW, Chen YM, Lu HY, et al. Effects of a combination of oral anti-diabetes drugs with basal insulin therapy on β-cell function and glycaemic control in patients with newly diagnosed type 2 diabetes. Diabetes Metab Res Rev. 2012;28:236–40.
Son JW, Lee IK, Woo JT, et al. A prospective, randomized, multicenter trial comparing the efficacy and safety of the concurrent use of long-acting insulin with mitiglinide or voglibose in patients with type 2 diabetes. Endocr J. 2015;62:1049–57.
Chien MN, Lee CC, Liu SC, Chen WC, Leung CH, Wang CH. Basal insulin initiation in elderly patients with type 2 diabetes in Taiwan: a comparison with younger patients. Int J Gerontol. 2015;9:142–5.
Chien MN, Chen YL, Hung YJ, et al. Glycemic control and adherence to basal insulin therapy in Taiwanese patients with type 2 diabetes mellitus (T2D) [abstract]. Diabetes. 2014;63:A600.
Goto H, Hirose T, Shimizu S, et al. Effectiveness of combination therapy with a sulfonylurea and once-daily insulin glargine in Japanese type 2 diabetic patients—evaluation of the long-term (18 months) results of the combination therapy. J Jpn Diabetes Soc. 2007;50:591–7.
Ji L, Zhang P, Zhu D, et al. Comparative effectiveness and safety of different basal insulins in a real-world setting. Diabetes Obes Metab. 2017;19:1116–26.
Kim SS, Kim IJ, Kim YK, et al. Insulin initiation in insulin-naive Korean type 2 diabetic patients inadequately controlled on oral antidiabetic drugs in real-world practice: the modality of insulin treatment evaluation study. Diabetes Metab J. 2015;39:481–8.
Kobayashi M, Tsukube S, Ikeda Y, Shuto Y. Safety and efficacy of combination therapy with insulin glargine and oral hypoglycaemic agents including DPP-4 inhibitors in Japanese T2DM patients: ALOHA 2 Study, a post-marketing surveillance for Lantus. J Diabetes Mellitus. 2014;4:273–89.
Odawara M, Kadowaki T, Naito Y. Effectiveness and safety of basal supported oral therapy with insulin glargine, in Japanese insulin-naive, type 2 diabetes patients, with or without microvascular complications: subanalysis of the observational, non-interventional, 24-week follow-up Add-on Lantus to Oral Hypoglycemic Agents (ALOHA) study. J Diabetes Complicat. 2015;29:127–33.
Ohta A, Kato H, Murayama K, et al. Effect of insulin glargine on endogenous insulin secretion and beta-cell function in Japanese type 2 diabetic patients using oral antidiabetic drugs. Endocr J. 2014;61:13–8.
Okayama K, Goto H, Yoshihara T, et al. Effectiveness of step-up bolus insulin addition on combination therapy with sulfonylurea and once-daily insulin glargine in Japanese type 2 diabetic patients (JUN-LAN Study 7). J Jpn Diabetes Soc. 2009;52:197–202.
Suzuki D, Umezono T, Miyauchi M, et al. Effectiveness of basal-supported oral therapy (BOT) using insulin glargine in patients with poorly controlled type 2 diabetes. Tokai J Exp Clin Med. 2012;37:41–6.
Tsukube S, Kadowaki T, Odawara M. Efficacy and safety assessment of basal supported oral therapy (BOT) with insulin glargine in a real-life clinical setting, stratified by concomitant orally administered antidiabetic agent (OAD) regimens including dipeptidyl peptidase-4 inhibitor (DPP-4i): subanalysis of the ALOHA2 study, drug-use surveillance in Japan. Diabetol Int. 2016;7:299–307.
Ji L, Zhang P, Weng J, et al. Observational registry of basal insulin treatment (ORBIT) in patients with type 2 diabetes uncontrolled by oral hypoglycemic agents in China—study design and baseline characteristics. Diabetes Technol Ther. 2015;17:735–44.
Ji L, Zhang P, Zhu D, et al. Observational registry of basal insulin treatment (ORBIT) in patients with type 2 diabetes uncontrolled with oral antihyperglycaemic drugs: real-life use of basal insulin in China. Diabetes Obes Metab. 2017;19:822–30.
