Abstract
Oropharyngeal candidiasis (OPC) is an opportunistic infection caused by Candida albicans. Despite its prevalence, little is known about C. albicans-specific immunity in the oral mucosa. Vaccines against Candida generate both Th1 and Th17 responses, and considerable evidence implicates IL-17 in immunity to OPC. However, IL-17 is also produced by innate immune cells that are remarkably similar to Th17 cells, expressing the same markers and localizing to similar mucosal sites. To date, the relative contribution(s) of Th1, Th17 and innate IL-17-producing cells in OPC have not been clearly defined. Here, we sought to determine the nature and function of adaptive T cell responses to OPC, using a new recall infection model. Mice subjected to infection and re-challenge with Candida mounted a robust and stable antigen specific IL-17 response in CD4+ but not CD8+ T cells. There was little evidence for Th1 or Th1/Th17 responses. The Th17 response promoted accelerated fungal clearance, and Th17 cells could confer protection in Rag1−/− mice upon adoptive transfer. Surprisingly, CD4 deficiency did not cause OPC, but was instead associated with compensatory IL-17 production by Tc17 and CD4-CD8-CD3+ cells. Therefore, classic CD4+Th17 cells protect from OPC, but can be compensated by other IL-17-producing cells in CD4-deficient hosts.
Keywords: Candida albicans, IL-17, Th17, adaptive immunity, oral mucosal immunity
Introduction
Candida albicans is a dimorphic fungus frequently found in the oral cavity that is nonpathogenic in healthy individuals. Immunocompromised patients frequently suffer from oropharyngeal candidiasis (OPC, “thrush”), characterized by painful pseudomembranous lesions in the tongue, pharynx and buccal mucosa (1). Most HIV+ patients develop oral thrush at least once, which is prognostic for poor outcome (2). Because loss of CD4+ T lymphocytes is a hallmark of AIDS, CD4+ T cells are considered key for defense against OPC. However, relatively little is known about T cell responses in the oral mucosa, and the specific T cell subset that mediates resistance to OPC has been an ongoing topic of debate.
Originally described in 1986, Th1 and Th2 cells secrete IFNγ and IL-4 and are induced to differentiate by IL-12 and IL-4, respectively. Th17 cells were identified in 2005, and produce IL-17 (IL-17A), IL-17F and IL-22 as signature cytokines (3, 4). Early studies of OPC suggested that Th1 cells were key mediators of immunity, because mice deficient in the p40 subunit of IL-12 were susceptible. However, mice lacking IFNγ were resistant to infection (5). The basis for this paradox became clear with the recognition that IL-12 shares its p40 subunit with IL-23, which promotes Th17 maintenance and proliferation (4). In experiments designed to address this issue, we found that IL-23−/−, IL-17RA−/− and IL-17RC−/− mice are susceptible to OPC, whereas mice lacking the IL-12p35 subunit are resistant, strongly supporting a role for Th17 and not Th1 cells (6, 7). However, experimental vaccines against Candida and other fungal infections such as Blastomyces generate both Th17 and Th1 responses (8–10), and Th17 cells and IL-17 have been implicated in immune pathology in gastric candidiasis (11). Thus, the relative importance of adaptive Th17 cells in immunity to mucosal candidiasis has not been entirely resolved (8, 9).
In humans, Candida-responsive CD4+ T cells express Th17 markers such as IL-17, RORγt, CCR6 and CCR4, while they sometimes co-express IFNγ, they do not express Th1-associated markers (12, 13). Recurrent OPC, which is one manifestation of chronic mucocutaneous candidiasis (CMC), is characteristic of several immunodeficiency syndromes, which collectively implicate Th17 cells in immunity to Candida (14). In AIDS, Th17 cells are preferentially depleted, and OPC incidence tracks with CD4 loss (15). Hyper-IgE (HIES)/Job’s Syndrome patients have mutations in STAT3 and concomitantly reduced Th17 frequency, and characteristically experience recurrent OPC (16–20). In addition, CMC can be caused by gain-of-function mutations in STAT1 that result in heightened cellular responses to IFNα/β, IFNγ and IL-27, all inhibitors of Th17 development (21, 22). At the level of pattern recognition, mutations in the fungal pattern recognition receptor dectin-1 or its adaptor CARD9 are linked to impaired Th17 generation and CMC (23, 24). Autoimmune polyendocrinopathy syndrome (APS-1) is also characterized by CMC, and is linked to neutralizing autoantibodies against Th17 cytokines (25–27). Mutations in IL-17RA and IL-17F in humans cause CMC, independently of other cofactors (28). Together, these data support an essential role for Th17 cells in immunity to Candida in mucosal tissues.
In this study, we sought to define the nature and contribution of adaptive Th responses to oral candidiasis using a newly established recall model of OPC. We show that strong, Candida-dependent recall responses are generated in the CD4+ but not CD8+ T cell compartment. There is no evidence for generation of a Th1 or IFNγ response. Importantly, development of Th17 cells in recall infection settings promotes accelerated fungal clearance, and transfer of CD4+ T cells into susceptible Rag1−/− hosts is sufficient to protect from disease. However, deficiency of CD4+ T cells leads to compensatory IL-17 production by CD8+ and CD3+CD4-CD8- (double negative, DN) cells and concomitant protection from OPC.
