Abstract
Introduction
Cardiometabolic disease (CMD) is the leading cause of mortality in China. A healthy diet plays an essential role in the occurrence and development of CMD. Although the Chinese heart-healthy diet is the first diet with cardiovascular benefits, a healthy dietary pattern that fits Chinese food culture that can effectively reduce the risk of CMD has not been found.
Methods/design
The study is a single-centre, open-label, randomised controlled trial aimed at evaluating the effect of the Reducing Cardiometabolic Diseases Risk (RCMDR) dietary pattern in reducing the risk of CMDs in people with dyslipidaemia and providing a reference basis for constructing a dietary pattern suitable for the prevention of CMDs in the Chinese population. Participants are men and women aged 35–45 years with dyslipidaemia in Tianjin. The _target sample size is 100. After the run-in period, the participants will be randomised to the RCMDR dietary pattern intervention group or the general health education control group with a 1:1 ratio. The intervention phases will last 12 weeks, with a dietary intervention of 5 working days per week for participants in the intervention group. The primary outcome variable is the cardiometabolic risk score. The secondary outcome variables are blood lipid, blood pressure, blood glucose, body composition indices, insulin resistance and 10-year risk of cardiovascular diseases.
Ethics and dissemination
The study complies with the Measures for Ethical Review of Life Sciences and Medical Research Involving Human Beings and the Declaration of Helsinki. Signed informed consent will be obtained from all participants. The study has been approved by the Medical Ethics Committee of the Second Hospital of Tianjin Medical University (approval number: KY2023020). The results from the study will be disseminated through publications in a peer-reviewed journal.
Trial registration number
Chinese Clinical Trial Registry (ChiCTR2300072472).
Keywords: Randomized Controlled Trial, Cardiovascular Disease, NUTRITION & DIETETICS, DIABETES & ENDOCRINOLOGY
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The Reducing Cardiometabolic Diseases Risk dietary pattern is designed based on the dietary habits of Chinese people, and following it can help reduce the risk of cardiometabolic diseases.
The pattern considers dietary feeding and guidance, which can help participants learn and maintain healthy eating habits even after the study ends.
The blinding of data analysis and indicator detection techniques used during the study helped minimise any bias that could have affected the results of the open trial.
Introduction
Cardiometabolic disease (CMD) is a kind of syndrome with cardiovascular damage and abnormal metabolism, including a series of diseases, such as cardiovascular disease (CVD), diabetes, dyslipidaemia and metabolic syndrome,1 which is the leading cause of mortality in China2 and worldwide.3 Dyslipidaemia is not only a type of CMD, but also a significant risk factor for other CMDs. In China, the prevalence of dyslipidaemia in adults has reached 35%, and has remained at a high level in recent years.4 Several studies have found a potential association between lipid metabolism and the risk of CMDs.5–7 It was plausible that dietary interventions might affect the risk of CMDs by regulating some lipid molecules.8 9
Diet is one of the ordinary and modifiable factors of CMDs. According to the Global Burden of Diseases Study 2017, nearly one-fifth of total death globally was attributed to diseases such as CVDs, metabolic diseases and cancers caused by unhealthy diet.10 In 2019, China ranked first globally in terms of the absolute number of diet-related CVD death and disability-adjusted life-year burden.11 In the past few decades, the dietary structure of the Chinese has undergone notable changes. In China, from 1982 to 2012, consumption of cereals, tubers and vegetables decreased; consumption of fruits, milk, eggs and nuts remained low; animal food consumption, primarily pork, increased rapidly, from 52.6 g/day to 137.7 g/day; cooking oil and salt consumption remained high; and the percentage of energy from fat increased from 18.4% to 32.9%.12 High sodium, low fruit and low marine n-3 fatty acids were leading dietary risk factors for CMD mortality in China.13 Therefore, in the prevention and treatment of CMD, it is of great value to study the association between dietary factors and CMD, and to develop dietary patterns appropriate for the Chinese.
Dietary pattern analysis is essential for exploring the relationship between the intake of various food groups or multiple nutrients and health outcomes from a holistic perspective, which is closer to daily diets.14 15 Some Hesperian healthy dietary patterns have been demonstrated to be cardiometabolic protective, such as the Dietary Approaches to Stop Hypertension (DASH) and the Mediterranean diet.16–18 However, because Chinese food culture differs from Hesperian food culture, healthy dietary patterns cannot simply be copied. The Chinese heart-healthy (CHH) diet is the first diet with a cardiovascular protective effect that fits Chinese food culture, but its effect on metabolic diseases is unclear.19 To date, a healthy dietary pattern has not been found that can comprehensively prevent CMDs in line with the dietary characteristics of the Chinese.
Consequently, a dietary pattern that might improve CMD health based on Chinese food culture was developed—the Reducing Cardiometabolic Diseases Risk (RCMDR) dietary pattern. This single-centre, randomised, open-label, parallel-controlled dietary intervention study was designed to assess the effect of the RCMDR dietary pattern on reducing CMD risk in people with dyslipidaemia. Moreover, the secondary aim of this study is to assess the effect of the RCMDR dietary pattern on improving blood lipids, blood pressure, blood glucose, insulin resistance, body composition indices and 10-year CVD risk.