Wulffelé MG, Kooy A, Lehert P, et al. Combination of insulin and metformin in the treatment of type 2 diabetes. Diabetes Care. 2002;25:2133–40.
Yki-Järvinen H, Ryysy L, Nikkilä K, Tulokas T, Vanamo R, Heikkilä M. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Ann Intern Med. 1999;130:389–96.
Yang Y, Shin JA, Yang HK, et al. Reduction of sulfonylurea with the initiation of basal insulin in patients with inadequately controlled type 2 diabetes mellitus undergoing long-term sulfonylurea-based treatment. Diabetes Metab J. 2016;40:454–62.
Kawamori R, Eliaschewitz FG, Takayama H, Hayashida CY. Efficacy of insulin glargine and glimepiride in controlling blood glucose of ethnic Japanese patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2008;79:97–102.
Pratley RE, Salsali A. Inhibition of DPP-4: a new therapeutic approach for the treatment of type 2 diabetes. Curr Med Res Opin. 2007;23:919–31.
Yoshihara T, Kumashiro N, Kanazawa Y, et al. Therapeutic efficacy of mitiglinide combined with once daily insulin glargine after switching from multiple daily insulin regimen of aspart insulin and glargine in patients with type 2 diabetes mellitus. Endocr J. 2006;53:67–72.
Kumashiro N, Yoshihara T, Kanazawa Y, et al. Long-term effect of combination therapy with mitiglinide and once daily insulin glargine in patients who were successfully switched from intensive insulin therapy in short-term study. Endocr J. 2007;54:163–6.
Hilgenfeld R, Seipke G, Berchtold H, Owens DR. The evolution of insulin glargine and its continuing contribution to diabetes care. Drugs. 2014;74:911–27.
Owens DR. Optimizing treatment strategies with insulin glargine in type 2 diabetes. Expert Rev Endocrinol Metab. 2012;7:377–93.
Yki-Järvinen H, Kauppinen-Mäakelin R, Tikkainen M, et al. Insulin glargine or NPH combined with metformin in type 2 diabetes: the LANMET study. Diabetologia. 2006;49:442–51.
Bazzano LA, Lee LJ, Shi L, Reynolds K, Jackson JA, Fonseca V. Safety and efficacy of glargine compared with NPH insulin for the treatment of type 2 diabetes: a meta-analysis of randomized controlled trials. Diabet Med. 2008;25:924–32.
Home PD, Fritsche A, Schinzel S, Massi-Benedetti M. Meta-analysis of individual patient data to assess the risk of hypoglycaemia in people with type 2 diabetes using NPH insulin or insulin glargine. Diabetes Obes Metab. 2010;12:772–9.
Mullins P, Sharplin P, Yki-Jarvinen H, Riddle MC, Haring HU. Negative binomial meta-regression analysis of combined glycosylated hemoglobin and hypoglycemia outcomes across eleven phase III and IV studies of insulin glargine compared with neutral protamine Hagedorn insulin in type 1 and type 2 diabetes mellitus. Clin Ther. 2007;29:1607–19.
Kawamori R, Iwamoto Y, Kadowaki T, Iwasaki M. Efficacy and safety of insulin glargine in concurrent use with oral hypoglycemic agents for the treatment of type 2 diabetic patients. Rinsho Iyaku. 2003;19:445–64.
Wang XL, Lu JM, Pan CY, et al. Evaluation of the superiority of insulin glargine as basal insulin replacement by continuous glucose monitoring system. Diabetes Res Clin Pract. 2007;76:30–6.
Pan CY, Sinnassamy P, Chung KD, Kim KW. Insulin glargine vs NPH insulin therapy in Asian type 2 diabetes patients. Diabetes Res Clin Pract. 2007;76:111–8.
Elizarova S, Galstyan GR, Wolffenbuttel BH. Role of premixed insulin analogues in the treatment of patients with type 2 diabetes mellitus: a narrative review. J Diabetes. 2014;6:100–10.
