Abstract
Objectives. We sought to determine whether childhood health disparities are best understood as effects of race, socioeconomic status (SES), or synergistic effects of the two.
Methods. Data from the National Health Interview Survey 1994 of US children aged 0 to 18 years (n=33911) were used. SES was measured as parental education. Child health measures included overall health, limitations, and chronic and acute childhood conditions.
Results. For overall health, activity and school limitations, and chronic circulatory conditions, the likelihood of poor outcomes increased as parental education decreased. These relationships were stronger among White and Black children, and weaker or nonexistent among Hispanic and Asian children. However, Hispanic and Asian children exhibited an opposite relationship for acute respiratory illness, whereby children with more educated parents had higher rates of illness.
Conclusions. The traditional finding of fewer years of parent education being associated with poorer health in offspring is most prominent among White and Black children and least evident among Hispanic and Asian children. These findings suggest that lifestyle characteristics (e.g., cultural norms for health behaviors) of low-SES Hispanic and Asian children may buffer them from health problems. Future interventions that seek to bolster these characteristics among other low-SES children may be important for reducing childhood health disparities.
Health disparities reflect differences in health because of sociodemographic variables, such as race, socioeconomic status (SES), and gender.1 Both racial and socioeconomic disparities in health are profoundly evident in the United States, such that Healthy People 2010—the national statement of health objectives—has made 1 of its 2 overarching goals the elimination of health disparities.1
Low-SES individuals consistently have poorer health than high-SES individuals across a variety of morbidity and mortality outcomes.2–5 Understanding these relations early in life is critical not only for maximizing children’s health but also for understanding the origins of adult disparities in health. Low SES has been associated with poorer health in childhood.6–11 For example, lower-SES children are less likely to receive vaccinations and have contact with physicians at early ages.7,12 Lower-SES children have poorer health behaviors, including higher injury rates at young ages and greater rates of smoking and sedentary behaviors.6,7
Lower-SES children also suffer from chronic impairments, such as higher rates of hospitalizations for asthma, and greater activity limitations.6,7,10 Disparities in childhood health have heavy costs. For example, on the basis of projected inability to work or lost time from work in adulthood because of illness, children living in poverty are projected to cost the United States $130 billion ($1996) in future economic output.13
Similarly, children belonging to minority groups have poorer health. For example, Black families have higher rates of low-birthweight babies and infant mortality than do White families.14–16 Black children have higher rates of elevated levels of blood lead12 and are more likely to have fair/poor health than are White children.17 Black mothers are less likely to receive prenatal care than are White mothers, and Black children are more likely to be hospitalized for conditions such as asthma.7 Fewer data have historically been available on other ethnic groups, and heterogeneity within groups makes patterns more difficult to interpret. However, there is some evidence that Hispanic and Asian children are more likely to have fair/poor health than are White children,18 and that cardiovascular risk factors such as body mass index and glycated hemoglobin levels are higher among Hispanics than among Whites.19
The vast majority of research on health disparities has focused on either SES or race and often controls for 1 factor when testing the effect of the other.5 Yet SES and race are closely intertwined, with members of many minority groups, on average, being lower in SES.20 Thus, some researchers have argued that researchers should be testing for interaction effects between race and SES.21–24
An interaction between race and SES could take a number of forms. Race and SES could interact synergistically to affect health. That is, the effects of low SES could be particularly pronounced among minority groups, perhaps if poverty effects are compounded by racism.23 The notion that individuals who belong to multiple groups facing discrimination are the most disadvantaged has been termed the double jeopardy hypothesis.25,26
Alternatively, the effects of low SES could be more pronounced among groups that are native born. This might occur because immigrants are more likely to have better health than those in the native-born population, even if they are lower in SES, a phenomenon termed the healthy immigrant effect.27,28 If Whites and Blacks are less likely to be immigrants, they may exhibit stronger relations between SES and health than other minority groups. Alternatively, if base rates of many illnesses are higher among Blacks than among Whites, a ceiling effect may exist, such that the effect of SES on health is less apparent among Blacks than among Whites.
