Abstract
Purpose
The present study examined whether the health–survival paradox could partially be due to sex-specific selection and information bias in surveys.
Methods
The study is based on the linkage of three population-based surveys of 15,330 Danes aged 46–102 years with health registers covering the total Danish population regarding hospitalizations within the last 2 years and prescription medicine within 6 months prior to the baseline surveys.
Results
Men had higher participation rates than women at all ages. Hospitalized women and women taking medications had higher participation rate compared with non-hospitalized women (difference 0.7–3.0%) and female non-users (difference 0.8–7.6%), respectively, while no consistent pattern was found among men according to hospitalization or medication use status. Men used fewer medications than women, but they under-reported medication use to a similar degree as did women.
Conclusions
Hospitalized women, as well as women using prescription medicine, were slightly overrepresented in the surveys. Hence, the study found some evidence that selection bias in surveys may contribute to the explanation of the health–survival paradox, but its contribution is likely to be small. However, there was no evidence for sex-specific reporting of medication use among study participants.
Keywords: sex differences, health, mortality, paradox, non-response, register study, healthcare utilization, hospitalization, medication use, Denmark
Background
In almost all western countries, men report better health than females (1, 2), but women still outlive men in all countries around the world (3). Among the most widely cited explanations for this apparent contradiction are favorable effects of estrogen on serum lipids (4), the compensatory effect of the second X chromosome (5, 6), a lower ability of the male immune system to avoid the harmful effects of infections (7), a relatively higher compatibility of sick roles with other female responsibilities, engagement in more risk-taking behavior among men, as well as better awareness of disease symptoms, timely seeking for medical advice (8, 9) and over-reporting of worse health among women (10, 11). The distribution of chronic diseases has been also proposed to contribute to the health–survival paradox (2, 12).
Despite mounting research regarding sex differences in health and mortality, we still do not fully understand the reasons for the paradox or its mechanisms. In addition to the fundamental biological and behavioral differences, the paradox can partially be due to bias in surveys if men are more reluctant than women to participate and/or accurately report in surveys if they have disabilities or diseases.
In the present study we utilized a unique opportunity to link three Danish surveys covering 15,330 individuals aged 46–102 years with the extensive register information on the complete Danish population. We hypothesized that unhealthy men will be less willing to participate in surveys than their female counterparts. If so, this would lead to a bias, resulting in underestimating the health problems in surveyed men. The study also aimed to test whether there is sex-specific information bias in the surveys by comparing self-reported medication use with prescribed medications recorded in the registers. We hypothesized that women and men will have a similar reporting pattern for major medications, e.g. cardiovascular, but women will have more accurate reporting of nervous and musculoskeletal system medications.
Materials and methods
The study is based on the linkage of the Study of Middle-Aged Danish Twins (MADT), the Longitudinal Study of Aging Danish Twins (LSADT), and the Danish 1905–Cohort Study with registers within Statistics Denmark. The studies are described in detail elsewhere (13–15). In brief, the MADT represented a random sample of 120 twin pairs from each birth cohort from 1931 to 1952, aged 46–68 years in 1998 when the survey was implemented. The LSADT involved the Danish twins aged 75 years and older by January 1995, and residing in Denmark. Twins aged at least 70 years were added to the 1997, 1999 and 2001 follow-ups (16). The 1905–Cohort Study included all Danes born in 1905 and alive in 1998. In all surveys the individuals residing in nursing homes or sheltered accommodation were considered eligible to participate in the study. If persons refused or were unable to participate in the face-to-face interview, a proxy respondent, usually a close relative, was sought.
All three studies are comparable with regard to the design, implementation and data collection instrument with only minor differences, mainly related to age distributions in the three surveys. The instrument consisted of various questions on health, lifestyle and socio-economic conditions, tests of cognitive and physical functioning, and the collection of biological samples. Data collection in each wave was carried out within approximately 3 months.
Register linkage
Since 1968 all residents of Denmark have been identified by a unique 10-digit identification number – the Civil Registration Number (CPR number) – that can be linked to thematically organized databases (called ‘registers’) within Statistics Denmark. All individuals who were invited to participate in the three studies were identified and linked to the Danish Demographic Database (includes information on birth, sex, death and migration); the National Patient Register (includes type and date of hospital admissions, diagnoses (8th International Classification of Diseases (ICD-8) until 1993 and ICD-10 since 1994), and other information for non-psychiatric illnesses since 1977); and the Prescription Medicine Register (contains the Anatomical Therapeutic Chemical classification system (ATC) codes of prescribed medications, dates of purchase and other related information since 1995). The drugs administered in hospitals are reported on the ward level rather than individual and, therefore, were omitted in the present analysis. Using CPR numbers the register data were combined with variables identifying participation in the surveys.
Non-response variables
Non-response was defined as non-participation in the intake survey for any reason other than death or emigration from the country. Proxy interviews were considered to be non-respondents, as proxies are often spouses and could confound the analysis of sex differences in the response pattern.
Hospitalization and medication use variables
All-cause and diagnosis-specific hospitalizations within 2 years prior to the baseline were selected as the operational measures of morbidity. This time period was selected in accordance with a 2-year interval between consecutive waves in the LSADT and 1905–Cohort Study. All-cause hospitalization included all inpatient admissions except ICD-8 Y-list (unique for the Danish healthcare system) and ICD-10 Z00–Z99. The total cardiovascular diseases (CVDs) hospitalization included all inpatient admissions with primary diagnoses ICD-8 390–459, 745–747 and ICD-10 I00–I99, Q20–Q28. Cancer hospitalization (apart from skin cancer) included all admissions for primary diagnoses ICD-8 140–171, 174–199, 201–207 and ICD-10 C00–C41, C45–C97.