Buse JB, Wolffenbuttel BH, Herman WH, et al. DURAbility of basal vs lispro mix 75/25 insulin efficacy (DURABLE) trial 24-week results: safety and efficacy of insulin lispro mix 75/25 vs insulin glargine added to oral antihyperglycemic drugs in patients with type 2 diabetes. Diabetes Care. 2009;32:1007–13.
Kumar A, Franek E, Wise J, Niemeyer M, Mersebach H, Simó R. Efficacy and safety of once-daily insulin degludec/insulin aspart vs insulin glargine (U100) for 52 weeks in insulin-naive patients with type 2 diabetes: a randomized controlled trial. PLoS One. 2016;11:e0163350.
Malone JK, Kerr LF, Campaigne BN, Sachson RA, Holcombe JH. Combined therapy with insulin lispro mix 75/25 plus metformin or insulin glargine plus metformin: a 16-week, randomized, open-label, crossover study in patients with type 2 diabetes beginning insulin therapy. Clin Ther. 2004;26:2034–44.
Raskin P, Allen E, Hollander P, et al. Initiating insulin therapy in type 2 Diabetes: a comparison of biphasic and basal insulin analogs. Diabetes Care. 2005;28:260–5.
Sheu WH, Ji L, Lee WJ, Jabbar A, Han JH, Lew T. Efficacy and safety of premixed insulin analogs in Asian patients with type 2 diabetes: a systematic review. J Diabetes Investig. 2017;8:518–34.
Feng SJ, Li YX. Efficacy and safety of insulin glargine combined with acarbose in the treatment of elder patients with type 2 diabetes. Chin J New Drugs. 2009;1533–4:1544.
Ji L, Min KW, Oliveira J, Lew T, Duan R. Comparison of efficacy and safety of two starting insulin regimens in non-Asian, Asian Indian, and East Asian patients with type 2 diabetes: a post hoc analysis of the PARADIGM study. Diabetes Metab Syndr Obes. 2016;9:243–9.
Onishi Y, Ono Y, Rabøl R, Endahl L, Nakamura S. Superior glycaemic control with once-daily insulin degludec/insulin aspart vs insulin glargine in Japanese adults with type 2 diabetes inadequately controlled with oral drugs: a randomized, controlled phase 3 trial. Diabetes Obes Metab. 2013;15:826–32.
Sun Y, Shao L, Niu X, et al. Clinical effectiveness of Novolin 30R vs Lantus combined with Glucobay treatment in elderly patients with type 2 diabetes mellitus controlled by oral hypoglycaemic agents: a randomized study. J Int Med Res. 2014;42:993–1001.
Tamemoto H, Ikoma A, Saitoh T, Ishikawa SE, Kawakami M. Comparison of once-daily glargine plus sulfonylurea with twice-daily 70/30 aspart premix in insulin-naive Japanese patients with diabetes. Diabetes Technol Ther. 2007;9:246–53.
Yang W, Xu X, Liu X, et al. Treat-to-_target comparison between once daily biphasic insulin aspart 30 and insulin glargine in Chinese and Japanese insulin-naïve subjects with type 2 diabetes. Curr Med Res Opin. 2013;29:1599–608.
Jeong I-K, Chung CH, Zhou Z, et al. Comparison of insulin intensification strategies with insulin lispro low mixture twice daily vs basal insulin glargine and prandial insulin lispro once daily in East Asian and Caucasian patients with type 2 diabetes mellitus. J Diabetes. 2017;9:396–404.
Jia W, Xiao X, Ji Q, et al. Comparison of thrice-daily premixed insulin (insulin lispro premix) with basal-bolus (insulin glargine once-daily plus thrice-daily prandial insulin lispro) therapy in east Asian patients with type 2 diabetes insufficiently controlled with twice-daily premixed insulin: an open-label, randomised, controlled trial. Lancet Diabetes Endocrinol. 2015;3:254–62.
Jin SM, Kim JH, Min KW, et al. Basal-prandial vs premixed insulin in patients with type 2 diabetes requiring insulin intensification after basal insulin optimization: a 24-week randomized non-inferiority trial. J Diabetes. 2016;8:405–13.
Marso SP, McGuire DK, Zinman B, et al. Efficacy and safety of degludec vs glargine in type 2 diabetes. N Engl J Med. 2017;377:723–32.