Finally, certain SES indicators may be a poorer marker of SES among some minority groups. For example, minority group members on average do not receive the same financial gains for equivalent years of education as do Whites,22,29 which could result in Whites having a stronger SES gradient than other racial groups.
We tested our reasoning by analyzing race by SES (on the basis of parental education) interactions predicting health outcomes in a large, nationally representative sample of US children. These analyses could provide information about the utility of assessing health disparities using SES, race, or some combination of the 2.
METHODS
Sample
Data are from the National Health Interview Survey 1994, a multistage, cross-sectional household interview survey of the civilian, noninstitutionalized population of the United States, conducted by the National Center for Health Statistics. Data from children aged 0 through 18 years were included in these analyses. In most cases, a proxy adult respondent (usually the child’s mother) was used for persons younger than 19 years. Data were extracted from 1994 because this sample contained more than twice as many children (n = 33 911) as any subsequent year of National Health Interview Survey data.
A total of 20717 children were classified as White (61%), 5776 as Black (17%), 4785 as Hispanic (14%), and 1088 as Asian (3%), with the remainder classified as Other or unknown. The average age of children in this sample was 8.72 years (SD= 5.35), and 49% were female. The race groups did not differ in gender composition but did differ in age, with Hispanic children being slightly younger than other children (P < .001). Details about the design and methods of the National Health Interview Survey can be found elsewhere.30
Measures
SES.
SES was measured by the highest level of education of parents or the responsible adult in the household. SES can be measured in several ways (e.g., education, occupation, income), with each having different implications.31,32 Education was used in the present study because it is the most stable indicator of SES.5 Also, given that minorities do not receive the same financial gains for equivalent years of education as do Whites,22,29 education may be a better indicator of distribution of SES across racial groups than income.
The number of years of education was coded from 0 to 18 (18= 18 years or more). The average education of parents was 13.35 years (SD = 2.79). As expected, the racial groups differed in average education, with Whites and Asians having more years of education than Blacks and Hispanics (P < .001). SES disparities were tested by probing differences across the education gradient in child health.
Race.
Participants’ race was coded into 1 of 5 categories: White, Black, Hispanic, Asian, and Other. Because the Other category was small and not always identifiable, these participants were not included in analyses. Categories for White, Black, and Asian were created by asking respondents to identify the group that represented their child’s race. Respondents were also asked whether the child’s origin/ancestry belonged to any Hispanic groups listed. This variable was used to categorize children as Hispanic. It should be noted that there could be overlap across the 2 questions (e.g., a child being identified as both Hispanic and White). Like other researchers, we used the Hispanic coding first and then categorized non-Hispanic children according to race (thus, Whites reflect non-Hispanic Whites).7 Racial disparities were tested by comparing each minority group with Whites.
Health.
We tested 3 types of health outcomes: (1) general health ratings, (2) chronic childhood conditions, and (3) acute childhood conditions.
General health.
Respondents were asked whether the child’s health was excellent, very good, good, fair, or poor. This variable was dichotomized into those reporting fair/poor health (1) and those reporting good to excellent health (0). Activity limitations were assessed by asking whether the child was limited in any activities because of an impairment or health problem (1=limited, 0=not limited); the same question was asked for school limitations. A total of 3.2% of children were in fair/ poor health, 6.9% had activity limitations, and 8.3% had school limitations.
Chronic conditions.
We focused on the most common chronic illness in childhood (asthma) and the leading cause of death across the lifespan (cardiovascular conditions). Respondents were asked whether the child had any conditions from a list of chronic conditions randomly chosen from 6 lists. The lists are described in Massey et al.30 Respondents in the selected respiratory conditions group were asked whether the child had asthma. Respondents in the selected circulatory conditions group were asked whether the child had any cardiovascular or circulatory chronic conditions (including heart disease, high blood pressure, and cerebrovascular disease). Responses were coded as present (1) or absent (0) for asthma and for any circulatory condition. Because each list was only administered to one sixth of the sample, separate chronic conditions weights were used. A total of 7.1% of children had asthma, and 2.3% had a circulatory condition.
Acute conditions.