Results
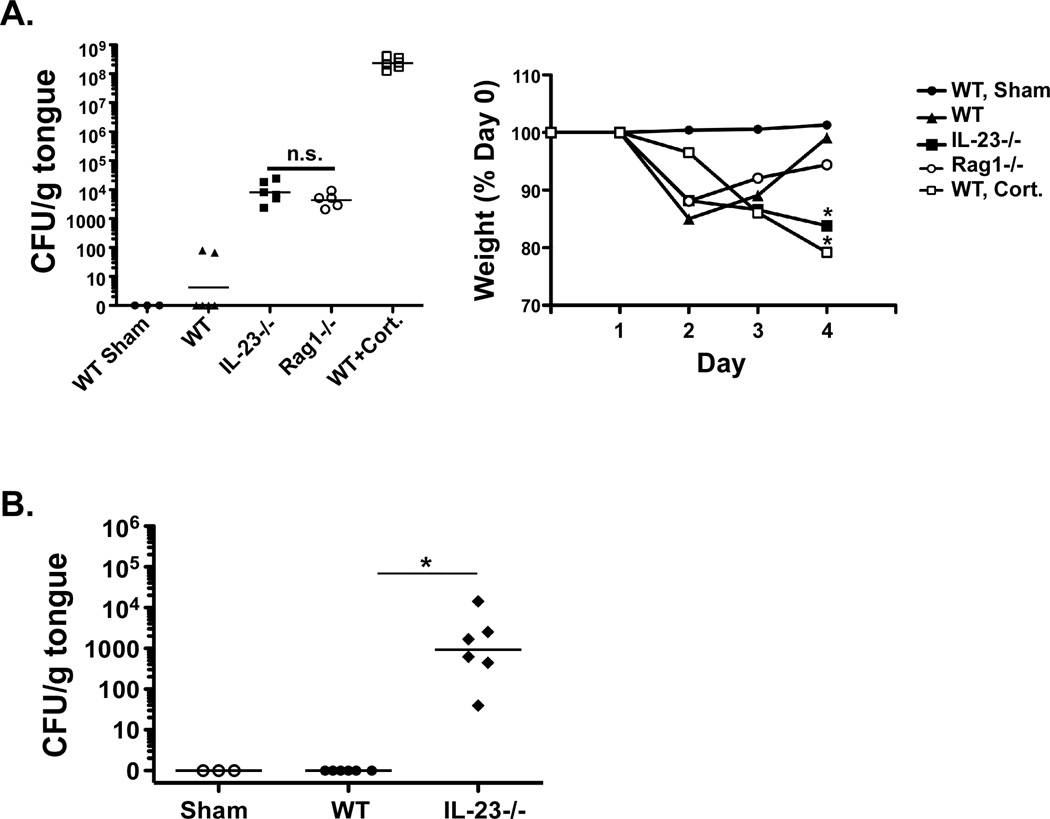
Pre-exposure to Candida albicans promotes accelerated fungal clearance
To address the role of the adaptive response in OPC, we first evaluated susceptibility in Rag1−/− mice. WT (C57BL/6) or Rag1−/− mice were subjected to a 4-day sublingual infection with 2×107 CFU C. albicans (6, 29). As controls, IL-23−/− or WT mice immunosuppressed with cortisone acetate were subjected to OPC. As reported previously, unmanipulated WT mice generally cleared the fungus by the end of the infection period, whereas IL-23−/− and cortisone-treated WT mice had high oral loads of Candida and concomitant weight loss (Fig 1A). Moreover, IL-23−/− mice failed to clear the infection for at least 3 weeks (Fig 1B). Rag1−/− mice exhibited fungal loads ~3 logs higher than WT, which were statistically indistinguishable from IL-23−/− mice, though the Rag1−/− mice did regain some weight towards the end of the experiment (Fig 1A). These results indicate that a rearranged antigen receptor is necessary for immunity to OPC, and further indicate that innate lymphoid-like cells (ILCs) such as those reported in certain forms of colitis do not appear to mediate immunity in this setting (30, 31).
Figure 1. Rag1−/− mice are susceptible to OPC.
WT, IL-23−/− or Rag1−/− mice were subjected to sublingual infection with C. albicans, and fungal load in tongue was assessed by plating onto YPD and colony enumeration in triplicate. Sham mice were inoculated with PBS only. Cortisone treated mice were given 225 mg/kg cortisone acetate at days −1, +1 and 3 relative to infection. CFU/g tongue tissue is indicated with geometric mean (bar). Weight loss (average per cohort) during infection is shown as a percentage of starting weight at day 0. Data represent 2 independent experiments. *p<0.05 compared to WT mice infected with Candida. B. IL-23−/− mice remain persistently infected with C. albicans. The indicated mice were subjected to 1° infection. 21 days later, fungal load in tongue was assessed by plating on YPD and colony enumeration in triplicate. *p<0.05 compared to WT.
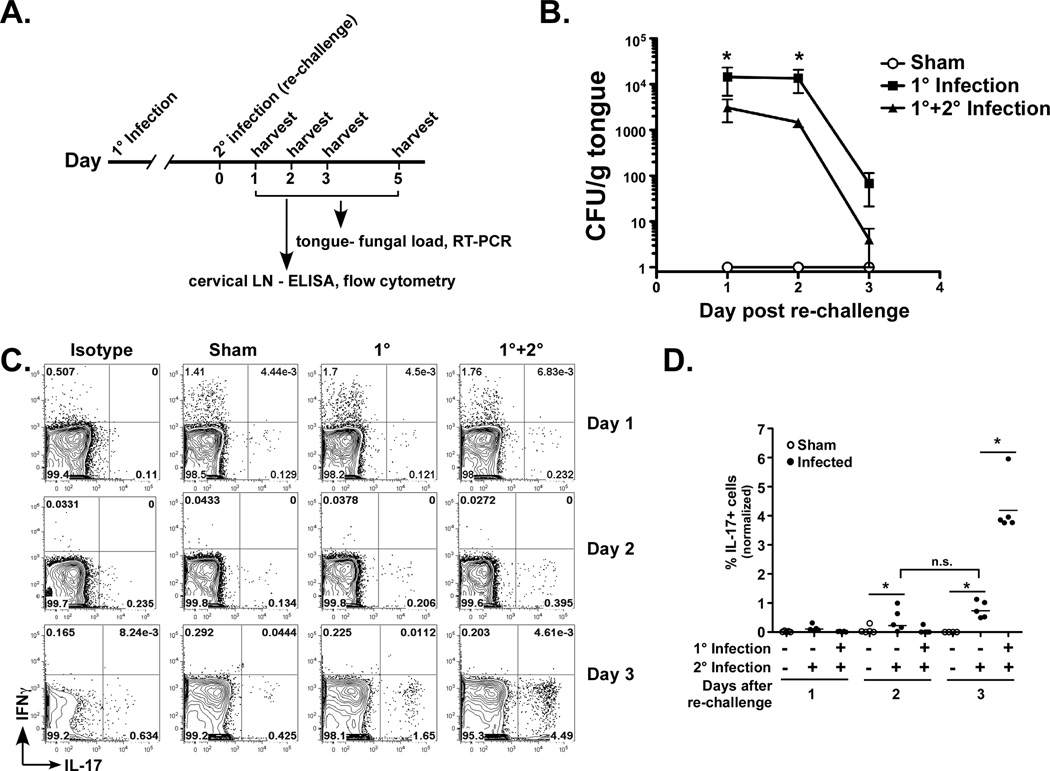
Taking advantage of the fact that C. albicans is not a commensal microbe in mice, we developed a system that permits experimental separation of the effects of innate and adaptive responses (Fig 2A). WT mice were inoculated orally by means of a Candida-soaked cotton ball placed sublingually for 75 minutes. 6–8 weeks after primary exposure, mice were re-challenged orally with Candida. As controls, mice were sham-inoculated with PBS at one or both time points. On days 1, 2 and 3 following re-challenge, tongue was harvested to analyze fungal burden and cervical lymph nodes (cLN) were analyzed for cytokine production. Mice pre-exposed to C. albicans (1° + 2° infection) had significantly lower fungal burdens (~1 log) after secondary challenge than those receiving only a 1° acute infection (Fig 2B). By day 3, most mice had cleared the infection, though residual fungal CFUs were still higher in mice receiving only a primary compared to secondary challenge. Therefore, prior exposure to Candida induces more efficient pathogen clearance.