All-cause and cardiovascular system medications use (ATC-C) was assessed within 6 months prior to the intake, as the information letter was usually sent weeks before the interview. Due to the availability of the Prescription Medicine Register only since 1995, the non-participation analyses for LSADT start with 1997 wave for medicine use. The interview dates were used to define the start and end of the 2-year/6-month interval. For non-respondents the first dates of the corresponding surveys were used.
Measurement of information bias
Information bias was evaluated by comparing the mean number of registered and reported medications. The comparison was made for all-cause, ATC-C, musculoskeletal (ATC-M), nervous (ATC-N) and respiratory (ATC-R) system medications.
The information on medication use in surveys was obtained by asking the participants to list all medicines that they take on a regular basis or to present to an interviewer their drug storage. All prescribed medications reported by the participants were assigned the ATC code by a pharmacologist and the number of reported medications was calculated as a total count of all prescribed medications, except alternative medications and vitamins. The number of prescribed all-cause medications from the register data was calculated as a total count of all medications prescribed within the 6 months after intake.
To account for possible changes of a medication within a pharmacological group, a medication was counted only once if the person was prescribed different drugs of the same pharmacological subgroup or the same drug multiple times within the selected time period. We also estimated a number of prescribed all-cause medications 6 months before and 3 months before and after the baseline, but the three methods yielded similar results. Previous research in Demark suggests that medication use within 6 months after the survey represents a more accurate measurement of actual medicine use (17).
Statistical analysis
Logistic regression was used to analyze the impact of prior hospitalization and medication use on response pattern, adjusted for age and sex, where appropriate. The estimates are presented in odds ratios (ORs) and 95% confidence intervals (CIs). All diagnosis-specific hospitalization/system-specific medication use variables were grouped as follows: 1- non-hospitalized/non-user, 2-hospitalized for specific diagnosis (cancer or total CVD)/ATC-C user and 3 – other diagnoses/other-ATC user. To elucidate sex differences in the response pattern the interaction between hospitalization or medication use variables and sex was included using non-hospitalized men or male non-users as the reference category. To correct for the correlated nature of twin data the robust regression for all equations was used controlling for cluster by twin pair (Intercooled Stata 9.0, StataCorp, College Station, TX).
Results
Response rate
In total, 5203 individuals were invited to participate in the MADT (mean age ± standard deviation [SD]: 56.9 ± 6.3) and 6535 eligible individuals were invited for the LSADT intake participation (77.4 ± 5.6). In the 1905–Cohort Study, 3600 elderly individuals (92.9 ± 0.41) were invited to intake survey. We were unable to track in the Statistics Denmark registers only 6 individuals from the MADT and 8 from the LSADT.
The age- and sex-specific response rates are presented in Table 1. Generally, men had higher participation rates than women. Participation rates tended to decrease with advanced age except for the LSADT.
Table 1.
Participation rates in the Study of Middle-Aged Danish Twins, the Longitudinal Study of Aging Danish Twins and the Danish 1905-Cohort Study
| Study | Age groups (y) | Men (% [n]) | Women (% [n]) | Total (% [n]) |
|---|---|---|---|---|
| MADTa | n=2597 | n=2606 | n=5203 | |
| 46–49 | 82.4 (398) | 81.4 (393) | 81.9 (791) | |
| 50–54 | 86.3 (515) | 83.0 (499) | 84.6 (1014) | |
| 55–59 | 85.2 (506) | 80.5 (467) | 82.9 (973) | |
| ≥60 | 84.1 (776) | 80.2 (755) | 82.1 (1531) | |
| Total | 84.5 (2195) | 81.1 (2114) | 82.8 (4309) | |
|
| ||||
| LSADT | n=2548 | n=3979 | n=6527 | |
| 70–74 | 70.4 (816) | 61.1 (909) | 65.2 (1725) | |
| 75–79 | 73.3 (576) | 70.7 (905) | 71.2 (1481) | |
| ≥80 | 75.1 (453) | 66.7 (808) | 69.5 (1261) | |
| Total | 72.4 (1845) | 65.9 (2622) | 72.4 (4467) | |
|
| ||||
| c1905 | n=849 | n=2751 | n=3600 | |
| 92–93 | 58.2 (494) | 47.9 (1320) | 50.4 (1814) | |
MADT – the Study of Middle-Aged Danish Twins, LSADT – the Longitudinal Study of Aging Danish Twins, c1905– the Danish 1905–Cohort Study
All-cause and diagnosis-specific hospitalization and response pattern
The data analysis revealed that hospitalized women had higher participation rates compared with non-hospitalized women at all age groups except the 80–89 age group. Non-hospitalized men had higher participation rates in the 70–79 and 80–89 age groups, while the reverse pattern was observed in the youngest and oldest-old ages (Table 2).
Table 2.