We focused on the leading childhood cause of deaths and years of productive life lost (injuries), and the most common type of acute illness in childhood (respiratory conditions). Respondents were asked whether the child had an injury that limited activity or resulted in medical attention in the previous 2 weeks. The same question was asked for acute respiratory illnesses (including colds, flu, acute bronchitis, pneumonia). Responses for all conditions were coded as present (1) or absent (0). A total of 1.4% of children had an injury, and 5.0% had an acute respiratory illness in the previous 2 weeks.
Data Analysis
Analyses were conducted with Stata/SE Version 8.2 software (Stata Corp, College Station, Tex), with weighted data to adjust for survey design effects because of clustered sampling and oversampling of certain groups. Logistic regression analyses were conducted to predict dichotomous health outcomes from SES and race variables. An interaction term was created by multiplying SES (years of parental education) by racial group (3 indicator variables for Blacks, Hispanics, and Asians).
With this coding, Whites served as the reference group. To test associations of health with education and race, health outcomes were first regressed onto parental education and race variables simultaneously. Second, to test whether parental education–health relations varied by race, health outcomes were regressed onto education, race, and the interaction term for education and race simultaneously. Age and gender were included as covariates in all analyses. Rates for figures were calculated with the prediction equation from the estimated logistic regression (presence/ absence of illness regressed on race and education). Rates are described as prevalence for outcomes that are chronic/stable (general health, limitations, chronic conditions), and as incidence for outcomes that occurred in the previous 2 weeks (injury, respiratory illness).
RESULTS
Table 1 ▶ presents the coefficients from the logistic regression analyses. For fair/poor health, the significant effect of education indicates that children from less educated families were more likely to be in fair/poor health. Significant effects of race were seen for Blacks, Hispanics, and Asians, such that children from each minority group were more likely to be rated in fair/poor health than were White children. The education-by-race interaction effect was not significant for Blacks compared with Whites, indicating that both White and Black children had similar education gradients for fair/poor health. The education-by-race interaction effect was significant for Hispanics compared with Whites (P < .001) and for Asians compared with Whites (at the P = .08 level), indicating that education gradients for Hispanics and Asians were less steep for fair/poor health than they were for Whites.
TABLE 1—
Logistic Regression Analyses Testing Effects of Parental Education and Race on Children’s Health: US National Health Interview Survey, 1994
| Regression Coefficient | Standard Error | P | |
| Fair/poor health | |||
| Education | −0.15 | 0.01 | <.001 |
| Race | |||
| Black | 0.70 | 0.08 | <.001 |
| Hispanic | 0.30 | 0.10 | <.01 |
| Asian | 0.41 | 0.18 | <.05 |
| Education × race | |||
| Black | 0.04 | 0.03 | ns |
| Hispanic | 0.11 | 0.03 | <.001 |
| Asian | 0.06 | 0.03 | .08 |
| Activity limitations | |||
