Abstract
Introduction and hypothesis
We performed a review of the literature reporting on the effects of pelvic floor muscle training (PFMT) on female sexual function (SF).
Methods
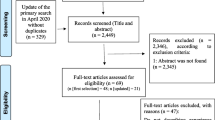
Pubmed (from 1946 to December 2014), Ovid Medline (from 1946 to December 2014), CINAHL (from 1937 to December 2014), PsycINFO (from 1805 to December 2014), Scopus and Cochrane Central Register of Controlled Trials were searched by two independent reviewers. Randomised controlled trials (RCTs) investigating the impact of PFMT on women’s SF published in English were included. Methodological quality was scored using the PEDro scale. Data were analysed qualitatively and interpreted.
Results
A total of 1341 women were included in the eight RCTs covered by this review. The studies were published between 1997 and 2014. Methodological scores were between 4 and 7. The sample included derived from heterogeneous populations of women. In only one study was SF the primary outcome measure. Pelvic floor dysfunction was an inclusion criterion in the majority of studies. Most studies reported a significant improvement in SF score after PFMT between control and intervention groups.
Conclusions
Although most studies indicated an improvement of at least one sexual variable in women with pelvic floor dysfunction, and one study demonstrated an improvement in SF in postpartum women selected independently of their continence status, the results need to be interpreted with caution. High-quality RCTs specifically designed to investigate the impact of PFMT on women’s SF are required.

Similar content being viewed by others
References
Abdo CH, Oliveira WM Jr, Moreira ED Jr, Fittipaldi JA (2004) Prevalence of sexual dysfunctions and correlated conditions in a sample of Brazilian women–results of the Brazilian study on sexual behavior (BSSB). Int J Impot Res 16:160–166
Nobre JP, Pinto-Gouveia J (2006) Dysfunctional sexual beliefs as vulnerability factors for sexual dysfunction Universidade de Coimbra, Portugal. J Sex Res 43:68–75
Clayton AH, Dennerstein L, Fisher WA, Kingsberg SA, Perelman MA, Pyke RE (2010) Standards for clinical trials in sexual dysfunction in women: research designs and outcomes assessment. J Sex Med 7:541–560
Lewis RW, Fugl-Meyer KS, Corona G, Hayes RD, Laumann EO, Moreira ED et al (2010) Definitions/epidemiology/risk factors for sexual dysfunction. J Sex Med 7:1598–1607
Knoepp LR, Shippey SH, Chen CC, Cundiff GW, Derogatis LR, Handa VL (2010) Sexual complaints, pelvic floor symptoms, and sexual distress in women over forty. J Sex Med 7:3675–3682
Pontiroli AE, Cortelazzi D, Morabito A (2013) Female sexual dysfunction and diabetes: a systematic review and meta-analysis. J Sex Med 10(4):1044–1051
Ibrahim ZM, Ahmed MR, Sayed Ahmed WA (2013) Prevalence and risk factors for female sexual dysfunction among Egyptian women. Arch Gynecol Obstet 87:1173–1180
Diehl A, da Silva R, Laranjeira R (2013) Female sexual dysfunction in patients with substance-related disorders. Clinics 68:205–211
Dumoulin C, Hunter KF, Moore K, Bradley CS, Burgio KL, Hagen S, Imamura M, Thakar R, Williams K, Chambers T (2014) Conservative management for female urinary incontinence and pelvic organ prolapse review 2013: Summary of the 5th international consultation on incontinence. Neurourol Urodyn. doi:10.1002/nau.22677