Methods
Study design
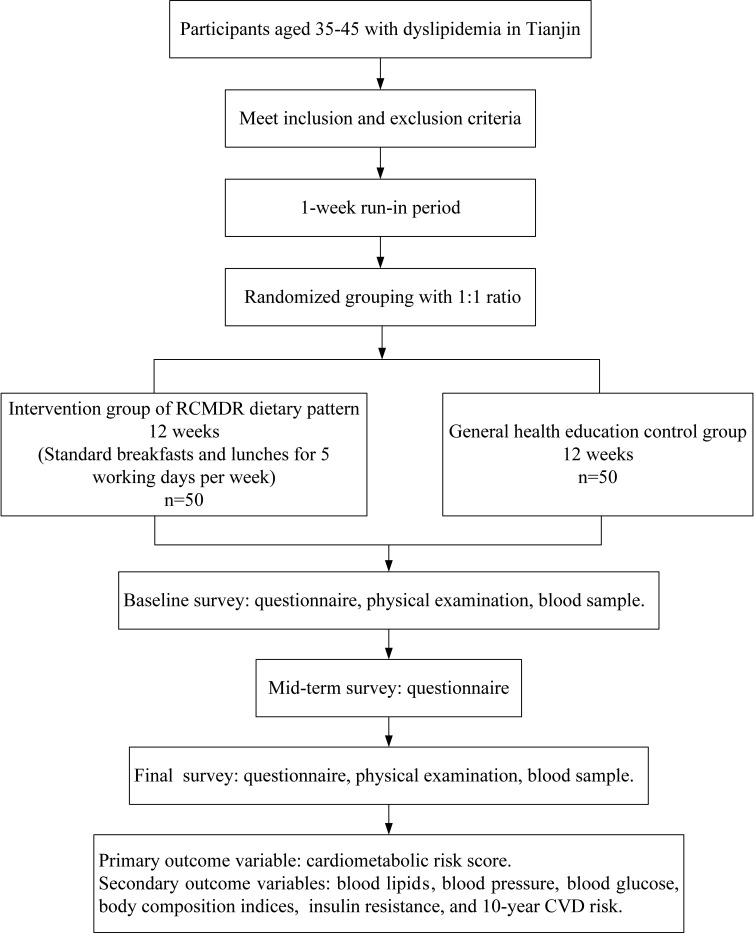
A single-centre, open-label, randomised controlled dietary intervention study was designed. In Tianjin, 100 eligible participants aged 35–45 years with dyslipidaemia will be recruited. Enhanced management of dyslipidaemia in this age group may better reduce the risk of incident CVD and diabetes and contribute to the primary prevention of CMDs.20–22 Participants will be randomised and allocated into the RCMDR dietary pattern intervention group or the general health education control group, with 50 participants in each group. After a 1-week run-in period, participants in the intervention group will receive free standard breakfasts and lunches and dietary guidance based on the RCMDR dietary pattern. Standard breakfasts and lunches will be prepared and cooked by cooks based on menus and recipes developed by a nutritionist, using the ingredients available in local markets. According to the 2023 Chinese guideline for lipid management, the lipid level should be reviewed in the first 3–6 months for those receiving non-pharmacological treatment such as diet control.4 Consistent with previous studies,23 24 the interventions will last 12 weeks. During intervention phases, standard breakfasts and lunches will be provided 5 working days per week, and dietary advice will be provided 2 rest days per week. Participants in the control group will receive dietary guidance based on the ‘Dietary Guidelines for Chinese Residents (2022)’ for 12 weeks. The schedule of follow-up, physical examinations and indices measurements will be the same for both groups. Figure 1 shows the flow chart of the study.
Figure 1.
The flow chart of the study. CVD, cardiovascular disease; RCMDR, Reducing Cardiometabolic Diseases Risk.
Participant recruitment
Participants will be recruited by researchers using posters. After an initial understanding of the study, potential participants will enrol voluntarily. Men and women aged 35–45 years with dyslipidaemia are eligible for the study according to the results of their latest physical examination. Subsequently, participants will be randomised into intervention and control groups. The details of inclusion and exclusion criteria are listed.
Inclusion criteria
Aged 35–45 years, permanent residents in Tianjin.
-
With borderline elevation of blood lipids and low or moderate risk of atherosclerotic CVD (ASCVD), meeting one of the following conditions:
5.2 mmol/L≤total cholesterol (TC)<7.2 mmol/L.
3.4 mmol/L≤low-density lipoprotein cholesterol (LDL-C)<4.9 mmol/L.
1.7 mmol/L≤triglyceride (TG)<2.3 mmol/L.
High-density lipoprotein cholesterol (HDL-C) <1.0 mmol/L.
Without lipid-lowering therapy (the above dyslipidaemic population).
Agree to participate in the study and sign an informed consent form.