| Education | −0.07 | 0.01 | <.001 |
| Race | |||
| Black | 0.25 | 0.06 | <.001 |
| Hispanic | −0.31 | 0.08 | <.001 |
| Asian | −1.20 | 0.20 | <.001 |
| Education × race | |||
| Black | −0.01 | 0.02 | ns |
| Hispanic | 0.12 | 0.02 | <.001 |
| Asian | 0.15 | 0.05 | <.01 |
| School limitations | |||
| Education | −0.06 | 0.01 | <.001 |
| Race | |||
| Black | 0.20 | 0.07 | <.01 |
| Hispanic | −0.35 | 0.09 | <.001 |
| Asian | −1.18 | 0.22 | <.001 |
| Education × race | |||
| Black | −0.01 | 0.03 | ns |
| Hispanic | 0.12 | 0.02 | <.001 |
| Asian | 0.14 | 0.06 | <.05 |
| Chronic condition: asthma | |||
| Education | 0.02 | 0.02 | ns |
| Race | |||
| Black | 0.18 | 0.15 | ns |
| Hispanic | −0.17 | 0.18 | ns |
| Asian | 0.03 | 0.33 | ns |
| Education × race | |||
| Black | −0.01 | 0.06 | ns |
| Hispanic | 0.01 | 0.05 | ns |
| Asian | 0.13 | 0.10 | ns |
| Chronic circulatory condition | |||
| Education | −0.01 | 0.03 | ns |
| Race | |||
| Black | −0.12 | 0.28 | ns |
| Hispanic | −0.06 | 0.32 | ns |
| Asian | −1.14 | 1.01 | ns |
| Education × race | |||
| Black | −0.12 | 0.08 | ns |
| Hispanic | 0.23 | 0.08 | <.01 |
| Asian | 0.13 | 0.05 | <.05 |
| Acute injury | |||
| Education | 0.03 | 0.02 | ns |
| Race | |||
| Black | −0.46 | 0.16 | <.01 |
| Hispanic | −0.25 | 0.16 | .10 |
| Asian | −1.52 | 0.60 | <.05 |
| Education × race | |||
| Black | −0.04 | 0.07 | ns |
| Hispanic | 0.01 | 0.04 | ns |
| Asian | 0.09 | 0.12 | ns |
| Acute respiratory illness | |||
| Education | 0.04 | 0.01 | <.001 |
| Race | |||
| Black | −0.54 | 0.09 | <.001 |
| Hispanic | 0.00 | 0.08 | ns |
| Asian | 0.07 | 0.14 | ns |
| Education × race | |||
| Black | −0.03 | 0.04 | ns |
| Hispanic | 0.12 | 0.03 | <.001 |
| Asian | 0.07 | 0.04 | .13 |
Note. Education = years of parental education; ns = not significant. Reference group for all race coefficients is Whites. Health outcomes: 0 = no problem, 1 = presence of health problem. Regression coefficients for race and education reflect these 2 variables entered simultaneously with age and gender as covariates. Coefficients for the interaction terms reflect interaction effects when entered simultaneously with race and education, and with age and gender as covariates.
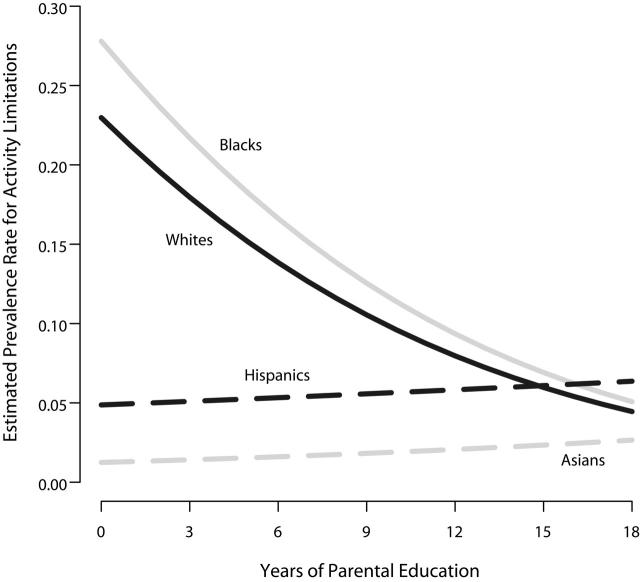
With respect to activity and school limitations, children from less educated families were more likely to have both activity and school limitations. Blacks were more likely to have activity and school limitations than were Whites, whereas Hispanics and Asians were less likely to have activity and school limitations than were Whites. In addition, there were significant interaction effects of education by race for both activity and school limitations when comparing Hispanics and Asians to Whites, but not when comparing Blacks to Whites. This interaction, depicted in Figure 1 ▶, revealed that the education gradient was similar for Blacks and Whites but was steeper for Whites than for Hispanics and Asians (all P’s were < .05). In follow-up analyses with Blacks as the reference group, we found a similar pattern of a steeper education gradient for Blacks than for Hispanics and Asians (P ’s were < .01).
FIGURE 1—
Parental education × race interaction for activity limitations.
Note. The education line was significant among White and Black children (P’s were <.001) but not for Hispanic and Asian children.