Ritzel R, Roussel R, Bolli GB, et al. Patient-level meta-analysis of the EDITION 1, 2 and 3 studies: glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml vs glargine 100 U/ml in people with type 2 diabetes. Diabetes Obes Metab. 2015;17:859–67.
Vora J, Christensen T, Rana A, Bain SC. Insulin degludec vs insulin glargine in type 1 and type 2 diabetes mellitus: a meta-analysis of endpoints in phase 3a trials. Diabetes Ther. 2014;5:435–46.
Wysham C, Bhargava A, Chaykin L, et al. Effect of insulin degludec vs insulin glargine U100 on hypoglycemia in patients with type 2 diabetes: the SWITCH 2 randomized clinical trial. JAMA. 2017;318:45–56.
Terauchi Y, Koyama M, Cheng X, et al. New insulin glargine 300 U/ml vs glargine 100 U/ml in Japanese people with type 2 diabetes using basal insulin and oral antihyperglycaemic drugs: glucose control and hypoglycaemia in a randomized controlled trial (EDITION JP 2). Diabetes Obes Metab. 2016;18:366–74.
Osonoi T, Onishi Y, Nishida T, Hyllested-Winge J, Iwamoto Y. Insulin degludec vs insulin glargine, both once daily as add-on to existing orally administered antidiabetic drugs in insulin-naive Japanese patients with uncontrolled type 2 diabetes: subgroup analysis of a pan-Asian, treat-to-_target phase 3 trial. Diabetol Int. 2016;7:141–7.
Yki-Järvinen H, Bergenstal R, Ziemen M, et al. New insulin glargine 300 units/mL vs glargine 100 units/mL in people with type 2 diabetes using oral agents and basal insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 2). Diabetes Care. 2014;37:3235–43.
Bolli GB, Riddle MC, Bergenstal RM, et al. New insulin glargine 300 U/ml compared with glargine 100 U/ml in insulin-naive people with type 2 diabetes on oral glucose-lowering drugs: a randomized controlled trial (EDITION 3). Diabetes Obes Metab. 2015;17:386–94.
Bolli GB, Riddle MC, Bergenstal RM, Wardecki M, Goyeau H, Home PD. Glycaemic control and hypoglycaemia with insulin glargine 300U/mL vs insulin glargine 100U/mL in insulin-naïve people with type 2 diabetes: 12-month results from the EDITION 3 trial. Diabetes Metab. 2017;43:351–8.
Aso Y, Suzuki K, Chiba Y, et al. Effect of insulin degludec vs insulin glargine on glycemic control and daily fasting blood glucose variability in insulin-naive Japanese patients with type 2 diabetes: I’D GOT trial. Diabetes Res Clin Pract. 2017;130:237–43.
Abd El Aziz MS, Kahle M, Meier JJ, Nauck MA. A meta-analysis comparing clinical effects of short- or long-acting GLP-1 receptor agonists vs insulin treatment from head-to-head studies in type 2 diabetic patients. Diabetes Obes Metab. 2017;19:216–27.
Wysham CH, Lin J, Kuritzky L. Safety and efficacy of a glucagon-like peptide-1 receptor agonist added to basal insulin therapy vs basal insulin with or without a rapid-acting insulin in patients with type 2 diabetes: results of a meta-analysis. Postgrad Med. 2017;129:436–45.
Jones AG, McDonald TJ, Shields BM, et al. Markers of β-cell failure predict poor glycemic response to GLP-1 receptor agonist therapy in type 2 diabetes. Diabetes Care. 2016;39:250–7.
Araki E, Inagaki N, Tanizawa Y, Oura T, Takeuchi M, Imaoka T. Efficacy and safety of once-weekly dulaglutide in combination with sulphonylurea and/or biguanide compared with once-daily insulin glargine in Japanese patients with type 2 diabetes: a randomized, open-label, phase III, non-inferiority study. Diabetes Obes Metab. 2015;17:994–1002.
