Abstract
Introduction
In an ageing society, older adults are the main users of healthcare services, and Chinese healthcare systems have been struggling to meet the care demand of older adults. Due to the illness, many older inpatients cannot finish daily activities independently and require healthcare from caregivers. Evaluating the care needs of older adults and exploring the factors affecting safe care at multiple levels are conducive to providing systematic care services for older inpatients. This study aims to examine which and how factors impact safe care for older inpatients and propose a safe care theory to provide directions on improving the safe care system in the hospital.
Methods and analysis
A mixed-methods study with three interrelated research streams will be designed. (1) A safe care concept model: we will conduct a scoping review to extract the facilitators and barriers influencing the safe care of older inpatients and construct a concept model based on the socio-ecological model and the Yorkshire Contributory Factors Framework. (2) A safe care theory model: we will conduct a qualitative study with thematic analysis (aimed at older inpatients, caregivers and nurses) to define the concept connotations and propose a theory model. (3) A safe care theory: we will use the scales related to the theory model to test the concepts and statements. We will revise the theory model and derive a safe care theory based on the mixed-methods study results. This study will start in October 2023 and end in October 2025.
Ethics and dissemination
This study was approved by the ethics committee (No. 20221598). All participants will be provided with consent forms prior to data collection. The study will be disseminated via peer-reviewed manuscripts and conferences.
Trial registration number
ChiCTR2300067421.
Keywords: Aged, Aging, Patient-Centered Care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This exploratory study uses a mixed method to gather data from various perspectives to construct a safe care theory.
Using mixed-methods study ensures that quantitative and qualitative data are applied to mutual validation, thereby enhancing the credibility of the study findings.
This protocol has been designed using a concept, statement and theory derivation strategy proposed by Walker and Avant on the exploration of theory.
As this is a theory exploration study, there may be a lack of practical evidence for some specific concepts and connections.
Introduction
China has entered a period of ageing population. Older adults (65 years or older) made up 13.5% of the Chinese population in 2020, and this proportion might triple over the next 30 years.1 The difficult situation of ageing brought great challenges to medical care. In China, the prevalence of chronic diseases in older adults is high, and approximately 78% of the older suffer from at least one chronic disease.2 Repeated admissions and prolonged lengths of hospitalisation have become a major economic burden for older patients and their families. Older inpatients were often unable to independently complete daily activities due to their illness and special physical conditions, so adverse events were more likely to occur when care was poor.3
During the hospitalisation of older patients, common adverse events included medication errors, falls, pressure ulcers and aspiration pneumonia.4 5 The risk assessment tools and corresponding intervention schemes for adverse events were conducive to guaranteeing the physiological safety of older inpatients. The extensive application of anxiety, depression, suicide and other related scales also helped healthcare teams to identify the mental state of older inpatients. However, physiological and psychological care, environmental comfort, and cultural safety were complex ecosystems that were interconnected and constantly functioning.5 6 As the centre of ecosystems, older inpatients need to build an active connection with the surrounding groups and finally achieve the ecosystems’ harmonious development. Currently, Chinese healthcare institutions need a theory to guide the clinical care practice of older inpatients. This theory should focus on developing care services in multiple aspects, enriching the conceptual connotations of safe care and optimising hospital care systems to ensure the safety of older inpatients.
The classical Watson human caring theory highlighted that caring is the essence of nursing and the psychological healing of the patients.7 Consequently, psychological care is an essential part of patient safety care. Silverglow et al 8 found that feeling safe had a positive impact on older adults’ diseases. Improving the sense of security of older inpatients should start by ensuring care safety. Based on the existing research on patient safety, Chinese hospitals have taken some measures to control potential safety factors and patient safety has been deeply rooted in the minds of the healthcare staff.9 Nevertheless, hospital care systems still lack practice theory since there are multiple cooperative stakeholders and complex factors in safe care.