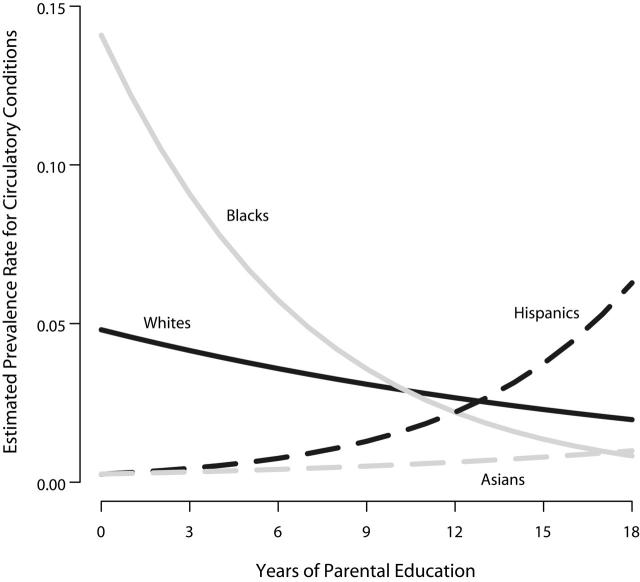
For chronic conditions, there were no significant effects of education or race on asthma. For chronic circulatory conditions, there was an interaction effect of education by race for Hispanics and Asians compared with Whites, but not for Blacks compared with Whites. This interaction effect, depicted in Figure 2 ▶, revealed that Blacks and Whites had similar education gradients, but that Whites had significantly different education gradients than Hispanics and Asians (P ’s were < .05). When Blacks were used as the reference group, we found a similar pattern of a steeper negative education gradient for Blacks compared with Hispanics and Asians (P ’s were < .01).
FIGURE 2—
Parental education × race interaction for chronic circulatory conditions.
Note. The education line was significant and negative among Black children (P < .05) but significant and positive among Hispanic and Asian children (P’s were <.05).
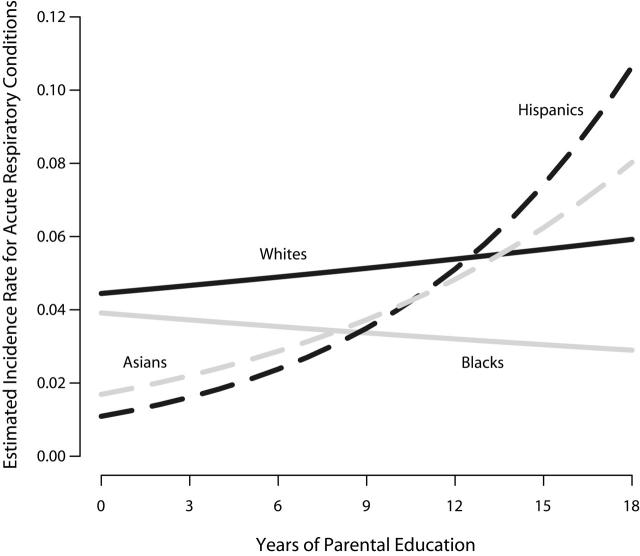
For acute childhood conditions, Blacks and Asians were less likely to report injuries than were Whites. No effects of education or interaction effects were found. For acute respiratory illness, Blacks were less likely to have a respiratory illness than were Whites. Children from more educated families were more likely to have a respiratory illness. In addition, a significant education-by-race interaction effect was found when Hispanics were compared with Whites. This effect, depicted in Figure 3 ▶, revealed that Hispanics had steeper positive gradients than did Whites (P < .001). When Blacks were used as the reference group, we found a similar pattern of steeper positive education gradients for Hispanics compared with Blacks (P < .001) and for Asians compared with Blacks (at the P = .06 level).
FIGURE 3—
Parental education × race interaction for acute respiratory illnesses.
Note. The education line was not significant among White and Black children but was significant for Hispanic and Asian children (P’s were <.05)
DISCUSSION
Our results illustrate that race and SES effects on child health are best understood in concert, rather than separately. That is, although parental education was related to child health, these differences were actually apparent only among certain racial groups. The traditional relation of fewer years of parental education with poorer health emerged among White and Black children in terms of overall health, activity and school limitations, and chronic circulatory conditions (in this case, for Blacks). In contrast, the education gradient was often not present among Hispanic and Asian children (e.g., activity limitations), and in some cases was reversed (e.g., acute respiratory illnesses).