Figure 2. Adaptive Candida albicans-responsive Th17 cells accelerate fungal clearance.
A. New re-challenge OPC infection model. Diagram of infection timeline. B. Re-challenge is associated with accelerated Candida clearance. WT mice were subjected to a 1° infection with Candida or PBS (Sham). After 6 weeks, mice were re-challenged with Candida (1° + 2° infection) or PBS. Mice were sacrificed at days 1, 2 and 3 post re-challenge, and fungal load in tongue was assessed by plating and colony enumeration in triplicate. Data are pooled from 2 replicate experiments. C. CD4+ Th17 but not Th1 cells are generated upon Candida re-challenge. cLN cells from the experiment described in B were isolated 1–3 days after re-challenge and stained for CD4, IL-17 and IFNγ. Lymphocytes (determined by forward and side scatter profiles) were gated on CD4+, and IL-17+ and IFNγ+ cell frequencies are depicted. Representative FACS plots are shown. D. Summary of data from panel C. Note that data are normalized to ICS staining from isotype controls. E–F. IL-17+ cells exhibit an activated phenotype. cLN cells were isolated 3 days after 1° or re-challenge and gated on CD3 and CD4. Surface expression of CD44 and CD27 was examined relative to intracellular IL-17. Data from mice subjected to recall are summarized in panel F. * p<0.05 G. CD4+ T cells are sufficient to confer immunity to OPC in Rag1−/− mice. WT mice were subjected to Sham or re-challenge (1°+2°). On day 3 after re-challenge, CD4+ and CD4- cells were harvested from cLN by magnetic sorting. 1 × 107 CD4+ or 2×107 CD4- cells were transferred into Rag1−/− recipients. After 24 h, Rag1−/− mice were infected with Candida, and weight loss monitored for 5 d (right). Fungal load in tongue was assessed at day 5 (left). * p<0.05 by t-test with Mann-Whitney correction or ANOVA; n.s., not significant. H. IL-17 but not IFNγ is expressed locally upon transfer with re-challenged CD4+ cells. Rag1−/− mice were adoptively transferred with (or without) CD4+ cells from WT mice given a Sham infection or a recall (1° + 2°) infection. Expression of il17a and ifng mRNA in tongue were assessed in by qPCR. Note that these samples are from a different experiment than shown in panel G. * p<0.05 by t-test with Mann-Whitney correction.
To evaluate the nature of the T cell compartment in Candida recall responses, draining cervical LN (cLN) cells were stained for CD4, IL-17 and IFNγ (Fig 2C–D). There were no CD4+IL-17+ cells in Sham-treated cLN. However, there was an increased frequency of CD4+IL-17+ cells in cLN of infected mice, comprising approximately 4% by day 3 post re-challenge. There was no detectable induction of CD4+IFNγ+ cells upon Candida infection, either during a first exposure or re-challenge, nor were there IFNγ+IL-17+ double-expressors evident in either setting. There was a small increase in CD4+IL-17+ cells in mice undergoing only a primary response. To evaluate the surface phenotype of the CD4+IL-17+ cells, total cLN cells isolated 3 days after re-challenge were gated on CD4, and surface expression of CD44 and CD27 were examined relative to intracellular IL-17. CD4+IL-17+ cells were primarily CD27-CD44+ (Fig 2E–F), consistent with an activated effector phenotype.
To determine whether Th17 cells have the capacity to protect from OPC, CD4+ or CD4- cells were isolated from cLNs of mice subjected to a recall response and transferred into susceptible Rag1−/− hosts (Supplementary Fig S1). After 24 h, mice were subjected to OPC. Mice receiving CD4+ but not CD4- cells showed complete protection from OPC (Fig 2G). Notably, il17a mRNA expression in tongue correlated with protection, indicative of a local Th17 response (Fig 2H). In contrast, there was no detectable ifng mRNA expression in the tongue following transfer of CD4+ cells (Fig 2H). These data suggest that Th17 cells comprise the dominant functional CD4 response upon Candida re-challenge.