In China, research on the safe care of older inpatients at the theory level needs to be improved, and there is no safe care theory based on Chinese guidelines, policies and general conditions. Constructing a theory can provide a perspective to screen and explain core ideas about the essence of practice, and the essence can also be explored through theory construction.10 Walker introduced the derivation strategy to create a theory that fitted with conditions where theoretical research did not exist or needed to be updated.10 Through the concept, statement and theory derivation strategy, the safe care theory can be constructed in a systematic process, and the subsequent research can be designed to enrich the theory connotations and validate the theory statements. For the framework of safe care theory and practice, existing research explored the building blocks from the perspective of the socio-ecological model (SEM) and the Yorkshire Contributory Factors Framework (YCFF), which provided valuable insights into subsequent research.
Social ecology emphasised that health conditions were related to the interplay of individuals and the environment.11 Some studies categorised the factors associated with healthy ageing and clarified the interactions of the factors based on the SEM, which confirmed that personal characteristics and the environmental conditions should be considered for safe care.12 13 Furthermore, Lawton et al 14 summarised a taxonomy of the factors contributing to patient safety issues by a systematic review, the YCFF. Based on the YCFF, Giles et al 15 developed a patient measure of safety, which testified that patients could identify factors contributing to the safety of their care. Using the SEM and the YCFF as a starting point, this study will generate a theoretical framework guiding the patient safety care practice from multiple dimensions.
Safe care of older inpatients is a complex pathway requiring healthcare professionals to thoroughly understand the interplay between the older and their surrounding environment. Previous research mainly focused on detecting factors from the single perspective of individuals or caregivers and comparing the effects of intervention schemes. Little is known about which theoretical mechanisms best direct safe care in the hospital. The depth of theoretical research and the theoretical understanding level of practitioners largely determine the effectiveness of care decisions and medical behaviours. Therefore, building on the SEM and the YCFF, a mixed-methods study with three inter-related research streams (a safe care concept model, a safe care theory model and a safe care theory) will be designed. This study aims to develop a safe care theory for older inpatients by combining quantitative and qualitative research. We believe the theory will guide further research to assist in optimising and upgrading the quality of older care services.
Theoretical framework
Our project will be guided by the SEM and the YCFF. Although there are many theoretical frameworks, we choose the YCFF as it is rooted in a systematic literature review and has been used to identify factors affecting patient safety. SEM has also been widely used in the health field.
In the 1970s, Bronfenbrenner introduced the ecological theory, revised over time to depict the nested circles of systems and related factors influencing an individual’s behaviour and health.11 Subsequently, disease ecology, health ecology and social ecology were derived. Among them, SEM has been successfully used in health research to interpret the complex influencing mechanism on individuals and their surrounding environment. Litchfield et al 16 unpicked the complicated factors of safe care practice by the SEM, including individual factors: responsibility and experience; interpersonal factors: communication and support; organisational factors: infrastructure and practice; community factors: the health profile of patients; and policy factors. Tan et al 17 conducted a scoping review to summarise the factors affecting the adoption of teledentistry among older adults based on the SEM, involving individual level: knowledge, attitudes and practices; organisational level: care settings and administration; community level: resources and support; and policy level: data privacy and regulations. Besides, existing research explored facilitators and barriers related to human health from the perspective of the SEM.18 19
Our study will use the SEM to organise the factors/concepts/contents affecting the safe care of older inpatients on the individual, interpersonal, environmental and policy levels. The definition of each ecological level is as follows: (1) Individual level: personal characteristics (eg, age, primary diseases, factors related to individual health, socioeconomic status). (2) Interpersonal level: interactions with people who influence individual health. (3) Environmental level: the hospital environment (eg, the hospital settings and infrastructure). (4) Policy level: safe culture, hospital norms, policy and accessibility of services. An adapted version of the SEM for our study is shown in figure 1.
Figure 1.
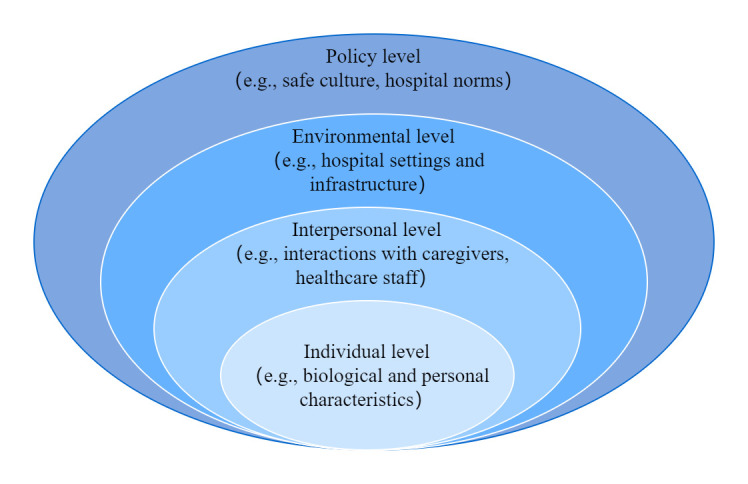
An adapted version of the socio-ecological model.