Exclusion criteria
-
With high-risk or extremely high-risk ASCVD,4 meeting one of the following conditions:
Patients with ASCVD.
Patients with diabetes ≥40 years old.
Chronic kidney disease stages 3–4.
Patients with grade 2 or above hypertension, or those with grade 1 hypertension who have two or more risk factors (risk factors include smoking, HDL-C <1.0 mmol/L, men aged ≥45 years old).
With a tumour or mental health diseases (such as depression, mania, anxiety, schizophrenia).
With abnormal thyroid, liver or kidney function.
With cardiovascular or cerebrovascular diseases.
With active epilepsy or severe auditory perception disorders, which make it difficult for participants to cooperate with the investigation.
The researchers consider the person unfit to complete the study.
Run-in period and randomisation
After signing informed consent forms, participants will enter a 1-week run-in period. The purpose of setting a run-in period is to help participants familiarise themselves with the intervention scheme and to allow the researchers to ascertain participants’ intake of daily food and estimated energy requirement (EER), as well as to identify and exclude participants who are failing to adhere to the study protocol. During the run-in, participants in both groups will be requested to keep dietary records of the variety and intake of all foods consumed during the day. At the end of the run-in period, participants will be reassessed for eligibility and adherence to the study protocol. Any participant who fails to complete dietary records for 2 or more days a week for any reason will be excluded from further participation in the study.
Participants will be formally enrolled in the study if they pass the run-in period and complete the baseline data collection. Participants will be randomised into intervention and control groups with a 1:1 ratio by a statistical analyst unaware of the study, using a random sequence generated by SPSS V.24.0. The randomised allocation concealment will be ensured using opaque sealed envelopes. The researchers responsible for recruitment would not know the allocation sequence in advance.
Blinding
In the study, we will only provide the feeding intervention to participants in the intervention group, so it is not possible to implement blinding to the participants. Meanwhile, it is also infeasible to blind the cooks, nutritionists and researchers in charge of preparing and measuring the standard meals. In addition, the researchers responsible for outcome assessment and data analysis will be blinded to the group allocation, and the data will be input into the computer by people outside the research team. On the other side, it might be easier to recruit participants in an open-label study than in a blinded study.
Intervention
Depending on the EER of the participants in the intervention group, the standard meals will be divided into three energy classes: 1400–1700 kcal, 1700–2000 kcal and over 2000 kcal. Standard breakfasts and lunches will be prepared in the kitchen, then delivered to the fixed canteen and distributed to each participant in the intervention group. Participants will be required to take photos of the leftovers from each standard meal and record the intake of all food consumed on weekdays (excluding standard meals) and rest days. Researchers will calculate the intake of daily nutrients based on these data and provide personalised dietary guidance to the participants. The frequency of dietary guidance will be once a week in the first month, once every 2 weeks in the second month and once in the third month.
The participants in the control group will not be provided with standard meals, but will only receive dietary guidance based on the ‘Dietary Guidelines for Chinese Residents (2022)’. Participants in the control group will be required to choose any 1 working day and rest day every week for dietary records. The frequency of dietary guidance will be the same as the intervention group.
Recipes of standard meals will be developed by researchers, nutritionists and cooks based on the nutritional composition of the RCMDR dietary pattern. The nutrient composition of the RCMDR dietary pattern and the methods to reach it are shown in table 1. Compared with other dietary patterns with cardiometabolic benefits, such as the DASH diet and the Mediterranean diet,25 26 the nutrient composition of the RCMDR dietary pattern was more similar to that of the CHH diet, including energy proportions of macronutrients and the amount of sodium, potassium and fibre. Besides, considering the participants have dyslipidaemia, we added a restriction on the intake of cholesterol.
Table 1.
The nutrient composition of the RCMDR dietary pattern and methods to reach the goals of nutrients
| Nutrients | Intake | Methods to reach the goals |
| Energy (kcal) | 1450–2350 | Average intake was evaluated during the run-in period. |
| Energy distribution of three meals | ||
| Breakfast:lunch:dinner | 3:4:3 | |
| Energy distribution of macronutrients | ||
| Carbohydrates (kcal%) | 56–58% | Increasing the use of whole grains and limiting added sugars (monosaccharide, disaccharide). |
| Protein (kcal%) | 17–19% | Increasing protein intake in legumes, dairy products, fish and lean meat. |
| Fat (kcal%) | 24–26% | Reducing the use of cooking oil by changing cooking methods, such as using steam instead of frying and using low-fat or skim dairy products, choosing skinned lean meat. |
| Saturated | <7% | Banning animal cooking oils. |
| Monounsaturated | 12% | Increasing the use of vegetable oil rich in monounsaturated fatty acid. |
| Polyunsaturated | 6–8% | Increasing the use of nuts and n-3 polyunsaturated fatty acid-rich fish. |
| Cholesterol (mg/day) | <300 | Reducing the use of animal-based foods. |
| Fibre (g/day) | 30 | Increasing the use of foods high in dietary fibre, such as whole grains, legumes, vegetables and fruits. |
| Sodium (mg/day) | 3000 | Reducing the use of salt and sodium seasoning during cooking. |
| Potassium (mg/day) | 3700 | Increasing the use of food with high potassium content. |
| Magnesium (mg/day) | 500 | Increasing the use of food with high magnesium content. |
| Calcium (mg/day) | 1000 | Increasing the use of dairy products, soy products, fish, nuts and dark vegetables. |
| Folate (μg/day) | 400–800 | Increasing the use of plant-based foods that contain high amounts of folate. |
RCMDR, Reducing Cardiometabolic Diseases Risk.