Participation rates at the intake by all-cause hospitalization and medication use status in the Study of Middle-Aged Danish Twins, the Longitudinal Study of Aging Danish Twins and the Danish 1905-Cohort Study
| Men (95%CI)a | Women (95%CI) | |||
|---|---|---|---|---|
| Hospitalization status | Non-hosp | Hospitalized | Non-hosp | Hospitalized |
| Age groups (y) | ||||
| 46–59 | 84.4 (82.5, 86.2) | 87.2 (81.9, 91.4) | 81.2 (79.1, 83.3) | 84.2 (79.9, 88.6) |
| 60–69 | 83.7 (80.8, 86.2) | 84.8 (78.7, 89.8) | 79.7 (76.7, 82.5) | 80.8 (74.0, 86.5) |
| 70–79 | 72.7 (70.2, 75.1) | 69.3 (65.5, 72.9) | 65.4 (63.3, 67.5) | 66.1 (62.4, 69.5) |
| 80–89 | 76.2 (71.4, 80.6) | 74.2 (67.8, 79.9) | 69.1 (65.4, 72.6) | 66.6 (61.7, 71.2) |
| ≥90 | 57.5 (53.1, 61.7) | 60.8 (55.6, 65.9) | 47.8 (45.5, 50.2) | 49.2 (46.3, 52.2) |
|
| ||||
| Medication use status | Non-users | All-cause users | Non-users | All-cause users |
|
| ||||
| Age groups (y) | ||||
| 46–59 | 85.7 (83.2, 88.0) | 83.8 (81.1, 86.2) | 79.2 (75.5, 82.5) | 82.9 (80.5, 85.0) |
| 60–69 | 82.0 (77.5, 86.0) | 84.9 (81.8, 87.7) | 77.1 (71.1, 82.4) | 80.8 (77.7, 83.6) |
| 70–79 | 73.3 (68.8, 77.6) | 72.0 (69.5, 74.5) | 65.1 (60.3, 69.7) | 65.9 (63.8, 68.1) |
| 80–89 | 90.0 (80.5, 95.9) | 75.5 (70.5, 80.1) | 73.7 (63.6, 82.2) | 76.7 (73.2, 79.9) |
| ≥90 | 55.1 (43.4, 66.4) | 59.7 (56.3, 63.1) | 41.6 (35.3, 48.1) | 49.2 (47.3, 51.1) |
CI – confidence interval
Logistic regression showed that women regardless of hospitalization status had increased risks of non-response in the three studies (Table 3), but the risk of non-response was the highest in non-hospitalized women. Only in the LSADT women with all-cause hospitalizations and non-hospitalized women had similar risks of non-response. Men with all-cause hospitalizations had lower risks of non-response in the MADT and 1905-Cohort Study, but they had an elevated risk of non-response (OR=1.18, CI: 0.99, 1.42) in the LSADT.
Table 3.
Risk of non-response at intake by all-cause hospitalization in the Study of Middle-Aged Danish Twins, the Longitudinal Study of Aging Danish Twins and the Danish 1905-Cohort Study
| Surveys | Sample No (%) | Total, model 1a OR (95% CI) | Total, model 2 OR (95% CI) | Men OR (95% CI) | Women OR (95% CI) |
|---|---|---|---|---|---|
| MADTb | 5203 | ||||
| None | 1 | 1 | 1 | ||
| Hospitalization | 788 (15.2) | 0.85 (0.69, 1.05) | 0.84 (0.61, 1.15) | 0.85 (0.64, 1.14) | |
| Women | 2606 (50.1) | 1.27 (1.09, 1.49) | |||
| 46–49 | 1 | 1 | 1 | 1 | |
| 50–54 | 0.82 (0.64, 1.06) | 0.82 (0.64, 1.06) | 0.75 (0.52, 1.07) | 0.89 (0.63, 1.28) | |
| 55–59 | 0.94 (0.73, 1.21) | 0.94 (0.73, 1.21) | 0.82 (0.57, 1.17) | 1.06 (0.75, 1.51) | |
| ≥60 | 0.99 (0.79, 1.25) | 0.99 (0.79, 1.25) | 0.89 (0.65, 1.24) | 1.09 (0.79, 1.51) | |
| Non-hosp. men | 2209 (42.5) | 1 | |||
| Hosp. men | 388 (7.5) | 0.84 (0.61, 1.15) | |||
| Non-hosp. | 2206 (42.4) | ||||
| women | 1.27 (1.07, 1.50) | ||||
| Hosp. women | 400 (7.7) | 1.09 (0.81, 1.46) | |||
|
| |||||
| LSADT | 6527 | ||||
| None | 1 | 1 | 1 | ||
| Hospitalization | 1995 (30.6) | 1.08 (0.96, 1.21) | 1.18 (0.99, 1.42) | 1.02 (0.88, 1.18) | |
| Women | 3979 (60.9) | 1.39 (1.24, 1.57) | |||
| 70–74 | 1 | 1 | 1 | 1 | |
| 75–79 | 0.72 (0.63, 0.83) | 0.72 (0.63, 0.83) | 0.86 (0.69, 1.07) | 0.65 (0.55, 0.78) | |
| ≥80 | 0.78 (0.68, 0.90) | 0.79 (0.68, 0.90) | 0.78 (0.62, 0.98) | 0.78 (0.65, 0.93) | |
| Non-hosp. men | 1702 (26.1) | 1 | |||
| Hosp. men | 846 (13.0) | 1.18 (0.99, 1.42) | |||
| Non-hosp. | 2830 (43.4) | ||||
| women | 1.46 (1.27, 1.69) | ||||
| Hosp. women | 1149 (17.6) | 1.49 (1.26, 1.77) | |||
|
| |||||
| c1905 | 3600 | ||||
| None | 1 | 1 | 1 | ||
| Hospitalization | 1423 (39.5) | 0.92 (0.81, 1.05) | 0.83 (0.63, 1.10) | 0.95 (0.82, 1.11) | |
| Women | 2751 (76.4) | 1.51 (1.29, 1.76) | |||
| Non-hosp. men | 497 (13.8) | 1 | |||
| Hosp. men | 352 (9.8) | 0.83 (0.63, 1.10) | |||
| Non-hosp. | 1680 (46.7) | ||||
| women | 1.43 (1.17, 1.74) | ||||
| Hosp. women | 1071 (29.8) | 1.36 (1.10, 1.68) | |||
Model 1 – all-cause hospitalization, sex, age, Model 2 – Model 1 + all-cause hospitalization*sex interaction