In 2012, Lawton et al 14 published the YCFF based on a synthesis of evidence-based work, which generated factors contributing to patient safety incidents. The YCFF included five contributing factors: active failures, situational factors, local working conditions, latent/organisational factors and latent/external factors. Currently, the YCFF has been applied to identify and categorise factors that cause harm to inpatients. Albalawi et al 20 categorised factors affecting patient safety culture in Saudi Arabia, containing strength and weakness factors. In addition, Albutt et al 21 conducted a qualitative study to investigate healthcare professionals’ perceptions of patient safety incidents in psychological care. The interview data were analysed based on the YCFF, and the results provided valuable insights into creating interventions to improve patient safety. Building on the core elements of the YCFF, our study will extract the factors related to safe care, classify the factors and define the concepts.
Methods
Overview of study design
Our project is divided into three sequential stages following the concept, statement and theory derivation strategy.
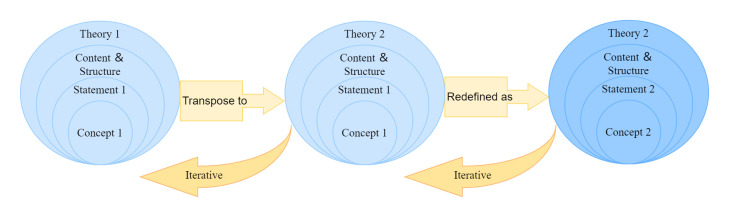
Stage 1 (A safe care concept model): A scoping review will be conducted to extract the factors (facilitators and barriers) influencing the safe care of older inpatients. Next, the inductive and deductive methods will be used to analyse the extracted information and explore critical themes in safe care based on the SEM and the YCFF. Metaphor or analogy is the core of derivation, and we will transpose and redefine a concept or a statement from one field or context to another through the derivation strategy (figure 2). In detail, we will derive concepts in safe care by selecting some concepts of SEM/YCFF for a metaphor/analogy and redefine the selected concepts in safe care to build a new set of concepts. A safe care concept model including individual characters, interpersonal relationships, hospitalisation environment and hospital culture may be constructed in this phase.
Figure 2.
Process of derivation strategy.
Stage 2 (A safe care theory model): A descriptive qualitative study will be performed to identify safe care systems’ content and logic relation based on the safe care concept model in the last phase. We hope to redefine the concept connotations and propose new statements according to the qualitative results. A safe care theory model, including the new concept definitions and statements, may be constructed in this phase (concept and statement derivation strategy).
Stage 3 (A safe care theory): The scales related to the safe care theory model will be used to test the concepts and statements. Based on the structural equation model/multivariate regression analysis results, we will revise the theory model, improve the theory diagram and develop the safe care theory (theory derivation strategy).
Concept, statement and theory derivation strategy
The complete theory exploration process generally includes defining concepts, finishing the statement of propositions and constructing a theory.22 Walker, famous nursing theorists, proposed three theoretical construction strategies: derivation, synthesis and analysis.10 The derivation strategy is the most widely used method among the three strategies. We choose the derivation strategy since it is well suited to situations where the theoretical framework still needs to be created or is outmoded.10 The five-step process of derivation strategy is as follows: (1) Review the literature to examine the level of theory construction in the _target field and summarise the connotations and application scopes of existing theories. (2) Read theories extensively and identify the theory that can be used to interpret the _target field. (3) Select a parent theory for conceptual, propositional and theoretical derivation. (4) Be immersed in the parent theory and extract content and structure that can be applied in the theory derivation. (5) Redefine or describe the new concept, statement and theory from the perspective of the parent theory with imagination and creativity.