The outcomes that we measured for Hispanic and Asian children were similar to each other but different from White and Black children, which suggests that the different gradients across racial groups may be because of social and cultural values that vary by group. For example, both Hispanic and Asian cultures have extensive close social networks and are interdependent cultures (e.g., valuing and thinking in terms of the group rather than the individual).33–35 This could result in Hispanic and Asian families sharing health beliefs and practicing health behaviors across SES groups, leading to a diminished effect of low parental education within these groups.
Alternatively, education gradients may be affected by immigration patterns. Hispanic and Asian children may be more likely to come from immigrant families than are White or Black children. If true, the present study suggests that the healthy immigrant hypothesis also has implications for education relations with health. That is, it is not just that immigrant groups are on average healthier; rather, immigrant groups may also be less susceptible to the effects of low education.
These patterns have important implications. First, it suggests that low parental education does not destine children to poor health; rather, because Hispanic and Asian children who are low in parental education maintain healthy outcomes, there may be factors that can buffer the impact of low education on child health, such as the role of social networks. Better understanding of these factors may allow us to intervene with other low-SES children to improve health outcomes early in life. Second, in terms of establishing public health priorities, it suggests that efforts to eliminate socioeconomic health disparities may be most effective through _targeting specific populations, such as White and Black children.
Our findings are consistent with previous child health research. For example, descriptive figures suggest larger gradients for low birthweight and infant mortality among Black and White children than among Hispanic or Asian children.7 Similar relations among Black and White children have also been found with parental education and child overall health and school-loss days.36 In addition, White youths have the strongest SES relation with smoking19 and obesity.37,38 Overall these patterns support the notion of childhood SES and health gradients, particularly among White children.
Our analyses showed no effect of either parental education or race on asthma prevalence rates. One possible explanation is the “hygiene hypothesis,” the notion that a decrease in childhood exposure to microbes and infections may increase the predisposition to chronic allergic conditions such as asthma.39–41 If children with higher SES are exposed to these more hygienic environments early in life, this may balance out other environmental characteristics (e.g., exposure to toxins) that are detrimental for many lower-SES children, resulting in no education differences for asthma.
White children were more likely to experience an injury than were minority children. White children are more likely to participate in sports than are Hispanic or Asian children, which may account for some of the racial differences in injuries.42 In contrast, no education effects were found for injuries. Although this is inconsistent with patterns found among younger children,6 high-SES adolescents have been found to participate in more activity-oriented lessons and sports teams than low-SES adolescents, presumably because of costs.43 If higher-SES older children are exposed to more situations with the potential for injury, this may result in no clear education differences in injuries across all of childhood.
Our study also found that in some cases, Hispanic and Asian children exhibited a reverse education gradient. Specifically, Hispanic and Asian children with more educated parents had higher rates of acute respiratory illnesses. It is possible that more educated Hispanic and Asian parents are more knowledgeable about different types of respiratory illnesses (e.g., pneumonia, bronchitis) and thus, identify them more frequently. It is also possible that higher-SES Hispanic and Asian families have greater access to health care7 that makes them more likely to take their child to the doctor for acute respiratory illnesses.
Limitations to the present study included having no direct measure of immigrant status or acculturation. Thus, we do not know the numbers of immigrants within racial/ ethnic groups and cannot directly test whether immigrant status, years since immigration, or acculturation explains the study findings. Further research is also needed to test differences in health among immigrants who are first generation versus second or higher generation.
Second, future studies that measure a variety of behavioral and social factors are needed to determine the characteristics that buffer low-SES Hispanic and Asian children from poor health. Last, the present study included only 1 measure of SES, parental education. This indicator is quite stable over time and thus may describe longer-lasting effects of parental SES on child health. Parental education may suggest pathways related to health knowledge; however, it does not tell us about the impact of other SES characteristics such as financial resources. Strengths of our study, however, include the use of a national probability sample weighted appropriately for clustered sampling and oversampling of specific groups, allowing us to document SES and race health disparities across US children.