MADT – the Middle-Age Danish Twins Study, LSADT – the Longitudinal Study of Aging Danish Twins, c1905 – the Danish 1905-Cohort Study, OR – odds ratio; CI – confidence interval
The analysis of diagnosis-specific hospitalizations prior to intake revealed that men with cancer hospitalizations had higher risks of non-response than non-hospitalized men, whereas there was no clear pattern among men with total CVD hospitalization. Women regardless of diagnose-specific hospitalization status had consistently elevated risks of non-response compared with non-hospitalized men, being the highest among women hospitalized for cancer or CVD in the twin samples (Supplementary Tables 1 and 2).
All-cause and system-specific medications and response pattern
Descriptive analysis showed that women taking medications had higher participation rates than female non-users, while no such a pattern was seen in men (Table 2). Logistic regression indicated that female non-users and women taking all-cause medications had increased risks of non-response than male non-users. However, the risk of non-response was highest among women with medication use in all three studies (Table 4). Men taking medications had a similar or lower risk of non-response in the MADT (OR=1.02, CI: 0.82, 1.27) and oldest sample (OR=0.85, CI: 0.53, 1.38) and a higher risk in the LSADT (OR=1.18, CI: 0.93, 1.50) than male non-users.
Table 4.
Risk of non-response at intake by total medication use in the Study of Middle-Aged Danish Twins, the Longitudinal Study of Aging Danish Twins and the Danish 1905-Cohort Study
| Surveys | Sample No. (%) | Total, model 1a OR (95% CI) | Total, model 2 OR (95% CI) | Men OR (95% CI) | Women OR (95% CI) |
|---|---|---|---|---|---|
| MADTb | 5203 | ||||
| Non-users | 1 | 1 | 1 | ||
| All-cause users | 3263 (62.7) | 0.89 (0.77, 1.05) | 1.04 (0.83, 1.29) | 0.78 (0.63, 0.98) | |
| Women | 2606 | 1.29 (1.09, 1.52) | |||
| 46–49 | 1 | 1 | 1 | 1 | |
| 50–54 | 0.83 (0.64, 1.07) | 0.83 (0.64, 1.07) | 0.74 (0.52, 1.07) | 0.91 (0.64, 1.31) | |
| 55–59 | 0.95 (0.73, 1.22) | 0.95 (0.74, 1.22) | 0.81 (0.57, 1.16) | 1.09 (0.76, 1.55) | |
| ≥60 | 1.00 (0.79, 1.27) | 1.00 (0.79, 1.27) | 0.88 (0.63, 1.22) | 1.12 (0.81, 1.56) | |
| Male non-users | 1175 (22.6) | 1 | |||
| Male users | 1422 (27.3) | 1.02 (0.82, 1.27) | |||
| Female non-users | 765 (14.7) | 1.51 (1.18, 1.93) | |||
| Female users | 1841 (35.4) | 1.19 (0.97, 1.48) | |||
|
| |||||
| LSADT | 5292c | ||||
| Non-users | 1 | 1 | 1 | ||
| All-cause users | 4294 (81.1) | 1.03 (0.87, 1.20) | 1.18 (0.92, 1.49) | 0.93 (0.75, 1.15) | |
| Women | 3170 (59.9) | 1.36 (1.18, 1.55) | |||
| 70–74 | 1 | 1 | 1 | 1 | |
| 75–79 | 0.64 (0.54, 0.75) | 0.64 (0.55, 0.75) | 0.74 (0.57, 0.96) | 0.58 (0.48, 0.72) | |
| ≥80 | 0.58 (0.49, 0.69) | 0.58 (0.50, 0.69) | 0.66 (0.50, 0.86) | 0.54 (0.44, 0.67) | |
| Male non-users | 483 (9.13) | 1 | |||
| Male users | 1639 (30.9) | 1.18 (0.93, 1.50) | |||
| Female non-users | 515 (9.7) | 1.65 (1.23, 2.22) | |||
| Female users | 2655 (50.2) | 1.52 (1.20, 1.93) | |||
|
| |||||
| c1905 | 3600 | ||||
| Non-users | 1 | 1 | 1 | ||
| All-cause users | 3300 (91.7) | 0.79 (0.63, 1.01) | 0.85 (0.53, 1.37) | 0.78 (0.59, 1.02) | |
| Women | 2751 (76.4) | 1.51 (1.29, 1.77) | |||
| Male non-users | 75 (2.1) | 1 | |||
| Male users | 774 (21.5) | 0.85 (0.53, 1.38) | |||
| Female non-users | 225 (6.3) | 1.65 (0.98, 2.79) | |||
| Female users | 2526 (70.2) | 1.28 (0.81, 2.03) | |||
Model 1 – all-cause medication use, sex, age, Model 2 – Model 1 + all-cause medication use*sex interaction
MADT – the Middle-Age Danish Twins Study, LSADT – the Longitudinal Study of Aging Danish Twins, c1905 – the Danish 1905-Cohort Study, OR – odds ratio; CI – confidence interval
Due to the availability of Prescription Medicine Register since 1995, the analysis of non-response by medication use starts from the LSADT 1997
Similar results were revealed in the analysis of ATC-C medications use (Supplementary Table 3). Compared to the reference group the highest risk of non-response was found among female non-users, followed by women taking ATC-C and other medications, and, finally, by men taking ATC-C and other medications in the older samples. Only in the MADT women taking ATC-C medications were at the highest risk of non-response.