The RCMDR dietary pattern was preliminarily developed based on previous studies’ evidence, including food types, intake ranges and explanations. Then, the Delphi method was used to optimise and modify the dietary pattern. In the end, a total of 23 experts completed two rounds of consultation, and the results showed that the active coefficients of the two rounds of expert consultation were 92.00% and 100%; the expert authority indices of the two rounds of expert consultation were 0.751 and 0757; and the Kendall’s W coefficients of the two rounds of expert consultation were 0.302 and 0.504; thus, a consensus was obtained (online supplemental file 1). The final RCMDR dietary pattern was established, including 9 domains, 20 subdomains and 5 elements. The detailed content of the RCMDR dietary pattern is shown in table 2.
Table 2.
The RCMDR dietary pattern
| Food groups | Edible portion intake | Explanation |
| Cereals and tubers | ||
| Cereals | 200–300 g/day | |
| Whole grains | 90–150 g/day | |
| Legumes* | 10–30 g/day | |
| Tubers | 50–100 g/day | |
| Vegetables and fruits | ||
| Vegetables | 350–550 g/day | |
| Dark green leafy and cruciferous species vegetables | 200–250 g/day | |
| Other dark vegetables | 100–200 g/day | |
| Other vegetables | 50–100 g/day | |
| Fruits | 200–350 g/day | Complete fresh fruits |
| Foods of animal origin | 90–150 g/day | Banning processed meat products |
| Fish | 300–500 g/week | Eating 3–4 times a week and choosing fish rich in n-3 PUFAs |
| Poultry | 100–175 g/week | Skinned lean meat, fresh meat |
| Livestock meat | 100–125 g/week | Skinned lean meat, fresh meat |
| Eggs | 3–5 per week | |
| Dairy products | 300–500 g/day | Low-fat or skimmed milk, yoghurt or other fermented dairy products |
| Soybeans and nuts | ||
| Soybeans | 30–40 g/day | The intake of soy products is calculated based on the same protein content. Individuals with hyperuricaemia or gout are not recommended to increase their intake of soybeans or soy products. |
| Nuts | 10–20 g/day | |
| Oil and salt | ||
| Cooking oil | 15–25 g/day | Alternating consumption of various vegetable oils rich in unsaturated fatty acid and avoiding animal oils |
| Salt | <5 g/day | Low-sodium salt is recommended for those without contraindications. |
| Added sugar | ||
|
Added sugar (monosaccharide,disaccharide) |
<150 g/week | Limiting the consumption of non-sugar sweeteners (NSS): all non-nutritional sweeteners that do not belong to the sugar category are low-calorie or calorie-free substitutes for free sugars. Common NSS include acesulfame, aspartame, edvante, cyclamate, neotame, saccharin, sucralose, steviol glycosides and steviol derivatives. |
| Sugar-sweetened beverages | Eliminating or limiting the consumption of sugar-sweetened beverages | Drinking sugary beverages should be calculated in the weekly intake of added sugar. |
|
Other sugary foods (cakes, cookies, cold drinks and snacks, candy, etc) |
Eliminating or limiting the consumption of other sugary foods | Eating other sugary foods should be calculated in the weekly intake of added sugar. |
| Water and alcohol | ||
| Water or tea | 1700 mL/day for males, 1500 mL/day for females | Summer or excessive sweating can be increased as needed. |
| Alcohol | <15 g/day | Eliminating or limiting the consumption of alcohol |
*Legumes do not include soybeans.
PUFAs, polyunsaturated fatty acids; RCMDR, Reducing Cardiometabolic Diseases Risk.