Understanding childhood health disparities is critical to improving America’s health. The average-age child in our sample (9 years old) who comes from a low-SES family is estimated to have 6 years’ less life expectancy than a high-SES child.44 Our findings demonstrate that parental education and child health gradients are strongest among White and Black children and weaker or reversed among Hispanic and Asian children. Designing future interventions that incorporate the protective factors of low-SES Hispanic and Asian children may help improve the health of all children and maximize the healthy and productive years of adults across the SES spectrum.
Acknowledgments
This study was funded by the National Institute of Child Health and Human Development (grant HD43652).
Human Participant Protection This study was approved by the research ethics board at the University of British Columbia, Vancouver.
Peer Reviewed
Contributors E. Chen initiated the study, planned data analyses, and wrote the article. A. D. Martin conducted statistical analyses and assisted with data interpretation. K. A. Matthews contributed to study conceptualization, data interpretation, and writing of the article.
References
- 1.Healthy People 2010: Understanding and Improving Health. Washington, DC: US Department of Health and Human Services; 2000.
- 2.Adler NE, Boyce T, Chesney MA, et al. Socioeconomic status and health: the challenge of the gradient. Am Psychol. 1994;49:15–24. [DOI] [PubMed] [Google Scholar]
- 3.Adler NE, Boyce WT, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health: no easy solution. JAMA. 1993;269:3140–3145. [PubMed] [Google Scholar]
- 4.Marmot MG, Shipley MJ, Rose G. Inequalities in death- specific explanations of a general pattern? Lancet. 1984;1:1003–1006. [DOI] [PubMed] [Google Scholar]
- 5.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Sociol. 1995;21:349–386. [Google Scholar]
- 6.Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: how and why do these relationships change with age? Psychol Bull. 2002;128: 295–329. [DOI] [PubMed] [Google Scholar]
- 7.Pamuk E, Makuc D, Heck K, Reuben C, Lochner K. Socioeconomic Status and Health Chartbook. Health, United States, 1998. Hyattsville, Md: National Center for Health Statistics; 1998.
- 8.Starfield B, Riley AW, Witt WP, Robertson J. Social class gradients in health during adolescence. J Epidemiol Community Health. 2002;56:354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newacheck PW. Poverty and childhood chronic illness. Arch Pediatr Adolesc Med. 1994;148: 1143–1149. [DOI] [PubMed] [Google Scholar]
- 10.Egbuonu L, Starfield B. Child health and social status. Pediatrics. 1982;69:550–557. [PubMed] [Google Scholar]
- 11.Starfield B, Robertson J, Riley AW. Social class gradients and health in childhood. Ambulatory Pediatr. 2002;2:238–246. [DOI] [PubMed] [Google Scholar]
- 12.Starfield B. Child health care and social factors: poverty, class, race. Bull N Y Acad Med. 1989;65: 299–306. [PMC free article] [PubMed] [Google Scholar]
- 13.Sherman A. Poverty Matters: The Cost of Child Poverty in America. Washington DC: Children’s Defense Fund; 1997.
- 14.Starfield B, Shapiro S, Weiss J, et al. Race, family income, and low birthweight. Am J Epidemiol. 1991; 134:1167–1174. [DOI] [PubMed] [Google Scholar]
- 15.Schoendorf KC, Hogue CJR, Kleinman JC, Rowley D. Mortality among infants of black as compared with white college-educated parents. N Engl J Med. 1992; 326:1522–1560. [DOI] [PubMed] [Google Scholar]
- 16.Hogue CJR, Hargraves MA. Class, race, and infant mortality in the United States. Am J Public Health. 1993;83:9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montgomery LE, Kiely JL, Pappas G. The effects of poverty, race, and family structure on US children’s health: data from the NHIS, 1978 through 1980 and 1989 through 1991. Am J Public Health. 1996;86: 1401–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flores G, Bauchner H, Feinstein AR, Nguyen UDT. The impact of ethnicity, family income, and parental education on children’s health and use of health services. Am J Public Health. 1999;89:1066–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winkleby MA, Robinson TN, Sundquist J, Kraemer HC. Ethnic variation in cardiovascular disease risk factors among children and young adults: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1999;281:1006–1013. [DOI] [PubMed] [Google Scholar]
- 20.Economic Report of the President. Washington, DC: US Government Printing Office; 1998.