Bø K, Talseth T, Vinsnes A (2000) Randomized controlled trial on the effect of pelvic floor muscle training on quality of life and sexual problems in genuine stress incontinent women. Acta Obstet Gynecol Scand 79:598–603
Handa VL, Whitcomb E, Weidner AC, Nygaard I, Brubaker L, Bradley CS, Paraiso MF, Schaffer J, Zyczynski HM, Zhang M, Richter HE (2011) Sexual function before and after non-surgical treatment for stress urinary incontinence. Female Pelvic Med Reconstr Surg 17:30–35
Liebergall-Wischnitzer M, Paltiel O, Hochner Celnikier D, Lavy Y, Manor O, Woloski Wruble AC (2012) Sexual function and quality of life of women with stress urinary incontinence: a randomized controlled trial comparing the Paula method (circular muscle exercises) to pelvic floor muscle training (PFMT) exercises. J Sex Med 9:1613–1623
Eftekhar T, Sohrabi M, Haghollahi F, Shariat M, Miri E (2014) Comparison effect of physiotherapy with surgery on sexual function in patients with pelvic floor disorder: A randomized clinical trial. Iran J Reprod Med 12:7–14
Braekken IH, Majida M, Ellström Engh M, Bø K (2015) Can Pelvic Floor Muscle Training Improve Sexual Function in Women with Pelvic Organ Prolapse? A Randomized Controlled Trial. J Sex Med 12:470–480
Hagen S, Stark D, Glazener C, Dickson S, Barry S, Elders A, Frawley H, Galea MP, Logan J, McDonald A, McPherson G, Moore KH, Norrie J, Walker A, Wilson D (2014) POPPY Trial Collaborators. Individualised pelvic floor muscle training in women with pelvic organ prolapse (POPPY): a multicentre randomised controlled trial. Lancet 383:796–806
Kegel A (1952) Sexual functions of the pubococcygeus muscle. West J Surg Obstet Gynecol 60:521–524
Shafik A (2000) The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 11:361–376
Graber B, Kline-Graber G (1979) Female orgasm: role of pubococcygeus muscle. J Clin Psychiatry 40:348–351
Ma Y, Qin H (2009) Pelvic floor muscle exercises may improve female sexual function. Med Hypotheses 72:223
Willans A (2014) The role of pelvic floor muscle exercise in the treatment of female sexual dysfunction. J Assoc Chart Physiotherapists Women’s Health 115:22–29
Howick J, Chalmers I, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I,Phillips B, Thornton H, Goddard O, Hodgkinson M. The Oxford Levels of Evidence 2″. Oxford Centre for Evidence-Based Medicine. http://www.cebm.net/index.aspx?o=5653
Macedo LG, Elkins MR, Maher CG, Moseley AM, Herbert RD, Sherrington C (2010) There was evidence of convergent and construct validity of Physiotherapy Evidence Database quality scale for physiotherapy trials. J Clin Epidemiol 63:920–925
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Wilson PD, Herbison GP (1998) A randomized controlled trial of pelvic floor muscle exercises to treat postnatal urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 9:257–264
Citak N, Cam C, Arslan H, Karateke A, Tug N, Ayaz R, Celik C (2010) Postpartum sexual function of women and the effects of early pelvic floor muscle exercises. Acta Obstet Gynecol Scand 89:817–822
Yang EJ, Lim JY, Rah UW, Kim YB (2012) Effect of a pelvic floor muscle training program on gynecologic cancer survivors with pelvic floor dysfunction: a randomized controlled trial. Gynecol Oncol 125:705–711
Patrick DL, Martin ML, Bushnell DM, Yalcin I, Wagner TH, Buesching DP (1999) Quality of life of women with urinary incontinence: further development of the incontinence quality of life instrument (I-QOL). Urology 53(1):71–6.