Our study will select the SEM and the YCFF as the parent theory and follow the concept, statement and theory derivation process to develop a safe care theory. Mixed-method research includes collecting and analysing qualitative and quantitative data in a single study that investigates one phenomenon, which is conducive to producing a measure of safe experience and deeply exploring stakeholders’ perspectives about safe care.23 By conducting a mixed-methods study, we will generate clinical evidence to test the theoretical statements and improve the theoretical model. The overall study is divided into three parts, and the research methods of each part are as follows.
Stage 1: a safe care concept model
Study design
A scoping review will be performed using the methodological steps proposed by Arksey and O’Malley24 and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (online supplemental 1).25 The phases of scoping review are as follows: (1) identify the research question, (2) examine relevant studies, (3) select the study, (4) chart the data and (5) collate, summarise and report the results.
bmjopen-2023-072770supp001.pdf (78.2KB, pdf)
Data sources
Our research question is which factors are related to safe care for older inpatients and how these factors affect the safe care process. The preliminary article title is: Safe care for older inpatients from the perspective of socio-ecological model: A scoping review. The search strategy will focus on older adults, hospitalisation and patient safety. A series of MESH terms and free text terms will be applied to filtrate articles (online supplemental 2). Databases, including Web of Science, MEDLINE, Embase, CINAHL and Cochrane Center Register of Controlled Trials, will be searched, and no date or language restrictions will be set. Additional potential articles will be located by manually screening the reference lists of all involved articles. Publications that meet the following criteria will be included in the final analysis: (1) the cared group is older adults (aged 65 and above), (2) the place of care is the hospital and (3) patient safety incidents are related to hospital care. Non-human studies (eg, biological science research, molecular research), comments, letters to the editor and conference abstracts will be excluded.
bmjopen-2023-072770supp002.pdf (61KB, pdf)
Data extraction
Two reviewers will independently screen the title and abstract of identified publications in accordance with the above inclusion and exclusion criteria. Results will be pooled, and any discrepancies will be resolved through discussion with a third reviewer. In addition, we will report why full-text articles are excluded following the PRISMA-ScR framework. The same two reviewers will conduct data extraction, and the extracted information includes the year, authors, country, the key characteristics of participants (eg, age, disease type), study setting, clinical specialties, study aims, study design, main study findings and the factors relating to safe care in the hospital. Furthermore, we will chart the extracted data and identify the potential relationships of the concepts.
Data analysis
The SEM encompasses individual, interpersonal, environmental and policy levels,26 which will be regarded as a framework to summarise the concepts of safe care. The YCFF was initially designed to screen factors in patient safety incidents, and we will apply it to categorising facilitators and barriers to safe care. The above two frameworks may be integrated when necessary. Moreover, both inductive and deductive thematic analysis approaches will be used to examine and code the significant findings of each selected study. The thematic analysis method will provide a more holistic perspective to cover all the possible hypotheses in safe care.27 We will depict the scoping review results and outline the safe care concept model to lay a foundation for the subsequent mixed-methods study. Constructing the safe care concept model will start in October 2023 and end in March 2024.
Stage 2: a safe care theory model
Study design and participants
A qualitative study will be conducted, and the safe care concept model will be used as an organising framework to examine and analyse the interviewers’ viewpoints. A convenience sample of the older adults, their caregivers and the corresponding nurses in three clinics (department of general surgery, department of internal medicine and department of geriatrics) of West China Hospital, Sichuan University will be enrolled. This hospital is one of China’s most famous hospitals, with over 10 000 staff and more than 4300 beds.
The following inclusion criteria will be adopted to recruit participants. For the older: (1) being 65 years or older, (2) hospital stay is 3 days or more, (3) being able to understand the content of the investigation, (4) no obvious obstacles to communication and (5) voluntary participation. Older patients will be excluded if they are critically ill or their disease conditions are prone to change. For the caregivers: (1) being 18 years or older, (2) caring for older inpatients, and the length of care is greater than or equal to half of the patient’s hospital stay, (3) being able to understand the content of the investigation, (4) no obvious obstacles to communication and (5) voluntary participation. For the nurses: (1) registered nurses, (2) working in this department for 1 year or more and (3) voluntary participation.