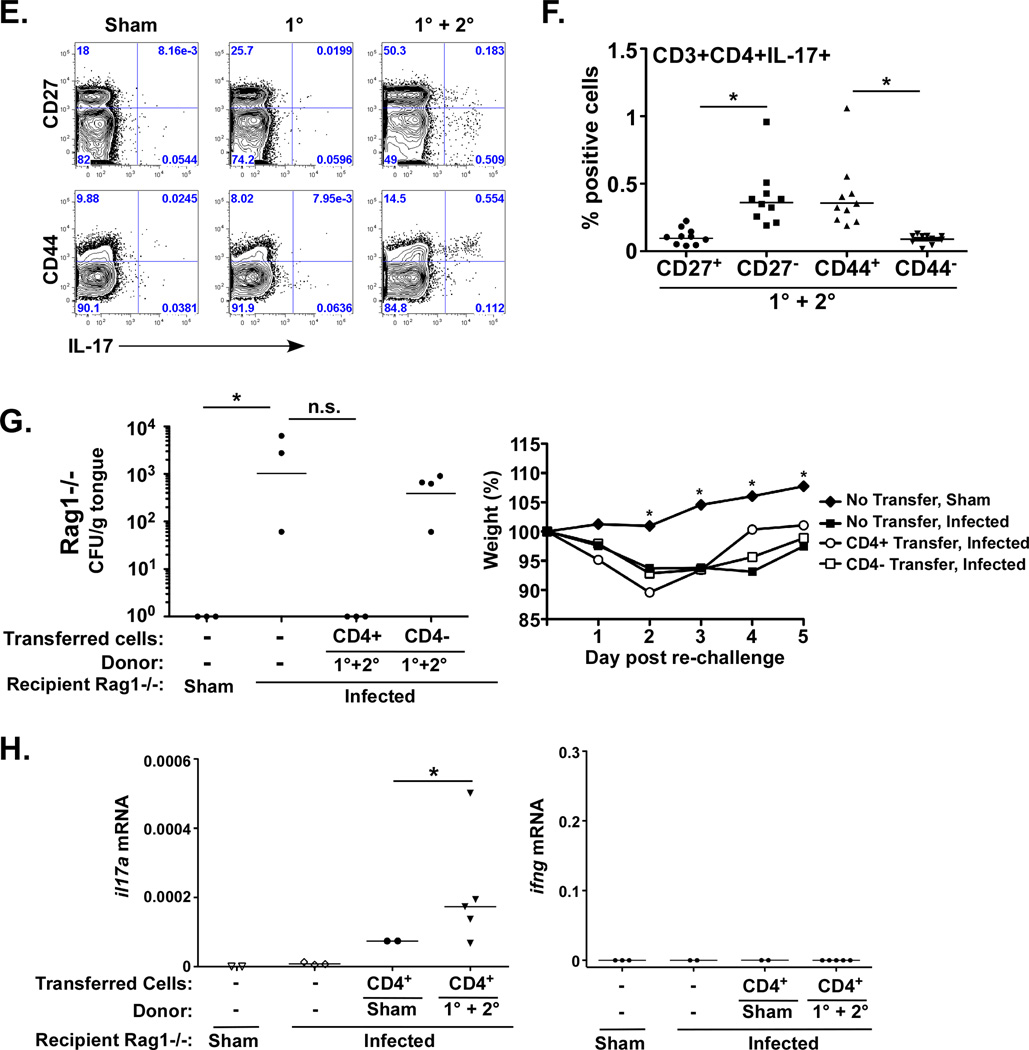
The IL-17 recall response to OPC comes from the CD4+ not the CD8+ compartment
To evaluate the nature of the T cell response in more detail, cells isolated from cLN 3 days post re-challenge were stained for CD3, CD4 and CD8, followed by intracellular staining for IL-17 and IFNγ (Fig 3A–B). As shown, only mice subjected to re-challenge generated significant numbers of IL-17+ cells in the CD4+ compartment (Fig 3B, left). There was no increase in the frequency of CD8+ IL-17+ cells (Fig 3B, left). Additionally, there was no change in the number of CD4+IFNγ+ cells (Fig 3B, right). There was a small increase in IFNγ+ cells in the CD8+ compartment, (Fig 3B, right), but this was transient and not sustained at 5 days post-infection (Supplementary Fig S2A). There was a low baseline level of IL-17+ cells in the CD3-negative population, which did not change after infection (Supplementary Fig S2B).
Figure 3. IL-17 is produced by CD4+ but not CD8+ T cells in cervical LN upon re-challenge with Candida.
A–B. CD4 but not CD8 IL-17+ T cells are induced following re-challenge. WT mice were subjected to the re-challenge model in Fig 2A. On day 3 post re-challenge, cLN cells were gated on CD3+ lymphocytes and CD4+ or CD8+ populations, and IL-17+ and IFNγ+ cell frequencies were assessed by ICS. Representative plots are shown. B. Summary of data from panel A, indicating percentages of IL-17+ (left) or IFNγ+ (right) cells from CD4+ and CD8+ compartments. Data are normalized to isotype control staining and are representative of 2 experiments. C–D. IL-17 and IFNγ levels in cLN cells following Candida re-challenge. Cells from cLN were isolated 3 d post re-challenge from the indicated mice and were then cultured in vitro for 4–5 d ± heat-killed C. albicans (HK Ca) (left and middle panels) or the ALS1/3 peptide (right) in the presence or absence of anti-CD4 neutralizing Abs (left) or anti-MHC Class II Abs (middle and right) (32). IL-17A or IFNγ was assessed by ELISA. * p<0.05 by Mann-Whitney t-test.