Rust J, Golombok S (1986) The GRISS: a psychometric instrument for the assessment of sexual dysfunction. Arch Sex Behav 15:157–165
Dennerstein L, Anderson-Hunt M, Dudley E (2002) Evaluation of a short scale to assess female sexual functioning. J Sex Marital Ther 28:389–397
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P (1996) The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. Br J Urol 77:805–812
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2004) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J Pelvic Floor Dysfunct 15:219
Baessler K, O’Neill SM, Maher CF, Battistutta D (2009) Australian pelvic floor questionnaire: a validated interviewer-administered pelvic floor questionnaire for routine clinic and research. Int Urogynecol J Pelvic Floor Dysfunct 20:149–158
Mouritsen L, Larsen JP (2003) Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 14:122–127
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376
Laycock J et al (1994) Clinical evaluation of the pelvic floor. In: Pelvic Floor Re-education, 1st edn. Springer-Verlag, London, pp 42–48
Brink CA, Sampselle CM, Wells TJ, Diokno AC, Gillis GL (1989) A digital test for pelvic muscle strength in older women with urinary incontinence. Nurs Res 38:196–199
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16:139–144
Van Brummen HJ, Bruinse HW, van de Pol G, Heintz AP, van der Vaart CH (2007) The effect of vaginal and cesarean delivery on lower urinary tract symptoms: what makes the difference? Int Urogynecol J Pelvic Floor Dysfunct 18:133–139
Wesnes SL, Hunskaar S, Bo K, Rortveit G (2009) The effect of urinary incontinence status during pregnancy and delivery mode on incontinence postpartum. A cohort study. BJOG 116:700–707
Brown S, Gartland D, Perlen S, McDonald E, MacArthur C (2014) Consultation about urinary and faecal incontinence in the year after childbirth: a cohort study. BJOG. doi:10.1111/1471-0528.12963
Weber AM, Walters MD, Schover LR, Mitchinson A (1995) Sexual function in women with uterovaginal prolapse and urinary incontinence. Obstet Gynecol 85:483–487
Lukacz ES, Whitcomb EL, Lawrence JM, Nager CW, Contreras R, Luber KM (2007) Are sexual activity and satisfaction affected by pelvic floor disorders? Analysis of a community-based survey. Am J Obstet Gynecol 197:88.e1–6
De Souza A, Dwyer PL, Rosamilia A, Hiscock R, Lim YN, Murray C, Thomas E, Conway C, Schierlitz L (2012) Sexual function following retropubic TVT and transobturator Monarc sling in women with intrinsic sphincter deficiency: a multicentre prospective study. Int Urogynecol J 23:153–158
Schoenfeld M, Fuermetz A, Muenster M, Ennemoser S, von Bodungen V, Friese K, Jundt K (2013) Sexuality in German urogynecological patients and healthy controls: is there a difference with respect to the diagnosis? Eur J Obstet Gynecol Reprod Biol 170:567–570
Lowenstein L, Gruenwald I, Gartman I, Vardi Y (2010) Can stronger pelvic muscle floor improve sexual function? Int Urogynecol J 21:553–556
Martinez CS, Ferreira FV, Castro AA, Gomide LB (2014) Women with greater pelvic floor muscle strength have better sexual function. Acta Obstet Gynecol Scand 93:497–502
Latif EZ, Diamond MP (2013) Arriving at the diagnosis of female sexual dysfunction. Fertil Steril 100:898–904
Basson R (2005) Women’s sexual dysfunction: revised and expanded definitions. CMAJ 172:1327–1333
Basson R, Berman J, Burnett A et al (2000) Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol 163(3):888–893
Roughan PA, Kunst L (1981) Do pelvic floor exercises really improve orgasmic potential? J Sex Marital Ther 7:223–229
Trudel G, Saint-Laurent S (1983) A comparison between the effects of Kegel’s exercises and a combination of sexual awareness relaxation and breathing on situational orgasmic dysfunction in women. J Sex Marital Ther 9:204–209
Lara LA, Montenegro ML, Franco MM, Abreu DC, Rosa e Silva AC, Ferreira CH (2012) Is the sexual satisfaction of postmenopausal women enhanced by physical exercise and pelvic floor muscle training? J Sex Med 9:218–223
Acknowledgments
We thank all Urogynecology Department staff of the Mercy Hospital for Women, Melbourne, VIC, Australia and especially to Christine Murray and Elizabeth Thomas.
Funding
The first author received a scholarship from São Paulo Research Foundation (FAPESP- 2012/215239).
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferreira, C.H.J., Dwyer, P.L., Davidson, M. et al. Does pelvic floor muscle training improve female sexual function? A systematic review. Int Urogynecol J 26, 1735–1750 (2015). https://doi.org/10.1007/s00192-015-2749-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2749-y