bmjopen-2023-082957supp001.pdf (4.5MB, pdf)
Compared with the CHH diet and ‘Dietary Guidelines for Chinese Residents (2022)’, the RCMDR dietary pattern has some characteristics concerning the intake of food groups. First, the intake of whole grains, vegetables, soy and its products, and nuts increased. Because of the cardiometabolic protective effects of these foods,27–30 we increased the intake of whole grains to 90–150 g/day, approximately accounting for one-half of cereals; increased the intake of vegetables to 350–550 g/day; increased the intake of soybeans to 30–40 g/day; and increased the intake of nuts to 10–20 g/day. Second, we reduced the intake of animal-based foods and divided meat intake into fish, poultry and livestock. In particular, the intake of red meat was reduced to 100–125 g/week and processed meat was banned. Meanwhile, considering the high content of lipids such as cholesterol, TGs and phospholipids in egg yolk,31 the intake of eggs was adjusted to three to five per week. However, the frequency of fish consumption was increased to three to four times per week, emphasising the importance of consuming fish rich in n-3 polyunsaturated fatty acids (PUFAs). Third, the RCMDR dietary pattern emphasised alternating consumption of various vegetable oils rich in unsaturated fatty acids and avoiding animal oils. In order to achieve this _target, our standard breakfast and lunch will be cooked with olive oil, and participants will be encouraged to use vegetable oils rich in n-3 PUFAs for low-temperature cooking at home, such as flaxseed oil.32
Specifically, the RCMDR dietary pattern includes a set of recipes of 2-week non-repeating and interchangeable standard breakfasts and lunches, as well as suggestions for dinners. These recipes were developed based on the nutrient composition and the food group intake of the RCMDR dietary pattern. Considering the generalisability and affordability of the RCMDR dietary pattern, the daily cost was approximately 50–60 renminbi per person per day, using common local food ingredients and cooking methods. In addition, the study will adopt a combination of feeding intervention and dietary guidance, making it easier for the participants and their families to learn and master the dietary pattern according to these recipes. Even after the experiment, the RCMDR dietary pattern is easy to grasp and stick to. A sample 1-day recipe is shown in table 3.
Table 3.
An example of a 1-day recipe for a diet
| RCMDR dietary pattern | |
| Breakfast | Sweet potato-filled whole wheat steamed bun |
| Millet congee | |
| Boiled spinach with olive oil | |
| Boiled egg | |
| Cherry tomatoes | |
| Walnuts and hazelnuts | |
| Skim milk | |
| Lunch | Steamed rice with quinoa and chickpeas |
| Stir-fried purple cabbage with coloured pepper | |
| Stir-fried water spinach | |
| Stewed tofu with tomato | |
| Steamed fish | |
| Snack | Sugar-free yoghurt |
| Apple | |
| Dinner (suggestions) |
Whole-grain cereal product |
| Boiled or stir-fried vegetables | |
| Boiled or stir-fried soy products |
RCMDR, Reducing Cardiometabolic Diseases Risk.
Measurements and data collection
Formal baseline data collection will be conducted on the last 2 days of the run-in period, including a questionnaire interview on demography (age, gender, education, marital status), lifestyle (smoking, drinking, physical activity and sleep status), dietary habit (frequency questionnaire and 24-hour food record), history of diseases (hypertension and diabetes), family history of disease (hypertension, diabetes, hyperlipidaemia, coronary heart disease, stroke and cancer), medication use (antihypertensive drugs and antidiabetic drugs), dietary supplement use (fish oil, vitamin C, vitamin B, calcium tablets, folic acid, multivitamins, iron, others), physical examinations (height, weight, blood pressure, waist–hip ratio, body composition indices), fasting blood test (fasting blood glucose (FBG), fasting insulin (FINS), glycated haemoglobin (HbA1c), fasting C peptide, TC, TGs, LDL-C, HDL-C, folic acid, homocysteine (Hcy), liver function (alanine aminotransferase (ALT), aspartate transaminase (AST)), kidney function (serum uric acid, urea, creatinine), apolipoprotein E (ApoE) and methylenetetrahydrofolate reductase (MTHFR) genotype polymorphism.
Methods of physical measurements
Blood pressure measurement: the Omron J710 upper arm electronic blood pressure monitor measures systolic blood pressure (SBP) and diastolic blood pressure (DBP). The third measurement will be required if the difference between SBP and DBP exceeds 10 mm Hg.
Body composition indices measurement: the body composition analyser and bioelectrical impedance method were used to measure body composition indices, such as height, weight, waist-to-hip ratio, body fat mass, body muscle mass and visceral fat mass, subcutaneous fat mass, basal energy expenditure, EER, etc.
Blood sample collection and tests
Blood samples will be collected at baseline and the end of the study. Before collecting blood samples, participants will be required to fast for at least 10 hours overnight. Fasting venous blood from participants will be collected by qualified nurses. The blood samples will be refrigerated and transported to the central laboratory of the School of Public Health, Tianjin Medical University. Analysis of FBG (using the glucose oxidase method), HbA1c (using the immunosuppressive turbidimetry), TG and TC (using the enzyme endpoint method), HDL-C and LDL-C (using the polyethylene sulfate precipitation method), and ALT, AST, serum uric acid, urea and creatinine (using the enzymatic method) will be carried out on a Roche Cobas 8000 automatic biochemistry analyser. Fasting C peptide and FINS were measured using ELISA kit. Serum folic acid was measured using a chemiluminescence immunoassay analyser. Serum Hcy (using the enzyme cycling method) was measured using an automated chemical analyser. ApoE and MTHFR genotype polymorphism testing will be commissioned by a gene sequencing company.