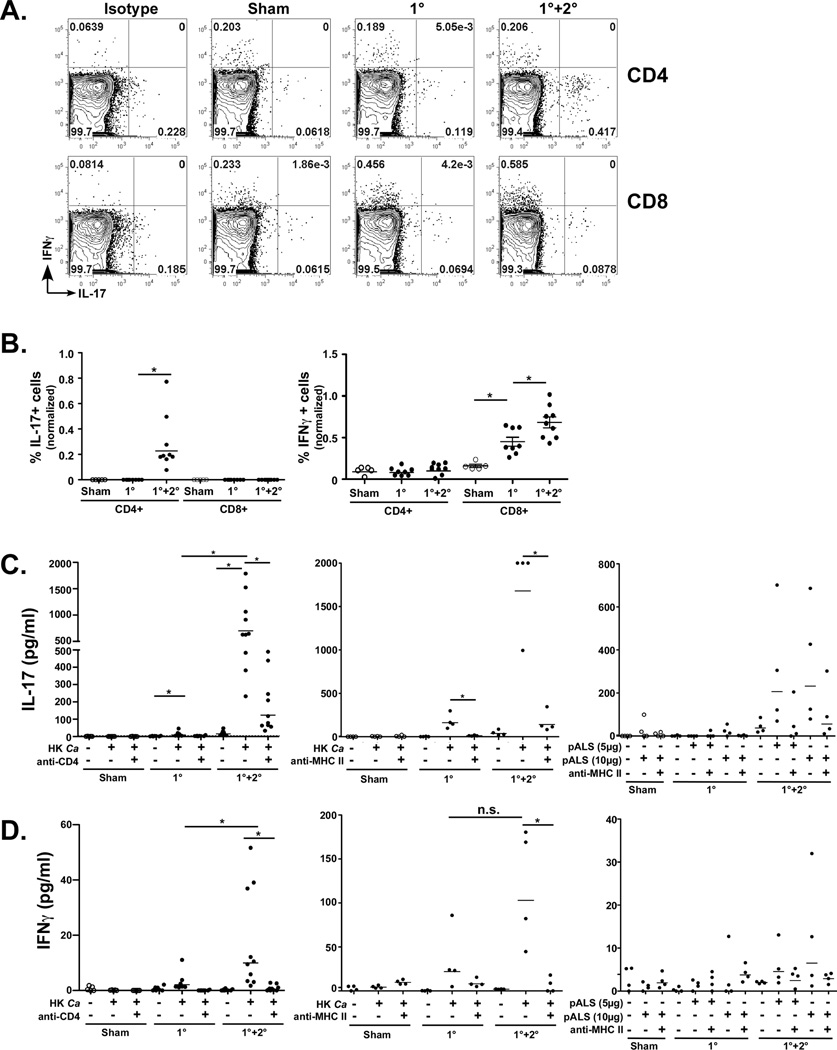
The CD4+ IL-17 recall response to OPC is antigen-specific
To confirm that induction of cytokines is Candida-specific, cLN cells were harvested 3 days after re-challenge and stimulated in vitro with heat killed (HK) C. albicans for 5 days in vitro. Supernatants were evaluated for IL-17 and IFNγ by ELISA. Consistent with the intracellular cytokine staining (ICS) data (Fig 3A–B), high levels of IL-17 (~500 pg/ml) were produced in mice exposed to Candida during a secondary response, but not in Sham-infected mice and only modestly in 1° infected mice (Fig 3C, left). Production of IL-17 was blocked by anti-CD4 (32) and anti-MHC Class II Abs, indicating that antigen presentation is required. To further verify that IL-17 production is antigen-specific, LN cells from infected mice were cultured in vitro with a peptide derived from the Candida adhesins Als1 and Als3, recently shown to be an epitope recognized by CD4+T cells (33). Treatment with the ALs1/3 peptide (pALS) triggered IL-17 production, though not to the same magnitude as HK Candida, and was blocked by anti-MHC Class II Abs (Fig 3C). Therefore, the Th17 response is antigen-specific.
Unexpectedly. there was a modest but reproducible CD4-dependent induction of IFNγ following treatment with HK Candida in re-challenged mice, ranging from ~15–100 pg/ml, depending on experiment, Fig 3D. The induction of IFNγ-producing cells was slightly increased in re-challenged mice compared to mice receiving only a primary infection, and was blocked with anti-CD4 or anti-MHC II Abs. However, there was no detectable IFNγ production after in vitro challenge with pALS. Although inducible IFNγ following in vitro challenge contrasts with the apparent lack of a Th1 response in cells taken immediately ex vivo measured by flow cytometry, it is most likely that Th1 cells are induced during infection, but at levels below the detection limit of FACS. Together, these data indicate that the response to oral Candida infection is primarily IL-17-driven, though we cannot entirely rule out a role for IFNγ. Moreover, generation of a strong CD4+Th17 recall response promotes accelerated oral clearance of C. albicans.
Compensatory sources of IL-17 in CD4-deficient mice
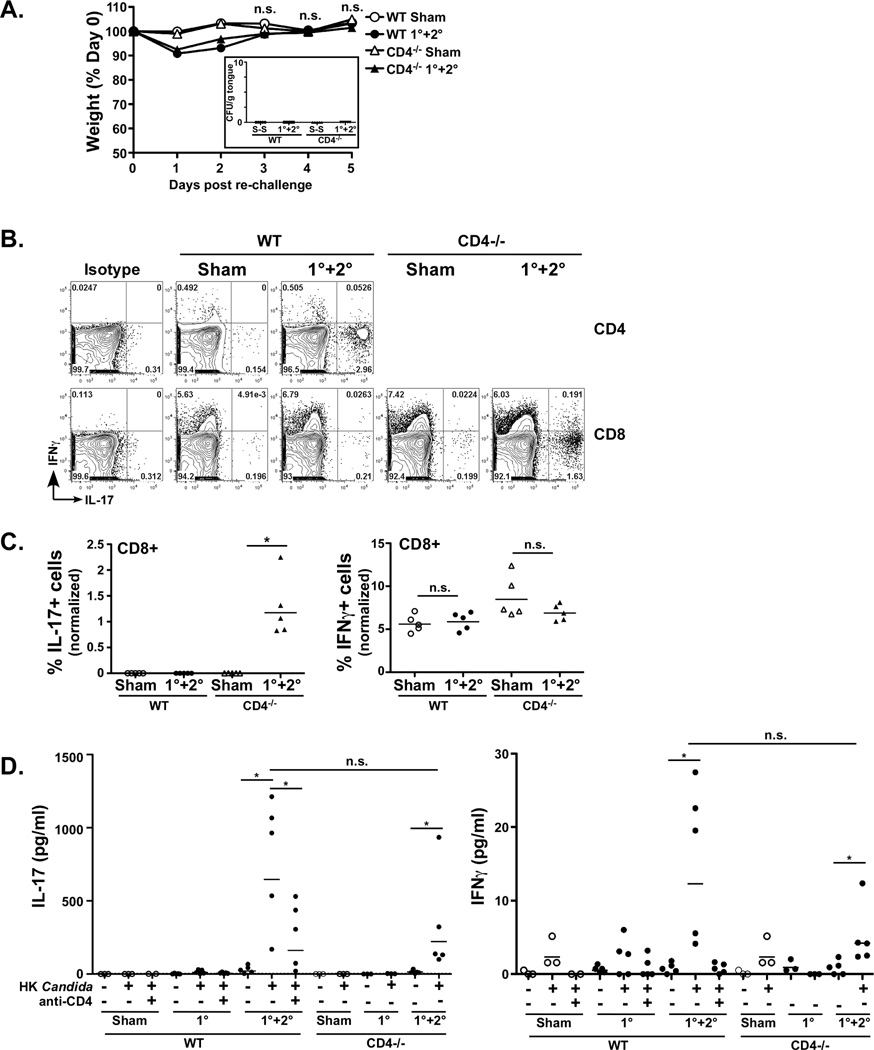
To determine whether generation of CD4+Th17 cells is necessary for clearance of Candida from the oral cavity, WT or CD4−/− mice were subjected to re-challenge and evaluated for symptoms of OPC, including weight loss and oral fungal burden. CD4−/− mice were resistant to OPC, as they regained weight equivalently to WT mice after infection (Fig 4A) and had no detectable oral fungal burden (Fig 4A, inset). To evaluate the possibility that IL-17 might be produced from a compensatory source in CD4-deficient mice, cLN cells from WT and CD4−/− mice were analyzed for cytokines 5 days after re-challenge. In WT mice, CD4+ but not CD8+ T cells expressed IL-17 during re-challenge (Fig 4B). However, in re-challenged CD4−/− mice, CD8+ T cells produced abundant IL-17 (Fig 4B–C). The frequency of IFNγ-expressing