All findings remained unaltered when all-cause and system-specific medication use was evaluated within 2 years prior to the intake and when all-cause medication use of at least 2 or 3 medications within 6 months prior to intake were considered. The results were also unchanged when sex-specific conditions and sex hormones were excluded from all-cause hospitalization and medication use in the MADT sample and when proxy interviews were considered as participants in the LSADT and 1905–Cohort Study (no proxy respondents were in the MADT that included the youngest participants).
Sex differences in the reporting of medication use
The registry data and self-reports showed that women consume more all-cause (Table 5), ATC-M and ATC-N medication medications compared with same-aged men. The use of ATC-C medications was similar in men and women. Sex differences in the mean number of respiratory medications differed by age, such that middle-aged women used more respiratory medicines than the same-aged men, but at older ages men used more respiratory medications.
Table 5.
The number of self-reported and registered medications in the Study of Middle-Aged Danish Twins, the Longitudinal Study of Aging Danish Twins and the Danish 1905-Cohort Study
| Study | No. of persons | Mean No. of registered medications (SE)* | Mean No. of reported medications (SE) | |||
|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | |
| MADTa | ||||||
| Age groups | ||||||
| 46–49 | 397 | 393 | 0.90 (0.07) | 1.69 (0.10) | 0.43 (0.04) | 0.77 (0.06) |
| 50–54 | 514 | 497 | 1.02 (0.07) | 1.99 (0.10) | 0.51 (0.04) | 0.92 (0.06) |
| 55–59 | 506 | 467 | 1.40 (0.08) | 2.33 (0.11) | 0.74 (0.06) | 1.22 (0.07) |
| ≥60 | 769 | 750 | 2.01 (0.09) | 2.69 (0.10) | 1.13 (0.06) | 1.41 (0.06) |
| Total | 2186 | 2107 | 1.44 (0.08) | 2.26 (0.11) | 0.77 (0.05) | 1.13 (0.06) |
|
| ||||||
| LSADT | ||||||
| Age groups | ||||||
| 70–74 | 804 | 901 | 2.92 (0.10) | 3.51 (0.10) | 1.93 (0.07) | 2.17 (0.07) |
| 75–79 | 562 | 894 | 2.88 (0.12) | 3.49 (0.10) | 1.75 (0.08) | 2.08 (0.07) |
| 80–84 | 258 | 442 | 3.26 (0.19) | 3.90 (0.16) | 2.01 (0.13) | 2.46 (0.11) |
| ≥85 | 178 | 344 | 4.20 (0.25) | 3.86 (0.17) | 2.63 (0.17) | 2.45 (0.12) |
| Total | 1802 | 1899 | 3.08 (0.14) | 3.62 (0.12) | 1.96 (0.09) | 2.23 (0.08) |
|
| ||||||
| c1905 | ||||||
| 92–93 | 448 | 1235 | 4.48 (0.15) | 5.16 (0.10) | 2.74 (0.11) | 3.26 (0.07) |
MADT - the Study of Middle-Aged Danish Twins, LSADT – the Longitudinal Study of Aging Danish Twins, c1905- the Danish 1905-Cohort Study, SE – standard error
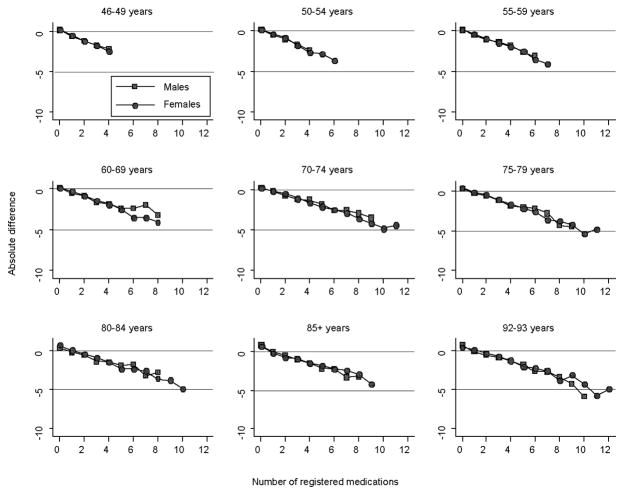
To reveal potential sex differences in reporting pattern we plotted the absolute difference between the sex-age-specific mean number of reported medications and the number of registered medications versus number of registered medications. The Figure 1 shows that both women and men under-reported the number of used medications compared with the register data. It was higher in younger cohorts and increased with increasing number of registered drugs. Under-reporting was the smallest for the ATC-C and largest for the ATC-M medications in the twin samples and the ATC-R medications in the 1905–Cohort Study. However, the degree of under-reporting was similar in both sexes for all-cause and system-specific medication use. Only under-reporting of the ATC-R medications was higher among women.