Dietary intake of foods and nutrients
First, all raw materials will be weighed before cooking, including the amount of oil and salt used. After cooking, each dish will be weighed according to the energy level of the standard meal. Researchers will calculate the average daily energy and dietary nutrients each participant takes using the China Food Composition (sixth edition) based on the photos of leftovers and dietary records submitted by the participants.33
Follow-up schedules
At the mid-term of the study, the uninformed researchers will carry out the same questionnaire interview. At the end of the study, the uninformed researchers will conduct the same questionnaire interview and physical examination of the participants using the same method as the baseline. The frequency of dietary guidance for participants in both groups will be the same: once a week in the first month, once every 2 weeks in the second month and once in the third month. Dietary data of participants in the intervention group will be collected daily, and in the control group will be collected twice a week. The schedule of measurements and visits of the study has been summarised in table 4.
Table 4.
The schedule of measurements and visits of the study
| Follow-up (weeks) | ||||||||||
| Screening | Run-in* | 1 | 2 | 3 | 4 | 6 | 8 | 10 | 12 | |
| Signed informed consent | √ | |||||||||
| Eligibility confirmation | √ | √ | ||||||||
| Questionnaire interview | √ | √ | √ | √ | ||||||
| Dietary record† | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
| Dietary guidance | √ | √ | √ | √ | √ | √ | √ | √ | ||
| Physical examination | √ | √ | ||||||||
| Fasting blood test | √ | √ | ||||||||
| Blood sample | √ | √ | ||||||||
| Reasons for withdrawal | √ | √ | √ | √ | √ | √ | √ | √ | √ | |
*Baseline data are collected on the last 2 days of the run-in period.
†Dietary data of participants in the intervention group will be collected daily.
Outcomes
The primary outcome is the change in cardiometabolic risk (CM-risk) score from baseline to the end of the study. The secondary outcomes include a change in blood lipid (LDL-C, TC, TG, HDL-C), blood pressure, FBG, insulin resistance measured by Homeostasis Model Assessment, body composition indices and 10-year risk of CVD from the Prediction for Atherosclerotic Cardiovascular Disease Risk in China.34
Sample size
Although the CM-risk score is the primary outcome, the methods of calculating the cardiometabolic score in different studies are inconsistent. Participants in the study have dyslipidaemia, and according to the 2023 Chinese guideline for lipid management, LDL-C is the primary _target for lipid intervention.4 Therefore, the sample size in the study was calculated using the change of LDL-C from baseline to the end of the study. According to the previous study that the calorie-restricted Mediterranean-style diet successfully reduced LDL-C by 0.23 mmol/L for patients with hypercholesterolaemia in 4 weeks, we conservatively assumed that the RCMDR dietary pattern will reduce LDL-C by 0.3 mmol/L in 12 weeks, and the SD of LDL-C change is 0.5 mmol/L in the control group.35 To have 80% power with a type I error rate of 5% to detect the assumed effect size, we would need 44 participants in each group. Assuming that 10% of study participants will be lost by the end of the study, 100 participants will be recruited.
Data management
Data will be collected in an electronic database. Participants will only be identified by a unique ID. Hard copies of data sheets containing participants’ files and other data (including questionnaires, test results, records of informed consent and other documents related to the conduct of the study) will be kept securely in a locked filing cabinet in a locked office, accessible only to key research team members. Blood samples will be kept in a locked freezer. All data and blood samples will be stored in Tianjin Medical University.
Statistical analysis
Statistical analyses will be performed using SPSS V.24.0 software. The analyses of outcomes will follow the intention-to-treat principle. Continuous variables conforming to normal distribution will be expressed as mean±SD, and non-normally distributed continuous variables will be expressed as median with limits of the IQR (25th and 75th percentiles). Categorical variables will be shown as frequencies and proportions (percentages). The differences in baseline variables between groups will be evaluated by using a t-test, Wilcoxon rank test or χ2 test. Linear regression will be used to estimate the absolute differences between the two groups regarding primary and secondary outcomes and reported as the least squares mean after adjusting the centre. Sensitivity analyses will be conducted to repeat the primary analyses with imputed missing values. We will use multiple imputations to impute missing values of outcomes. A two-sided p value of <0.05 will be considered statistically significant.
Quality control
The reliability and validity of the questionnaire are high. According to the purpose of this study, based on previous studies, multiple collective discussions were conducted to unify the evaluation standards of the questionnaire, ensuring scientificity, consistency and comparability. All researchers participating in this study must receive uniform training and be tested after training, including standard operating procedures for participant data collection and methods for collecting and preserving biological samples to ensure accurate and complete information and to avoid measurement bias. All biological samples will be tested in the central laboratory of Tianjin Medical University. The researchers responsible for detecting relevant indicators will be blinded to the randomisation grouping of participants.
Patient and public involvement
This research study did not involve patients or the general public in its design, conduct, reporting or dissemination.