CD8+ cells was similar in WT and CD4−/− mice (Fig 4C, right), further confirming that IFNγ responses do not seem to play a role in protection. Although somewhat variable, levels of IL-17 from the CD8-compartment in CD4−/− mice were usually comparable to that of the CD4 compartment in WT mice (Fig 4D left, and data not shown). IL-17 secretion from in vitro-stimulated cLN cells was observed only during 2° challenge (Fig 4D, left). There was a weak but significant increase in the IFNγ response as well (Fig 4D, right). There was a low frequency of IL-17-producing cells in the CD3-negative population in both WT and CD4−/− mice, which did not change following infection (Supplementary Fig S2).
Figure 4. CD4-deficient mice are resistant to re-challenge with Candida, associated with compensatory IL-17 from CD8+ T cells.
A. CD4−/− mice are resistant to OPC. WT or CD4−/− mice were subjected to the OPC re-challenge model. Daily weight measurements post re-challenge are indicated as a percentage of starting weight. N.s., not significant by ANOVA. Inset: Fungal burden on day 5 after re-challenge is indicated. B–C. CD4−/− but not WT mice induce IL-17+CD8+ T cells upon re-challenge. WT or CD4−/− mice were subjected to the re-challenge model. On day 5 post re-challenge, cLN cells were gated on CD3+ lymphocytes and CD4+ or CD8+ populations, and IL-17+ and IFNγ+ cell frequencies are depicted in CD4+ (WT only) or CD8+ cells. Representative plots are shown. B. Summary of flow cytometry data from panel A, indicating percentages of IL-17+ (left) or IFNγ+ (right) cells from CD4+ and CD8+ compartments. Data are normalized to isotype controls and are representative of 2 independent experiments. D. CD4−/− and WT mice produce IL-17 upon re-challenge. Cells from cLN were isolated 3 d post re-challenge and cultured in vitro for 5 d ± heat-killed (HK) Candida albicans ± anti-CD4 neutralizing Abs. Concentrations of IL-17A or IFNγ were assessed by ELISA.
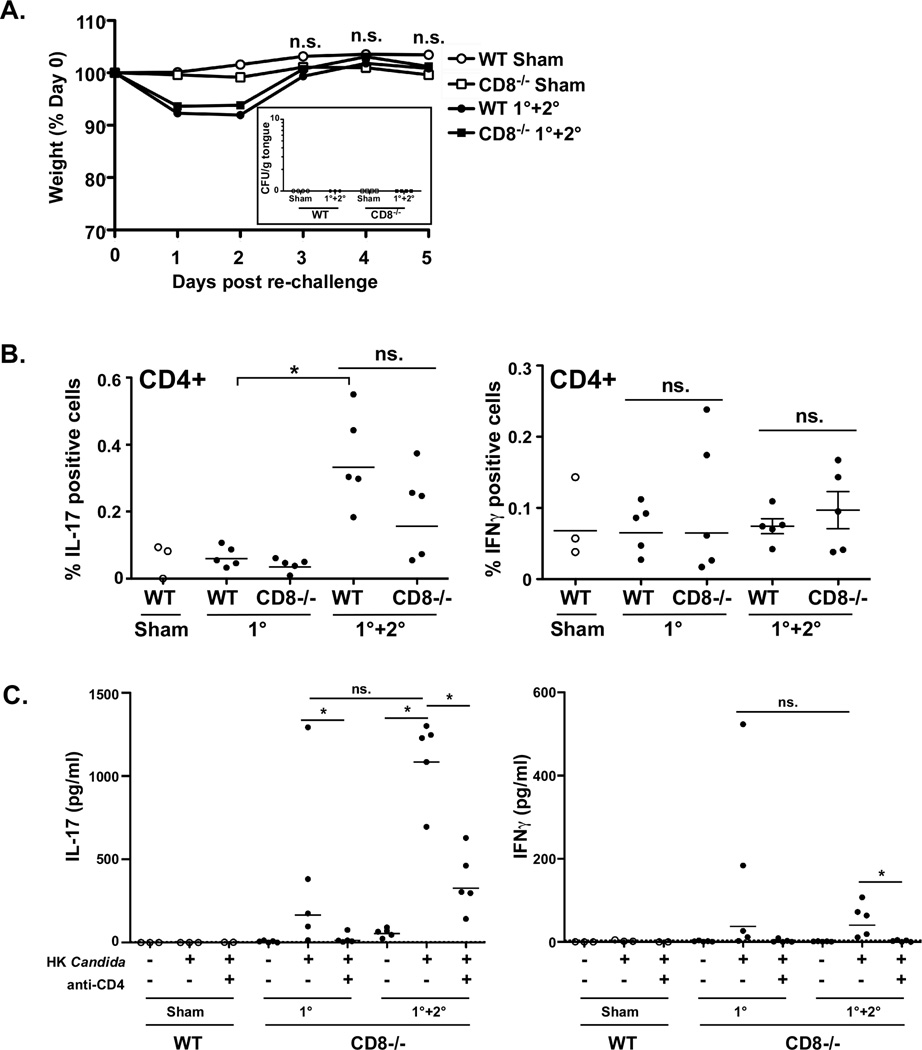
Since the resistance of CD4−/− mice to C. albicans re-challenge correlates with compensatory IL-17 production by CD8+ T cells, we tested the susceptibility of CD8−/− mice to OPC. Like CD4−/− mice, CD8−/− mice were resistant to OPC upon re-challenge, based on weight gain after infection and the complete absence of an oral fungal load (Fig 5A). Consistently, equivalent numbers of CD4+IL-17+ cells were present in cLN of CD8−/− and WT mice subjected to re-challenge but not in cLN of mice that only received a 1° infection, whereas CD4+IFNγ+ cell frequencies were unchanged (Fig 5B). High levels of IL-17 were induced after in vitro culture with HK Candida (Fig 5C), which was blocked with anti-CD4 Abs (Fig 5C, left). Although the difference between IL-17 levels in the 1° and 1°+2° in vitro cultures did not reach statistical significance, this was likely due to a single outlier in the 1° sample, and the overall trend strongly resembled what was observed in the CD4 compartment in WT mice. There was induction of a weak IFNγ response in CD8−/− mice during both 1° and 2° responses (Fig 5C, right).