Figure 1.
Reporting of Medication Use in the Study of Middle-Aged Danish Twins, Longitudinal Study of Aging Danish Twins and Danish 1905–Cohort Study
Discussion
The present study used a combination of survey and national health register data to test whether sex-specific selection and information biases in surveys contribute to the explanations of the health–survival paradox. We found that men had higher participation rates than women at all ages. Further, hospitalized women had higher participation rates than their non-hospitalized counterparts at almost all ages, whereas less consistency was indicated in participation rates among men based on hospitalization status. We also found that women taking all-cause medications had higher participation rates than female non-users, while no such a pattern was observed among men. Likewise, compared with the reference group women with all-cause hospitalization and medication use were at lower risks of non-response than non-hospitalized women or female non-users, respectively. The risk of non-response among men based on hospitalization and medication use had inconsistent pattern across the samples.
These results indicate that women with all-cause hospitalization and women taking prescription medications were slightly overrepresented in surveys. Selective non-participation of healthier women in surveys may result in overestimating health problems among surveyed women and, thus, contribute to the explanation of the health–survival paradox, although its contribution is likely to be small.
The present study revealed higher non-response rates in women that is in agreement with previous research findings in Denmark, Sweden, the Netherlands, and Canada (18–20). Other studies found no or weak evidence for sex differential participation in surveys (21, 22) or even higher participation rates in women compared with men (23, 24). Surveys in Denmark and the Netherlands showed that sex differences in response rates varied by age such that men until 60–65 years had lower participation rates, whereas at older ages women had higher risks of non-participation (25, 26). In a longitudinal survey of elderly in Australia more women refused to participate in the study at the baseline, but no sex difference in participation rates was observed during follow-up surveys (27). In our study, however, women at all ages had lower participation rates than men, which is consistent with other studies (21).
Other studies in Denmark that used register data to investigate selection bias in surveys in terms of healthcare use did not specifically report sex-specific results. In a Danish 1936-cohort study non-respondents had higher mortality and hospitalization rates than participants prior to the survey at age of 60 years (28). Others found that non-respondents had higher hospitalization rates shortly before and throughout data collection, although participants and non-respondents had similar hospital admission rates when healthcare use was measured over a longer period before or after the survey (14, 18, 25). Research in the Dutch population revealed similar utilization of hospital care among participants and non-respondents or even more frequent use of other health services by the participants (20, 29). Possible explanations for such inconsistent results are differences in time periods within which the utilization of health services was measured, age structure of study populations, selected morbidity indicators and data sources (supplementary survey of non-respondents or register).
The present study adds to the previous research evidence that women use medications more frequently than men - especially nervous system medications (30, 31). Our finding of a slightly higher use of respiratory medications in women at younger ages and in men at older ages corresponds with the trends of smoking prevalence in Denmark in 1964–94, when the decline in smoking prevalence was more pronounced in men, whereas the prevalence of heavy smoking remained stable in men and tended to increase in women (32).
The Danish men, contrary to our expectation, tended to underreport medication use similarly to women except that underreporting of the ATC-R medications was higher among women. Our results partially agree with other studies of congruence of self-reports with pharmacy records. Caskie et al. indicated that the proportion of major drugs (e.g. CVD, gastrointestinal, hormones, etc) registered in pharmacy records but omitted from self-reports was similar in women and men, though men had higher levels of agreement for nervous system medications (33). Van den Brandt found that women were more often long-term drug users than men, but no sex differences in the drug recall were indicated (34). Other researchers also failed to find substantial sex differences in the recall of nonsteriod anti-inflammatory or cardiovascular drugs (35, 36).
The current study was well suited for testing the impact of non-response on the health–survival paradox. The data on healthcare utilization were obtained for almost all eligible individuals through linkage of the surveys with registry data rather than through supplementary surveys of non-respondents, which allowed avoiding biased estimates due to the initial pattern of non-response. Second, we used the data from three large nationwide population-based surveys previously conducted in Denmark that included individuals aged 46–102 years and persons living in nursing homes or alternative accommodation. Finally, the present study had a considerable sample size and, consequently, good power to detect the sex differential impact of hospitalization and medication use on response pattern.
The major weakness of this study is that all-cause hospitalization and medication use indicators could be rather crude measures of health. To assure that health was similarly defined in women and men we further considered diagnosis-specific hospitalizations and system-specific medication use that only slightly alter the initial results. Furthermore, to minimize possible errors related to over-the-counter medication we excluded vitamins and alternative medicines from the number of self-reported medications and performed the analysis for several system-specific medications requiring prescription. Besides, all three studies were conducted within approximately the same time period and in a single country and may not be representative for other settings.
In conclusion, the study suggests that selection in surveys may contribute to explaining the health–survival paradox, but its contribution is likely to be small. It also proposed that once in the study men do not underreport medication use compared with women.