Inagaki N, Atsumi Y, Oura T, Saito H, Imaoka T. Efficacy and safety profile of exenatide once weekly compared with insulin once daily in Japanese patients with type 2 diabetes treated with oral antidiabetes drug(s): results from a 26-week, randomized, open-label, parallel-group, multicenter, noninferiority study. Clin Ther. 2012;34:1892–908.
Seino Y, Min KW, Niemoeller E, Takami A. Randomized, double-blind, placebo-controlled trial of the once-daily GLP-1 receptor agonist lixisenatide in Asian patients with type 2 diabetes insufficiently controlled on basal insulin with or without a sulfonylurea (GetGoal-L-Asia). Diabetes Obes Metab. 2012;14:910–7.
Seino Y, Kaneko S, Fukuda S, et al. Combination therapy with liraglutide and insulin in Japanese patients with type 2 diabetes: a 36-week, randomized, double-blind, parallel-group trial. J Diabetes Investig. 2016;7:565–73.
Kaneko S, Oura T, Matsui A, Shingaki T, Takeuchi M. Efficacy and safety of subgroup analysis stratified by baseline HbA1c in a Japanese phase 3 study of dulaglutide 0.75 mg compared with insulin glargine in patients with type 2 diabetes. Endocr J. 2017;64:1165–72.
Kanazawa Y, Igarashi Y, Komiya K, et al. Long-term efficacy of insulin glargine after switching from NPH insulin as intensive replacement of basal insulin in Japanese diabetes mellitus. Comparison of efficacy between type 1 and type 2 diabetes (JUN-LAN Study 1.2). Endocr J. 2007;54:975–83.
Suzuki D, Toyoda M, Kondo M, et al. Efficacy of long-acting insulin analog insulin glargine at high dosage for basal-bolus insulin therapy in patients with type 2 diabetes. Tokai J Exp Clin Med. 2012;37:35–40.
Yokoyama H, Tada J, Kamikawa F, Kanno S, Yokota Y, Kuramitsu M. Efficacy of conversion from bedtime NPH insulin to morning insulin glargine in type 2 diabetic patients on basal-prandial insulin therapy. Diabetes Res Clin Pract. 2006;73:35–40.
Bu S, Guo XH, Yang WY, et al. Post-hoc analyses of type 2 diabetes patients switch from premixed insulin regimen to basal insulin plus oral hypoglycemic agents regimen. Zhonghua Yi Xue Za Zhi. 2007;87:3115–8.
Shigihara N, Tamaki M, Goto H, et al. Efficacy and safety of switching from premix twice daily injection to sulfonylurea and once daily insulin glargine in Japanese type 2 diabetes (JUN-LAN Study 8). J Jpn Diabetes Soc. 2010;53:157–61.
Takahashi H, Sakai K, Kawanishi K, et al. Efficacy of switching from premix analog insulin twice daily injection to insulin glargine once daily injection with sitagliptin. Diabetetol Int. 2015;6:33–8.
Umezono T, Suzuki D, Kuriyama Y, et al. Long-term glycemic control in Japanese type 2 diabetes patients after switching treatment from twice-daily premixed insulin to once daily insulin glargine. Tokai J Exp Clin Med. 2013;38:28–32.
Yang W, Lv X, Li Q, Jia W, Tian H. A prospective study to optimize insulin treatment by switching to insulin glargine in type 2 diabetic patients previously uncontrolled on premixed insulin: the optimization study. Curr Med Res Opin. 2012;28:533–41.
Zhang B, Zhao J, Yang W. Glycemic control and safety in Chinese patients with type 2 diabetes mellitus who switched from premixed insulin to insulin glargine plus oral antidiabetics: a large, prospective, observational study. Diabetes Metab Res Rev. 2017;33:e2863.
Zhang Y, Xie YJ, Meng DD, Zhang HH, Chen H, Liu E. Clinical study of treatment switching from premixed insulin to basal insulin combined with oral hypoglycemic drugs in patients with type 2 diabetes. Diabetol Metab Syndr. 2014;6:37.
Takahara M, Shiraiwa T, Kaneto H, Katakami N, Matsuoka TA, Shimomura I. Efficacy of sitagliptin on blood glucose fluctuation in Japanese type 2 diabetic patients with basal-supported oral therapy. Endocr J. 2012;59:1131–6.