Figure 5. CD8−/− mice respond to Candida similarly to WT.
A. CD8−/− mice are resistant to OPC. WT or CD8−/− mice were subjected to the OPC re-challenge model. Daily weight measurements are indicated as a percent of starting weight. N.s., not significant by ANOVA. Inset: Fungal burdens on day 5 post re-challenge are indicated. B. CD8−/− mice enhance Th17 cells but not Th1 cells upon re-challenge. On day 3 post re-challenge, cLN cells from WT or CD8−/− mice were gated on lymphocytes, CD3+ cells and CD4+ cells. The frequency of IL-17+ and IFNγ+ cells among the CD4+ population is shown. Data are normalized to isotype controls. *p<0.05 by t-test with Mann-Whitney correction. C. CD8−/− mice secrete IL-17 upon re-challenge with Candida in a CD4-dependent manner. Cells from cLN of indicated mice were isolated 3 d post re-challenge and cultured in vitro for 5 d ± HK C. albicans ± anti-CD4 neutralizing Abs. IL-17A or IFNγ were assessed by ELISA. Note that this is from the same experiment presented in Fig 4D. *p<0.05 by Mann-Whitney t-test.
Functional compensation by Tc17 and DN cells in CD4−/− mice
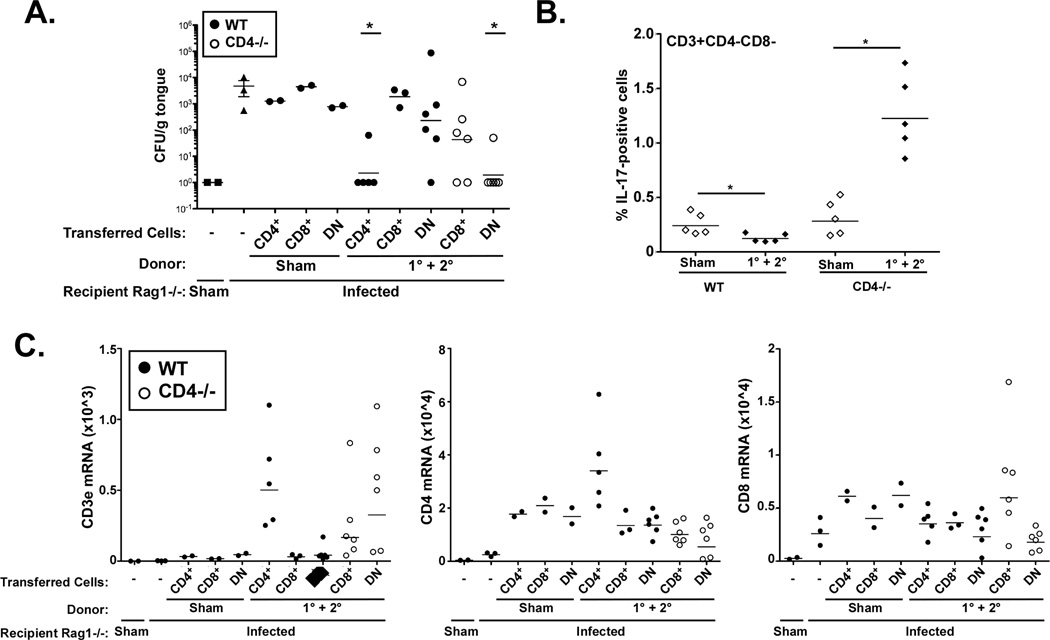
We next determined whether the CD8+ “Tc17” cells from re-challenged CD4-deficient hosts were capable of mediating immunity to OPC. To that end, Rag1−/− mice were adoptively transferred with CD4+ cells, CD8+ cells or CD4-CD8- double negative (DN) cells derived from WT or CD4−/− donors (Supplementary Fig S1B). Cells from Sham-infected WT donors did not provide any protection from OPC. As expected, CD4+ cells but not CD8+ or DN cells from infected WT donors were protective. Also as predicted, CD8+ cells from infected CD4−/− mice provided detectable (although variable) protection from OPC. Unexpectedly, the DN population from CD4−/− mice were also protective, even more consistently than the CD8+ population (Fig 6A). Based on these observations, we evaluated IL-17 expression in the DN population from WT and CD4−/− mice. IL-17 was indeed expressed in the DN cells, but only in the context of CD4 deficiency (Fig 6B).
Figure 6. CD8+ and DN cells protect from OPC in the context of CD4-deficiency.