Data collection
In qualitative studies, the sample size is expected to involve cases with rich information and reach a depth of understanding rather than striving to satisfy a certain number (statistically determined).28 Our study’s sample size is about 10–15 per group, and practical considerations will determine the actual number during the investigation. In addition, our sampling process will cover various ranges of participants and realise data saturation across contents and themes.
A semistructured interview outline guided by the safe care concept model will be used to explore deep descriptions of what factors are related to safe care and how these factors affect the safe care process (online supplemental 3). Prior to the interview, all participants will be fully informed of the study purposes and asked to sign the informed consent form. The participants’ sociodemographic information will be collected by a brief investigator-developed questionnaire, and patients’ clinical characteristics will be recorded from their dictations or medical records. Furthermore, the researcher will inform the participants that the interview process will be audio recorded and transcribed, and the research results will help construct a new care theory. The researchers will also inform participants that any information collected will be documented as blinded and confidential, and that all analysis results will be presented as aggregate to the researchers and in the case of public spread.
bmjopen-2023-072770supp003.pdf (70.4KB, pdf)
Data analysis
The trained researchers will perform interviews in Chinese. Then, the audiorecorded materials will be literally transcribed and anonymised, and a conceptual content analysis approach will be applied to analyse the qualitative data. This method is selected since it is appropriate when existing literature or theory in the area of interest is limited.
A coding outline will be built guided by the safe care concept model, and the transcripts will be coded by two researchers. First, two researchers will read all materials repeatedly to understand the whole. Second, they will read the materials at the theme level to derive codes by first highlighting the precise words/sentences from the document that appeared to capture core factors/concepts/thoughts and then making notes of their initial ideas and original analyses. After coding the transcripts, labels for codes will emerge that reflect more than one core theme (concept derivation strategy). These labels will be the key building blocks for the original theory model and will be sorted into clusters according to how various labels are linked (statement derivation strategy). Based on the literal and logical relationships between clusters, researchers will mix and organise these into a smaller number of higher-level categories with the guidance of a coding outline (theory derivation strategy). Next, a theory model containing the definitions for each category and statement will be created. Constructing the safe care theory model will start in April 2024 and end in April 2025.
Stage 3: a safe care theory
Study design and participants
A cross-sectional questionnaire study will be conducted at West China Hospital, Sichuan University. We will use a population-based convenience sampling method to investigate older inpatients in three clinics (department of general surgery, department of internal medicine and department of geriatrics). The inclusion criteria are as follows: (1) being 65 years or older, (2) hospital stay is 3 days or more, (3) being able to understand the content of the investigation, (4) no obvious obstacles to communication and (5) voluntary participation. Older patients will be excluded if they are critically ill or their disease conditions are prone to change.
Instrument
The questionnaire will contain three parts. Like the interview outline, the questionnaire is a preliminary draft, and items/scales might be added, deleted or revised later based on the safe care theory model. The first part of the questionnaire is a demographic table designed by the researchers, including (1) personal characteristics: age, gender, educational background, marital status, the number of children, smoking, drinking and monthly income; (2) personal medical factors: primary diseases, admitting diagnosis, medication history, medical insurance, length of hospital stay and (3) environment: safety incidents history, health status, social participation, and care satisfaction.
In the second part, we will use the Chinese version of the Hospital Consumer Assessment of Healthcare Providers and Systems scale (HCAHPS).29 HCAHPS was developed by the Agency for Healthcare Research and Quality and the Centers for Medicare & Medicaid Services.30 This scale has already become a widely used tool to measure the quality of hospital services by evaluating patients’ perceptions and satisfaction with hospital care. Chinese scholars translated HCAHPS into Chinese and conducted a cultural adaptation test. For the Chinese HCAHPS, the content validity indexing (CVI) score is 0.95, the comparative fit index of confirmatory factor analysis (CFA) is 0.93, and the standardised root mean square residual is 0.06.29 These test values show the scale is a reliable measuring instrument.