Ethics and dissemination
The study complies with the Measures for Ethical Review of Life Sciences and Medical Research Involving Human Beings and the Declaration of Helsinki. Signed informed consent will be obtained from all participants (online supplemental file 2). The study has been approved by the Medical Ethics Committee of the Second Hospital of Tianjin Medical University (approval number: KY2023020) and registered in the Chinese Clinical Trial Registry (ChiCTR2300072472). The results from the study will be disseminated through publications in a peer-reviewed journal.
bmjopen-2023-082957supp002.pdf (4.1MB, pdf)
Current status
The first participant was enrolled on 14 June 2023.
In summary, the study is a randomised controlled dietary intervention trial to evaluate the effect of the RCMDR dietary pattern on cardiometabolic health in people with dyslipidaemia. The study not only comprehensively considered the effect of diet on CMDs, but also considered the generalisability and affordability of the RCMDR dietary pattern among the population. The study’s findings will significantly prevent CMDs in China and improve Chinese residents’ nutritional status and health levels.
Supplementary Material
Footnotes
Contributors: GH, WL and FM conceived and designed the study. QW, LZ, CC, XC, LH and TL will perform the study, collect and analyse all experimental data. QW provided the first version of the manuscript. SB, ZL, HL, JY, YD, YC, MZ, LC, WL, FM and GH provided critical comments on the original manuscript. WL and GH revised and finalised the manuscript. All authors read and approved the final version of the manuscript.
Funding: This research was supported by the National Nutrition Science Research Grant of Chinese Nutrition Society (grant number: CNS-NNSRG2022-149).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Castro JP, El-Atat FA, McFarlane SI, et al. Cardiometabolic syndrome: pathophysiology and treatment. Curr Hypertens Rep 2003;5:393–401. 10.1007/s11906-003-0085-y [DOI] [PubMed] [Google Scholar]
- 2. The WCOTROCHADIC . Report on cardiovascular health and diseases in China 2022: an updated summary. Biomed Environ Sci 2023;36:669–701. 10.3967/bes2023.106 [DOI] [PubMed] [Google Scholar]
- 3. Ralston J, Nugent R. Toward a broader response to cardiometabolic disease. Nat Med 2019;25:1644–6. 10.1038/s41591-019-0642-9 [DOI] [PubMed] [Google Scholar]
- 4. Li J-J, Zhao S-P, Zhao D, et al. Chinese guideline for lipid management. Front Pharmacol 2023;14:1190934. 10.3389/fphar.2023.1190934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kaze AD, Santhanam P, Musani SK, et al. Metabolic dyslipidemia and cardiovascular outcomes in type 2 diabetes mellitus: findings from the look ahead study. J Am Heart Assoc 2021;10:e016947. 10.1161/JAHA.120.016947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Niu Z, Wu Q, Sun L, et al. Circulating glycerolipids, fatty liver index, and incidence of type 2 diabetes: a prospective study among Chinese. J Clin Endocrinol Metab 2021;106:2010–20. 10.1210/clinem/dgab165 [DOI] [PubMed] [Google Scholar]
- 7. Chen S, Wu Q, Zhu L, et al. Plasma glycerophospholipid profile, erythrocyte N–3 pufas, and metabolic syndrome incidence: a prospective study in Chinese men and women. Am J Clin Nutr 2021;114:143–53. 10.1093/ajcn/nqab050 [DOI] [PubMed] [Google Scholar]
- 8. Eichelmann F, Sellem L, Wittenbecher C, et al. Deep lipidomics in human plasma: cardiometabolic disease risk and effect of dietary fat modulation. Circulation 2022;146:21–35. 10.1161/CIRCULATIONAHA.121.056805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen S, Zong G, Wu Q, et al. Associations of plasma glycerophospholipid profile with modifiable lifestyles and incident diabetes in middle-aged and older Chinese. Diabetologia 2022;65:315–28. 10.1007/s00125-021-05611-3 [DOI] [PubMed] [Google Scholar]
- 10. GBD 2017 . Risk factors collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. The Lancet 2019;1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dong C, Bu X, Liu J, et al. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: a systematic analysis of the global burden of disease study. Nutr Metab Cardiovasc Dis 2022;32:897–907. 10.1016/j.numecd.2021.11.012 [DOI] [PubMed] [Google Scholar]
- 12. Huang L, Wang Z, Wang H, et al. Nutrition transition and related health challenges over decades in China. Eur J Clin Nutr 2021;75:247–52. 10.1038/s41430-020-0674-8 [DOI] [PubMed] [Google Scholar]
- 13. He Y, Li Y, Yang X, et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol 2019;7:540–8. 10.1016/S2213-8587(19)30152-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schulz CA, Oluwagbemigun K, Nöthlings U. Advances in dietary pattern analysis in nutritional epidemiology. Eur J Nutr 2021;60:4115–30. 10.1007/s00394-021-02545-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 2002;13:3–9. 10.1097/00041433-200202000-00002 [DOI] [PubMed] [Google Scholar]