Taniguchi M, Tamura M. A multicenter open-label, single-arm, 24-week phase IV study evaluating the effectiveness and safety of treatment of insulin glargine in type 2 diabetes mellitus following glucagon-like peptide-1 (GLP-1) failure (GAUDI Study). Rinsho Iyaku. 2015;9:843–56.
Kadowaki T, Ohtani T, Naito Y, Odawara M. Potential formula for the calculation of starting and incremental insulin glargine doses: ALOHA subanalysis. PLoS One. 2012;7:e41358.
Ohtani T, Ito T. Safety and effectiveness of BOT (Basal supported Oral Therapy) using insulin glargine in Japanese patients with type 2 diabetes-results from post-marketing surveillance of insulin glargine (ALOHA study). Shinyaku To Rinsho (J New Rem Clin). 2011;60:458–75.
Kadowaki T, Ohtani T, Odawara M. Baseline predictive factors for glycemic control in Japanese type 2 diabetes patients treated with insulin glargine plus oral antidiabetic drugs: ALOHA study subanalysis. Diabetol Int. 2013;4:16–22.
Ikeda Y, Tsukube S, Kadowaki T, Odawara M. Predictors for achieving _target glycemic control in Japanese patients with type 2 diabetes after initiation of basal supported oral therapy using insulin glargine: sub-analysis of the ALOHA2 study, drug use surveillance in Japan. Diabetol Int. 2016;7:188–98.
Odawara M, Ohtani T, Kadowaki T. Dosing of insulin glargine to achieve the treatment _target in Japanese type 2 diabetes on a basal supported oral therapy regimen in real life: ALOHA study subanalysis. Diabetes Technol Ther. 2012;14:635–43.
Odawara M, Kadowaki T, Naito Y. Plasma glucose monitoring and the subsequent HbA1c control in patients with type 2 diabetes on a basal supported oral therapy regimen in real life: subanalysis of the ALOHA study: a 24-week, prospective, open-label, multicenter, observational study. Diabetol Int. 2015;6:66–76.
Odawara M, Kadowaki T, Naito Y. Incidence and predictors of hypoglycemia in Japanese patients with type 2 diabetes treated by insulin glargine and oral antidiabetic drugs in real-life: ALOHA post-marketing surveillance study sub-analysis. Diabetol Metab Syndr. 2014;6:20.
Brown A, Guess N, Dornhorst A, Taheri S, Frost G. Insulin-associated weight gain in obese type 2 diabetes mellitus patients: what can be done? Diabetes Obes Metab. 2017;19:1655–68.
The Diabetes Association of the Republic of China (Taiwan). Taipei, Taiwan, ROC: DAROC; 2018. DAROC clinical practice guidelines for diabetes care—2018. http://www.endo-dm.org.tw/dia/direct/. Accessed 27 Jul 2018.
Japan Diabetes Society. Treatment guide for diabetes 2014–2015. Tokyo: JDS; 2017.
Korean Diabetes Association. 2015 treatment guidelines for diabetes. Seoul: KDA; 2017.
Weng J, Ji L, Jia W, et al. Standards of care for type 2 diabetes in China. Diabetes Metab Res Rev. 2016;32:442–58.
Tsai ST, Pathan F, Ji L, et al. First insulinization with basal insulin in patients with type 2 diabetes in a real-world setting in Asia. J Diabetes. 2011;3:208–16.
Ishii H, Iwamoto Y, Tajima N. An exploration of barriers to insulin initiation for physicians in Japan: findings from the diabetes attitudes, wishes and needs (DAWN) JAPAN study. PLoS One. 2012;7:e36361.
Garg SK, Admane K, Freemantle N, et al. Patient-led vs physician-led titration of insulin glargine in patients with uncontrolled type 2 diabetes: a randomized multinational ATLAS study. Endocr Pract. 2015;21:143–57.
Chan JCN, Bunnag P, Chan SP, et al. Glycaemic responses in Asian and non-Asian people with type 2 diabetes initiating insulin glargine 100units/mL: a patient-level pooled analysis of 16 randomised controlled trials. Diabetes Res Clin Pract. 2018;135:199–205.