HCAHPS is composed of the following items: communication with physicians (three items), communication with nurses (three items), responsiveness of nurses (two items), education about new medications prescribed in the hospital (two items), pain management (two items), discharge planning (two items), and quietness and cleanliness of the hospital physical environment (two items).31 Patients will assess whether their perceptions are in line with the items and rate items from 1 (never) to 4 (always), except for the two items of discharge planning (no or yes). Moreover, patients will estimate the global hospital levels from 0 to 10 and express their thoughts on the hospital recommendation, rating from 1 (definitely not recommend) to 4 (definitely recommend). Our study will use this scale to reflect the patients' perception of ecological security (eg, caregivers, healthcare staff and hospital) and examine the interpersonal, environmental and policy dimensions of the safe care theory model.
In the third part, we will use the Safety Sense of Older Inpatients Scale (SSOIS) developed by Zhai.32 SSOIS includes four dimensions: healthcare behaviour (9 items), interpersonal relationship (7 items), ward management (6 items) and illness (5 items), with a total of 27 items. Patients estimate whether their feeling is congruent with the items and use a 5-point Likert scale to rate (1: strongly disagree; 2: disagree; 3: neutral; 4: agree and 5: strongly agree). The scores for each domain are added together to obtain a final score ranging from 27 to 135. A higher final score signifies a better sense of safety. SSOIS’ Cronbach alpha is 0.809, and the CVI is 0.836, which shows acceptable internal consistency reliability. Our study will use this scale to reflect inpatients’ safety perceptions.
Data collection
Data collection will be conducted by two trained researchers. They will visit West China Hospital, Sichuan University, and provide information about the research (eg, significance, study aims, risks and benefits of participation, and confidentiality) for eligible patients. Patients who choose to participate will be asked to sign an informed consent, complete the questionnaire and submit it to the researchers. Considering the special physical condition of older inpatients, researchers will help patients fill out the questionnaire based on patients’ answers when necessary. After the questionnaires are finished, researchers will check the answers’ completeness to ensure the questionnaires’ quality and then enter the questionnaires anonymously. We may use the multivariate regression analysis and/or structural equation model to analyse data. Therefore, the proportion of the sample size to the variables should be at least 20:1.33 Our study involves 17 variables, plus a 10% probability of sample loss, and the final sample size is at least 374.
Data analysis
The software SPSS Statistics V.24.0 will be used to analyse data. Descriptive statistics will be applied to calculate the participants’ demographics, and multivariate regression analysis will be used to identify the factors affecting safe care. In addition, based on the safe care theory model, we will use CFA to test the relationships between latent and observed variables. Then, we will use SPSS Amos V.24.0 software to explore models, use the maximum likelihood estimation method to assess the model parameters and optimise the model by the revised index. The level of significance will be set at 0.05. Data analysis methods might be revised according to research needs when necessary. Testing the safe care theory model and constructing the safe care theory will start in May 2025 and end in October 2025.
Data management
The mixed-method study has qualitative and quantitative data. After each investigation, researchers will check the completeness of data to ensure the data quality and then enter them into the database anonymously. Any unclear information will be promptly confirmed with the patient, and the data inspection and entry process will be carried out by two researchers simultaneously.
Research ethics
Participants will be recruited voluntarily and will receive information about confidentiality, anonymity, and the right to withdraw from the study at any time for any reason without consequence. All participants will be provided with consent forms before data collection, who choose to participate will be asked to sign an informed consent.
Patient and public involvement
This study has been designed and conducted in conjunction with the local patient and public involvement panel, which advised the use of literature review, qualitative research and quantitative research. The interview outline and questionnaires will be developed following the scoping review results. Patients, caregivers and nurses will be involved in this research’s design, implementation, reporting or dissemination plans.
Discussion
Based on the current hospital care situation, we follow the steps of the concept, statement and theory derivation strategy, combine core elements of the SEM and the YCFF, and design a mixed-methods study to construct and test the safe care theory model. Any concepts/factors that emerge as significant from qualitative and quantitative research will be screened and integrated into the final theory. The results of this project will offer a comprehensive perspective to analyse the mechanism affecting the safe care of older inpatients. The safe care theory for older inpatients will provide theoretical guidance for safe care services in clinical practice and play a crucial role in improving multiple stakeholders’ collaborative participation. Additionally, combining SEM and geriatric care enriches the theoretical connotation of safe care services and promotes effective hospital care management. The new combination pattern might be conducive to broadening the research horizon of the older care system and providing valuable references for future nursing theory research. We believe the findings will contribute to improving hospital care services for the ageing population.