- 16. Wang DD, Nguyen LH, Li Y, et al. The gut microbiome modulates the protective association between a mediterranean diet and cardiometabolic disease risk. Nat Med 2021;27:333–43. 10.1038/s41591-020-01223-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gan ZH, Cheong HC, Tu Y-K, et al. Association between plant-based dietary patterns and risk of cardiovascular disease: a systematic review and meta-analysis of prospective cohort studies. Nutrients 2021;13:3952. 10.3390/nu13113952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kahleova H, Salas-Salvadó J, Rahelić D, et al. Dietary patterns and cardiometabolic outcomes in diabetes: a summary of systematic reviews and meta-analyses. Nutrients 2019;11:2209. 10.3390/nu11092209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang Y, Feng L, Zeng G, et al. Effects of cuisine-based Chinese heart-healthy diet in lowering blood pressure among adults in China: multicenter, single-blind, randomized, parallel controlled feeding trial. Circulation 2022;146:303–15. 10.1161/CIRCULATIONAHA.122.059045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lan Y, Wu D, Cai Z, et al. Supra-additive effect of chronic inflammation and atherogenic dyslipidemia on developing type 2 diabetes among young adults: a prospective cohort study. Cardiovasc Diabetol 2023;22. 10.1186/s12933-023-01878-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dayimu A, Wang C, Li J, et al. Trajectories of lipids profile and incident cardiovascular disease risk: a longitudinal cohort study. J Am Heart Assoc 2019;8:e013479. 10.1161/JAHA.119.013479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zhou H, Ding X, Yang Q, et al. Associations of hypertriglyceridemia onset age with cardiovascular disease and all-cause mortality in adults: a cohort study. J Am Heart Assoc 2022;11:e026632. 10.1161/JAHA.122.026632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. He M, Wang J, Liang Q, et al. Time-restricted eating with or without low-carbohydrate diet reduces visceral fat and improves metabolic syndrome: a randomized trial. Cell Rep Med 2022;3. 10.1016/j.xcrm.2022.100777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sofi F, Dinu M, Pagliai G, et al. Low-calorie vegetarian versus mediterranean diets for reducing body weight and improving cardiovascular risk profile: cardiveg study (cardiovascular prevention with vegetarian diet). Circulation 2018;137:1103–13. 10.1161/CIRCULATIONAHA.117.030088 [DOI] [PubMed] [Google Scholar]
- 25. Kahleova H, Rembert E, Alwarith J, et al. Effects of a low-fat vegan diet on gut microbiota in overweight individuals and relationships with body weight, body composition, and insulin sensitivity. a randomized clinical trial. Nutrients 2020;12:2917. 10.3390/nu12102917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Estruch R, Ros E, Salas-Salvadó J, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 2018;378:25:e34. 10.1056/NEJMoa1800389 [DOI] [PubMed] [Google Scholar]
- 27. Reynolds A, Mann J, Cummings J, et al. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. The Lancet 2019;393:434–45. 10.1016/S0140-6736(18)31809-9 [DOI] [PubMed] [Google Scholar]
- 28. Bechthold A, Boeing H, Schwedhelm C, et al. Food groups and risk of coronary heart disease, stroke and heart failure: a systematic review and dose-response meta-analysis of prospective studies. Crit Rev Food Sci Nutr 2019;59:1071–90. 10.1080/10408398.2017.1392288 [DOI] [PubMed] [Google Scholar]
- 29. Xue T, Wen J, Wan Q, et al. Association of soy food with cardiovascular outcomes and all-cause mortality in a Chinese population: a nationwide prospective cohort study. Eur J Nutr 2022;61:1609–20. 10.1007/s00394-021-02724-8 [DOI] [PubMed] [Google Scholar]
- 30. Balakrishna R, Bjørnerud T, Bemanian M, et al. Consumption of nuts and seeds and health outcomes including cardiovascular disease, diabetes and metabolic disease, cancer, and mortality: an umbrella review. Advances in Nutrition 2022;13:2136–48. 10.1093/advances/nmac077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xiao N, Zhao Y, Yao Y, et al. Biological activities of egg yolk lipids: a review. J Agric Food Chem 2020;68:1948–57. 10.1021/acs.jafc.9b06616 [DOI] [PubMed] [Google Scholar]
- 32. Ganesan K, Sukalingam K, Xu B. Impact of consumption and cooking manners of vegetable oils on cardiovascular diseases- a critical review. Trends in Food Science & Technology 2018;71:132–54. 10.1016/j.tifs.2017.11.003 [DOI] [Google Scholar]
- 33. Y Y . China Food Composition Tables. 6th edn. Beijing: Peking University Medical Press, 2018. [Google Scholar]
- 34. Yang X, Li J, Hu D, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-par project (prediction for Ascvd risk in China). Circulation 2016;134:1430–40. 10.1161/CIRCULATIONAHA.116.022367 [DOI] [PubMed] [Google Scholar]
- 35. Son D-H, Kwon Y-J, Lee HS, et al. Effects of a calorie-restricted Mediterranean-style diet on plasma lipids in Hypercholesterolemic South Korean patients. Nutrients 2021;13:3393. 10.3390/nu13103393 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-082957supp001.pdf (4.5MB, pdf)
bmjopen-2023-082957supp002.pdf (4.1MB, pdf)