Supplementary Material
Acknowledgments
Financial support is provided by the Max Planck Institute for Demographic Research and research grants from the National Institute on Aging (Grant NIA-PO1-AG08761) and the VELUX Foundation.
Abbreviations
- ATC
Anatomical Therapeutic Chemical classification system
- ATC-C
cardiovascular system medications
- ATC-M
musculoskeletal system medications
- ATC-N
nervous system medications
- ATC-R
respiratory system medications
- c1905
Danish 1905–Cohort Study
- CHD
coronary heart disease
- CPR number
Civil Personal Registration Number
- CVD
cardiovascular disease
- ICD
International Classification of Diseases
- LSADT
Longitudinal Study of Aging Danish Twins
- MADT
Study of Middle-Aged Danish Twins
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Olsen KM, Dahl S-A. Health Differences between European Countries. Soc Sci Med. 2007;64:1665–1678. doi: 10.1016/j.socscimed.2006.11.031. [DOI] [PubMed] [Google Scholar]
- 2.Case A, Paxson C. Sex Differences in Morbidity and Mortality. Demography. 2005;42:189–214. doi: 10.1353/dem.2005.0011. [DOI] [PubMed] [Google Scholar]
- 3.Barford A, Dorling D, Smith GD, Shaw M. Life Expectancy: Women Now on Top Everywhere. BMJ. 2006;332:808. doi: 10.1136/bmj.332.7545.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Waldron I, Johnston S. Why Do Women Live Longer Than Men? J Human Stress. 1976;2:19–30. doi: 10.1080/0097840X.1976.9936063. [DOI] [PubMed] [Google Scholar]
- 5.Austad S. Why Women Live Longer Than Men: Sex Differences in Longevity. Gend Med. 2006;3:79–92. doi: 10.1016/s1550-8579(06)80198-1. [DOI] [PubMed] [Google Scholar]
- 6.Christensen K, Kristiansen M, Hagen-Larsen H, Skytthe A, Bathum L, Jeune B, et al. X-Linked Genetic Factors Regulate Hematopoietic Stem-Cell Kinetics in Females. Blood. 2000;95:2449–2451. [PubMed] [Google Scholar]
- 7.Owens IPF. Ecology and Evolution: Sex Differences in Mortality Rate. Science. 2002;297:2008–2009. doi: 10.1126/science.1076813. [DOI] [PubMed] [Google Scholar]
- 8.Nathanson CA. Illness and the Feminine Role: A Theoretical Review. Soc Sci Med. 1975;9:57–62. doi: 10.1016/0037-7856(75)90094-3. [DOI] [PubMed] [Google Scholar]
- 9.Galdas PM, Cheater F, Marshall P. Men and Health Help-Seeking Behaviour: Literature Review. J Adv Nurs. 2005;49:616–623. doi: 10.1111/j.1365-2648.2004.03331.x. [DOI] [PubMed] [Google Scholar]
- 10.Verbrugge LM, Wingard DL. Sex Differentials in Health and Mortality. Women Health. 1987;12:103–145. doi: 10.1300/J013v12n02_07. [DOI] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL. Gender Differences in the Reporting of Physical and Somatoform Symptoms. Psychosom Med. 1998;60:150–155. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Wingard DL, Cohn BA, Kaplan GA, Cirillo PM, Cohen RD. Sex Differentials in Morbidity and Mortality Risk Examined by Age and Cause in the Same Cohort. Am J Epidemiol. 1989;130:601–610. doi: 10.1093/oxfordjournals.aje.a115374. [DOI] [PubMed] [Google Scholar]
- 13.Gaist D, Bathum L, Skytthe A, Jensen TK, McGue M, Vaupel JW, et al. Strength and Anthropometric Measures in Identical and Fraternal Twins: No Evidence of Masculinization of Females with Male Co-Twins. Epidemiology. 2000;11:340–343. doi: 10.1097/00001648-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Christensen K, Holm NV, McGue M, Corder L, Vaupel JW. A Danish Population-Based Twin Study on General Health in the Elderly. J Aging Health. 1999;11:49–64. doi: 10.1177/089826439901100103. [DOI] [PubMed] [Google Scholar]
- 15.Nybo H, Gaist D, Jeune B, Bathum L, McGue M, Vaupel JW, et al. The Danish 1905 Cohort: A Genetic-Epidemiological Nationwide Survey. J Aging Health. 2001;13:32–46. doi: 10.1177/089826430101300102. [DOI] [PubMed] [Google Scholar]
- 16.Christensen K, Frederiksen H, Vaupel JW, McGue M. Age Trajectories of Genetic Variance in Physical Functioning: A Longitudinal Study of Danish Twins Aged 70 Years and Older. Behav Genet. 2003;33:125–136. doi: 10.1023/a:1022501817781. [DOI] [PubMed] [Google Scholar]
- 17.Støvring H. Selection Bias Due to Immigration in Pharmacoepidemiologic Studies. Pharmacoepidemiology and Drug Safety. 2007;16:681–686. doi: 10.1002/pds.1419. [DOI] [PubMed] [Google Scholar]
- 18.Osler M, Schroll M. Differences between Participants and Non-Participants in a Population Study on Nutrition and Health in the Elderly. Eur J Clin Nutr. 1992;46:289–295. [PubMed] [Google Scholar]