Supplementary Material
Footnotes
Contributors: All listed authors certified their contribution. Conceptualisation: LY and XH; methodology: LY and XH; formal analysis and investigation: LY and LL; writing—original draft preparation: LY; writing—review and editing: XH, FW and LL. In addition, we thank all patients, caregivers and nurses who participated in the study.
Funding: This study was supported by the Sichuan Science and Technology Program (NO.2021YJ0016)
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. National Bureau of Statistics . China statistical Yearbook—2021. 2020. Available: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.html [Accessed 11 Aug 2022].
- 2. National Health Commission of the People’s Republic of China . 2022. Available: http://www.gov.cn/zhengce/zhengceku/2022-03/01/content_5676342.htm [Accessed 11 Aug 2022]. [DOI] [PMC free article] [PubMed]
- 3. Mikos M, Banas T, Czerw A, et al. Hospital inpatient falls across clinical departments. Int J Environ Res Public Health 2021;18:8167. 10.3390/ijerph18158167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Adamuz J, Juvé-Udina M-E, González-Samartino M, et al. Care complexity individual factors associated with adverse events and in-hospital mortality. PLoS One 2020;15:e0236370. 10.1371/journal.pone.0236370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sandoval T, Martínez M, Miranda F, et al. Incident adverse drug reactions and their effect on the length of hospital stay in older inpatients. Int J Clin Pharm 2021;43:839–46. 10.1007/s11096-020-01181-3 [DOI] [PubMed] [Google Scholar]
- 6. Heier L, Riouchi D, Hammerschmidt J, et al. Safety performance in acute medical care: a qualitative, explorative study on the perspectives of healthcare professionals. Healthcare 2021;9:1543. 10.3390/healthcare9111543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gunawan J, Aungsuroch Y, Watson J, et al. Nursing administration: watson’s theory of human caring. Nurs Sci Q 2022;35:235–43. 10.1177/08943184211070582 [DOI] [PubMed] [Google Scholar]
- 8. Silverglow A, Lidèn E, Berglund H, et al. What constitutes feeling safe at home? A qualitative interview study with frail older people receiving home care. Nurs Open 2021;8:191–9. 10.1002/nop2.618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huang H, Xiao L, Chen Z, et al. A national study of patient safety culture and patient safety goal in Chinese hospitals. J Patient Saf 2022;18:e1167–73. 10.1097/PTS.0000000000001045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lorraine O, Walker KCA. Strategies for Theory Construction in Nursing. 2018. Available: https://nursology.net/resources/books/strategies-for-theory-construction-in-nursing-6th-edition/ [accessed 11 Aug 2022]. [Google Scholar]
- 11. Collins AE. Health ecology and environmental management in Mozambique. Health Place 2002;8:263–72. 10.1016/s1353-8292(02)00005-9 [DOI] [PubMed] [Google Scholar]
- 12. Jang H-Y. Factors associated with successful aging among community-dwelling older adults based on ecological system model. Int J Environ Res Public Health 2020;17:3220. 10.3390/ijerph17093220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lak A, Rashidghalam P, Myint PK, et al. Correction to: comprehensive 5P framework for active aging using the ecological approach: an Iterative systematic review. BMC Public Health 2020;20:33. 10.1186/s12889-020-8227-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lawton R, McEachan RRC, Giles SJ, et al. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf 2012;21:369–80. 10.1136/bmjqs-2011-000443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Giles SJ, Lawton RJ, Din I, et al. Developing a patient measure of safety (PMOS). BMJ Qual Saf 2013;22:554–62. 10.1136/bmjqs-2012-000843 [DOI] [PubMed] [Google Scholar]
- 16. Litchfield I, Perryman K, Avery A, et al. From policy to patient: using a socio-ecological framework to explore the factors influencing safe practice in UK primary care. Social Science & Medicine 2021;277:113906. 10.1016/j.socscimed.2021.113906 [DOI] [PubMed] [Google Scholar]
- 17. Tan SHX, Lee CKJ, Yong CW, et al. Scoping review: Facilitators and barriers in the adoption of teledentistry among older adults. Gerodontology 2021;38:351–65. 10.1111/ger.12588 [DOI] [PubMed] [Google Scholar]