Tamaki M, Shimizu T, Kanazawa A, et al. Effects of changes in basal/total daily insulin ratio in type 2 diabetes patients on intensive insulin therapy including insulin glargine (JUN-LAN Study 6). Diabetes Res Clin Pract. 2008;81:e1–3.
Abrahamson MJ, Peters A. Intensification of insulin therapy in patients with type 2 diabetes mellitus: an algorithm for basal-bolus therapy. Ann Med. 2012;44:836–46.
Araki E, Onishi Y, Asano M, Kim H, Yajima T. Efficacy and safety of dapagliflozin over 1 year as add-on to insulin therapy in Japanese patients with type 2 diabetes: the DAISY (Dapagliflozin Added to patients under InSulin therapY) trial. Diabetes Obes Metab. 2017;19:562–70.
Inagaki N, Harashima S, Maruyama N, Kawaguchi Y, Goda M, Iijima H. Efficacy and safety of canagliflozin in combination with insulin: a double-blind, randomized, placebo-controlled study in Japanese patients with type 2 diabetes mellitus. Cardiovasc Diabetol. 2016;15:89.
Ishihara H, Yamaguchi S, Nakao I, Okitsu A, Asahina S. Efficacy and safety of ipragliflozin as add-on therapy to insulin in Japanese patients with type 2 diabetes mellitus (IOLITE): a multi-centre, randomized, placebo-controlled, double-blind study. Diabetes Obes Metab. 2016;18:1207–16.
Araki E, Haneda M, Kasuga M, et al. New glycemic _targets for patients with diabetes from the Japan Diabetes Society. J Diabetes Investig. 2017;8:123–5.
Acknowledgements
Funding
This manuscript, all writing assistance, and journal processing charges were funded by Eli Lilly and Company. All authors had full access to the articles reviewed in this manuscript and take complete responsibility for the integrity and accuracy of this manuscript.
Medical Writing Assistance
Writing assistance with early drafts of this manuscript was provided by Luke Carey, PhD, and Tania Dickson, PhD, of ProScribe—Envision Pharma Group. Writing assistance with later drafts of this manuscript was provided by Michelle A. Carey, PhD, of Syneos Health.
Authorship
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their permission for this version to be published.
Disclosures
Takahisa Hirose has received honoraria from Ono Pharmaceutical Co. Ltd., Sanofi K.K., Sumitomo Dainippon Pharma Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., AstraZeneca K.K., Novo Nordisk Pharma Ltd., Takeda Pharmaceutical Company Ltd., Eli Lilly Japan K.K., MSD K.K. and research funding from Mitsubishi Tanabe Pharma Corporation, Astra Zeneca K.K., Takeda Pharmaceutical Company Ltd., Eli Lilly, Sanofi K.K., Novo Nordisk, Boehringer Ingelheim, Ono Pharmaceutical Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Kissei Pharmaceutical Co., Ltd, and MSD. Ching-Chu Chen has served on an advisory panel for Novo Nordisk, Eli Lilly, Boehringer Ingelheim, Sanofi, Takeda, AstraZeneca and has been a member of speakers bureaus for Merck Sharp & Dohme, Eli Lilly, Boehringer Ingelheim, Sanofi and AstraZeneca. Kyu Jeung Ahn has served on an advisory panel for Eli Lilly, Takeda, AstraZenaca, Merck, JW Pharmaceutical, and research funding from Novo Nordisk, Daiichi Sankyo, Daewoong Pharmaceutical, Dong-A ST, Dongwha, Eli Lilly, Boehringer Ingelheim, BMS, Sanofi, Astellas, AstraZeneca, Janssen, LG Chem, MSD, Otsuka, Korea United Pharm, Yuhan, Ildong Pharmaceutical, CKD, Handok, Hanmi Pharmaceutical and JW Pharmaceutical. Jacek Kiljański is an employee and stockholder of Eli Lilly.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new results of studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7907873.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hirose, T., Chen, CC., Ahn, K.J. et al. Use of Insulin Glargine 100 U/mL for the Treatment of Type 2 Diabetes Mellitus in East Asians: A Review. Diabetes Ther 10, 805–833 (2019). https://doi.org/10.1007/s13300-019-0613-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-0613-7