- 19.von Strauss E, Fratiglioni L, Jorm AF, Viitanen M, Winblad B. Attitudes and Participation of the Elderly in Population Surveys: Data from a Longitudinal Study on Aging and Dementia in Stockholm. J Clin Epidemiol. 1998;51:181–187. doi: 10.1016/s0895-4356(97)00242-4. [DOI] [PubMed] [Google Scholar]
- 20.Boshuizen HC, Viet AL, Picavet HSJ, Botterweck A, van Loon AJM. Non-Response in a Survey of Cardiovascular Risk Factors in the Dutch Population: Determinants and Resulting Biases. Public Health. 2006;120:297–308. doi: 10.1016/j.puhe.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Zunzunegui MV, Beland F, Gutierrez-Cuadra P. Loss to Follow-up in a Longitudinal Study on Aging in Spain. J Clin Epidemiol. 2001;54:501–510. doi: 10.1016/s0895-4356(00)00325-5. [DOI] [PubMed] [Google Scholar]
- 22.Launer LJ, Wind AW, Deeg DJH. Nonresponse Pattern and Bias in a Community-Based Cross-Sectional Study of Cognitive Functioning among the Elderly. Am J Epidemiol. 1994;139:803–812. doi: 10.1093/oxfordjournals.aje.a117077. [DOI] [PubMed] [Google Scholar]
- 23.Korkeila K, Suominen S, Ahvenainen J, Ojanlatva A, Rautava P, Helenius H, et al. Non-Response and Related Factors in a Nation-Wide Health Survey. Eur J Epidemiol. 2001;17:991–999. doi: 10.1023/a:1020016922473. [DOI] [PubMed] [Google Scholar]
- 24.van den Akker M, Buntinx F, Metsemakers JF, Knottnerus JA. Morbidity in Responders and Non-Responders in a Register-Based Population Survey. Fam Pract. 1998;15:261–263. doi: 10.1093/fampra/15.3.261. [DOI] [PubMed] [Google Scholar]
- 25.Kjoller M, Thoning H. Characteristics of Non-Response in the Danish Health Interview Surveys, 1987–1994. Eur J Public Health. 2005;15:528–535. doi: 10.1093/eurpub/cki023. [DOI] [PubMed] [Google Scholar]
- 26.Lamers LM. Medical Consumption of Respondents and Non-Respondents to a Mailed Health Survey. Eur J Public Health. 1997;7:267–271. [Google Scholar]
- 27.Jacomb P, Jorm A, Korten A, Christensen H, Henderson AS. Predictors of Refusal to Participate: A Longitudinal Health Survey of the Elderly in Australia. BMC Public Health. 2002;2:4. doi: 10.1186/1471-2458-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Drivsholm T, Eplov LF, Davidsen M, Jorgensen T, Ibsen H, Hollnagel H, et al. Representativeness in Population-Based Studies: A Detailed Description of Non-Response in a Danish Cohort Study. Scand J Public Health. 2006;34:623–631. doi: 10.1080/14034940600607616. [DOI] [PubMed] [Google Scholar]
- 29.Reijneveld SA, Stronks K. The Impact of Response Bias on Estimates of Health Care Utilization in a Metropolitan Area: The Use of Administrative Data. Int J Epidemiol. 1999;28:1134–1140. doi: 10.1093/ije/28.6.1134. [DOI] [PubMed] [Google Scholar]
- 30.Barat I, Andreasen F, Damsgaard EM. The Consumption of Drugs by 75-Year-Old Individuals Living in Their Own Homes. Eur J Clin Pharmacol. 2000;56:501–509. doi: 10.1007/s002280000157. [DOI] [PubMed] [Google Scholar]
- 31.Roe CM, McNamara AM, Motheral BR. Gender- and Age-Related Prescription Drug Use Patterns. Ann Pharmacother. 2002;36:30–39. doi: 10.1345/aph.1A113. [DOI] [PubMed] [Google Scholar]
- 32.Osler M, Prescott E, Gottschau A, Bjerg A, Hein HO, Sjol A, et al. Trends in Smoking Prevalence in Danish Adults, 1964–1994. The Influence of Gender, Age, and Education. Scand J Soc Med. 1998;26:293–298. doi: 10.1177/14034948980260041101. [DOI] [PubMed] [Google Scholar]
- 33.Caskie GIL, Willis SL. Congruence of Self-Reported Medications with Pharmacy Prescription Records in Low-Income Older Adults. Gerontologist. 2004;44:176–185. doi: 10.1093/geront/44.2.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van den Brandt PA, Petri H, Dorant E, Goldbohm RA, Van de Crommert S. Comparison of Questionnaire Information and Pharmacy Data on Drug Use. Pharm Weekbl Sci. 1991;13:91–96. doi: 10.1007/BF01974987. [DOI] [PubMed] [Google Scholar]
- 35.West SL, Savitz DA, Koch G, Strom BL, Guess HA, Hartzema A. Recall Accuracy for Prescription Medications: Self-Report Compared with Database Information. Am J Epidemiol. 1995;142:1103–1112. doi: 10.1093/oxfordjournals.aje.a117563. [DOI] [PubMed] [Google Scholar]
- 36.Sjahid SI, van der Linden PD, Stricker BHC. Agreement between the Pharmacy Medication History and Patient Interview for Cardiovascular Drugs: The Rotterdam Elderly Study. Br J Clin Pharmacol. 1998;45:591–595. doi: 10.1046/j.1365-2125.1998.00716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.