- 21.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 22.Williams DR. Racial/ethnic variations in women’s health: the social embeddedness of health. Am J Public Health. 2002;92:588–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kessler RC, Neighbors HW. A new perspective on the relationships among race, social class, and psychological distress. J Health Soc Behav. 1986;27:107–115. [PubMed] [Google Scholar]
- 24.Pettigrew TF. Race and class in the 1980S: an interactive view. Daedalus. 1981;110:233–255. [Google Scholar]
- 25.Levin S, Sinclair S, Veniegas RC, Taylor PL. Perceived discrimination in the context of multiple group memberships. Psychol Sci. 2002;13:557–560. [DOI] [PubMed] [Google Scholar]
- 26.Ferraro KF, Farmer MM. Double jeopardy to health hypothesis for African Americans: analysis and critique. J Health Soc Behav. 1996;37:27–43. [PubMed] [Google Scholar]
- 27.Hummer RA, Rogers RG, Nam CB, LeClere FB. Race/ethnicity, nativity, and US adult mortality. Soc Sci Q. 1999;80:136–153. [Google Scholar]
- 28.Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86:837–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaufman JS, Cooper RS, McGee DL. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8:621–628. [PubMed] [Google Scholar]
- 30.Massey JT. Overview of the National Health Interview Survey and its sample design. Vital Health Stat 2. 1989; No. 110:1–5. [PubMed] [Google Scholar]
- 31.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Ann Rev Public Health. 1997;18:341–378. [DOI] [PubMed] [Google Scholar]
- 32.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82: 816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marin G, Marin BV. Research With Hispanic Populations. Newbury Park, Calif: Sage; 1991.
- 34.Markus HR, Kitayama S. Culture and the self: implications for cognition, emotion, and motivation. Psychol Rev. 1991;98:224–253. [Google Scholar]
- 35.Heine SJ. Self as cultural product: an examination of East Asian and North American selves. J Pers. 2001; 69:881–906. [DOI] [PubMed] [Google Scholar]
- 36.McGauhey PJ, Starfield B. Child health and the social environment of white and black children. Soc Sci Med. 1993;36:867–874. [DOI] [PubMed] [Google Scholar]
- 37.Gordon-Larsen P, Adair LS, Popkin BM. The relationship of ethnicity, socioeconomic factors, and overweight in US adolescents. Obes Res. 2003;11:121–129. [DOI] [PubMed] [Google Scholar]
- 38.Kimm SYS, Obarzanek E, Barton BA, et al. Race, socioeconomic status, and obesity in 9- to 10-year-old girls: the NHLBI Growth and Health Study. Ann Epidemiol. 1996;6:266–275. [DOI] [PubMed] [Google Scholar]
- 39.Strachan DP. Hay fever, hygiene, and household size. BMJ. 1989;299:1259–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strachan DP. Family size, infection and atopy: the first decade of the “hygiene hypothesis.” Thorax. 2000; 55(suppl 1):S2–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Braun-Fahrlander C, Riedler J, Herz U, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med. 2002; 347:869–877. [DOI] [PubMed] [Google Scholar]
- 42.Videon TM. Whoplays and who benefits: gender, interscholastic athletics, and academic outcomes. Sociol Perspect. 2002;45:415–444. [Google Scholar]
- 43.Sallis JF, Zakarian JM, Hovell MF, Hofstetter CR. Ethnic, socioeconomic, and sex differences in physical activity among adolescents. J Clin Epidemiol. 1996;49: 125–134. [DOI] [PubMed] [Google Scholar]
- 44.Kubzansky LD, Krieger N, Kawachi I, Rockhill B, Steel GK, Berkman LF. United States: social inequality and the burden of poor health. In: Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M, eds. Challenging Inequities in Health. New York, NY: Oxford University Press; 2001.