- 18. Akinyemiju T, Ogunsina K, Gupta A, et al. A socio-ecological framework for cancer prevention in low and middle-income countries. Front Public Health 2022;10:884678. 10.3389/fpubh.2022.884678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bamuya C, Correia JC, Brady EM, et al. Use of the socio-ecological model to explore factors that influence the implementation of a diabetes structured education programme (EXTEND project) inLilongwe, Malawi and Maputo, Mozambique: a qualitative study. BMC Public Health 2021;21:1355. 10.1186/s12889-021-11338-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Albalawi A, Kidd L, Cowey E. Factors contributing to the patient safety culture in Saudi Arabia: a systematic review. BMJ Open 2020;10:e037875. 10.1136/bmjopen-2020-037875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Albutt A, Berzins K, Louch G, et al. Health professionals’ perspectives of safety issues in mental health services: a qualitative study. Int J Ment Health Nurs 2021;30:798–810. 10.1111/inm.12838 [DOI] [PubMed] [Google Scholar]
- 22. Lau SC, Bhattacharjya S, Fong MW, et al. Effectiveness of theory-based digital self-management interventions for improving depression, anxiety, fatigue and self-efficacy in people with neurological disorders: a systematic review and meta-analysis. J Telemed Telecare 2022;28:547–58. 10.1177/1357633X20955122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Philippa R, Ann H, Jacqueline M, et al. Professional identity in nursing: a mixed method research study. Nurse Educ Pract 2021;52:103039. 10.1016/j.nepr.2021.103039 [DOI] [PubMed] [Google Scholar]
- 24. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 25. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-SCR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 26. Katewongsa P, Pongpradit K, Widyastari DA. Physical activity level of Thai children and youth: evidence from Thailand’s 2018 report card on physical activity for children and youth. J Exerc Sci Fit 2021;19:71–4. 10.1016/j.jesf.2020.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Obieche O, Lee M, Salehi N. Exploring attitudes towards smoking behaviour and cessation among hospitalised smokers via a socio-ecological framework: a scoping review. Addict Behav 2021;122:107040. 10.1016/j.addbeh.2021.107040 [DOI] [PubMed] [Google Scholar]
- 28. Whop LJ, Butler TL, Brotherton JML, et al. Study protocol: yarning about HPV vaccination: a qualitative study of factors influencing HPV vaccination among aboriginal and Torres Strait Islander adolescents in Australia. BMJ Open 2021;11:e047890. 10.1136/bmjopen-2020-047890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu K, Squires A, You L-M. A pilot study of a systematic method for translating patient satisfaction questionnaires. J Adv Nurs 2011;67:1012–21. 10.1111/j.1365-2648.2010.05569.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Giordano LA, Elliott MN, Goldstein E, et al. Development, implementation, and public reporting of the HCAHPS survey. Med Care Res Rev 2010;67:27–37. 10.1177/1077558709341065 [DOI] [PubMed] [Google Scholar]
- 31. Liu X, Zheng J, Liu K, et al. Associations of nurse education level and nurse staffing with patient experiences of hospital care: a cross sectional study in China. Res Nurs Health 2020;43:103–13. 10.1002/nur.22003 [DOI] [PubMed] [Google Scholar]
- 32. Zhai X. Analysis of the influencing factors of sense of security in hospitalized older patients, Available: https://kns.cnki.net/kcms/detail/detail.aspxdbcodeCMFDdbnameCMFD201501filename1014332344.nhuniplatformNZKPTv1cHZYwjKWmJoIEOApScMD3tmm-Upcz9nK0o6HUhjYKMcM7mQ2LCrym8GKniyESL [Accessed 1 Aug 2022].
- 33. Yao L, Xiao M, Luo Y, et al. Research on the factors that influence patients with colorectal cancer participating in the prevention and control of surgical site infection: based on the extended theory of planned behaviour. Health Expect 2021;24:2087–97. 10.1111/hex.13355 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072770supp001.pdf (78.2KB, pdf)
bmjopen-2023-072770supp002.pdf (61KB, pdf)
bmjopen-2023-072770supp003.pdf (70.4KB, pdf)