A. WT (filled circles) or CD4−/− mice (open circles) were subjected to sham infection or re-challenge (1°+2° infections). CD4+, CD8+ and DN cells were purified by magnetic sorting and transferred into Rag1−/− recipients, which were then subjected to OPC or Sham infections, as indicated. Fungal load after 4 days was assessed by plating. B. CD3+CD4-CD8- (DN) cells express IL-17 upon re-challenge in CD4−/− but not WT mice. Percent of DN cells expressing IL-17 by ICS is indicated. * p<0.05 by Mann Whitney t-test. C. Expression of T cell markers in tongue correlates with disease protection. Rag1−/− recipients were adoptively transferred with the indicated cell populations (CD4+, CD8+ or DN) from WT sham or infected mice. Tongue mRNA was evaluated for cd3e, cd4 or cd8 by qPCR (multiplied by 104). Each data point indicates a single mouse analyzed in triplicate.
To verify that the transferred cell populations were mediating a local response in the oral mucosa, we performed qPCR on tongue mRNA samples. As shown, CD3ε expression in tongue correlated with protection from OPC, suggesting that the relevant effector populations were being recruited and/or expanding in situ (i.e., CD3+CD4+ cells from WT donors and CD3+CD8 and CD3+CD4-CD8- [DN] cells from CD4−/− donors) (Fig 6C). A similar observation was made for CD4 and CD8 mRNA expression, which correlated with the protective IL-17-producing populations (Fig 6C). Collectively, these results demonstrate that under normal circumstances, CD4+ Th17 cells and not CD8+ or DN cells mediate IL-17-dependent immunity during adaptive responses to OPC. However, in conditions of CD4-deficiency, CD8 “Tc17” cells and DN cells can serve as alternate sources of IL-17 that are able to promote effective immunity to Candida albicans. This finding illustrates the highly flexible nature of the anti-fungal immune response.
Discussion
The goal of this study was to determine the nature of long-term T cell response to OPC taking advantage of the fact that mice are not normally colonized with Candida and do not have baseline levels of Candida-reactive T cells. Upon re-challenge, we observed bona fide antigen-specific Th17 responses generated against Candida. There was no evidence for a CD8+IL-17+ (Tc17) response, nor were CD3-IL-17+, CD4+IFNγ+, CD8+IFNγ+ or IFN+IL-17+ double-expressing T cells detectable by flow cytometry during recall (Fig 2–3). There was, however, a small but reproducible induction of IFNγ following in vitro challenge with HK Candida (Fig 3D), indicating that Th1 cells are generated at low levels and may potentially participate in antifungal responses. Generation of this Th17-dominant response correlates with improved clearance of Candida, and CD4+ T cells were sufficient to confer immunity to OPC in susceptible Rag1−/− hosts (Figs 2G–H, 6), demonstrating a functional role for Candida-specific Th17 cells.
The finding that adaptive Th17 responses provided a ~1 log reduction of oral fungal burden is significant (Fig 2B), while highlighting challenges associated with improving antifungal immunity. There are presently no vaccines to any fungal organisms, so it is imperative to define correlates of immunity that could provide clinical benefit. The only experimental vaccine to Candida where efficacy has been evaluated in OPC is based on the cell wall adhesin Als3, which conferred less than 1 log protection upon challenge (34). Notably, we observed a Th17-specific recall response to this protein following Candida infection (Fig 3C). During disseminated candidiasis, a vaccine consisting of DCs transfected with C. albicans RNA caused only a 5-fold decrease in fungal burden (35). Similarly, vaccination with antibody-inducing cell wall preparations of Candida resulted in, at most, a ~2 log decrease in fungal burden following intravenous or intravaginal challenge (36). Thus, there is clearly a need for optimization of antifungal immune responses, all the more challenging given that the _target population for such vaccines is usually immunocompromised (e.g., HIV/AIDS patients). Although our findings support the idea that Candida-specific Th17 cells are protective during acute infection, the time frames employed in this study were to brief to demonstrate true immunologic memory, which will be essential for any effective immunization strategy. Further efforts to probe the issue of Th17 memory generation and maintenance are therefore still warranted.
An unexpected finding was compensatory IL-17 production in the context of CD4-deficiency. Whereas in WT mice IL-17 was only made by CD4+ T cells during recall Candida infections, both CD8+ and DN T cells from CD4−/− mice expressed IL-17 upon re-challenge (Fig 4,6). This compensatory phenotype helps explain the resistance of CD4−/− mice to OPC. The DN cells in the CD4−/− mice are likely to be MHC Class II-restricted T cells that have been previously shown to exist in high numbers in CD4-deficient mice (37), although to our knowledge they have not previously been shown to secrete IL-17. Compensatory CD8 T cell responses in CD4-deficiency have been observed in HIV/SIV infection (38). For example, in HIV patients with low CD4 counts, IL-17+γδ+ T cells reactive to Candida are expanded (39). Both Th17 and Tc17 cells are observed in SIV-infected rhesus macaques, with preferential loss of Th17 but not Tc17 in early phases of disease (40). Compensatory CD8+ “Tc17” cells were also recently described in a model of immunity to Blastomyces dermatitidis. In that system, Blastomyces-specific Tc17 cells were induced upon vaccination in the absence of CD4+ T cell help, and protected mice from lethal challenge. Moreover, vaccination-dependent influx of neutrophils into the lungs correlated with protection and was dependent on vaccine-induced Tc17 cells (10).
The regulation of Th17 memory cells in settings of infection is beginning to be understood. A recent proteomics study of Candida epitopes identified MHC Class II-bound peptides derived from Candida cell wall adhesins, Als1 and Als3. Th17 cells recognizing these antigens were found in significant numbers in both human and murine memory T cell repertoires (33). Consistently, we saw reactivity to this Als1/3 peptide in Th17 cells from Candida re-challenged mice (Fig 3C). Th17 cells are challenging to understand due to their plasticity in vivo (41), as they frequently interconvert with Th1 cells or Tregs (42, 43). Using a lineage-tracking system to track the fate of IL-17-expressing cells, Stockinger’s group reported that Th17 cells convert to dual-expressing IL-17+IFNγ+ “Th1/17” cells and IL-17-IFNγ Th1 cells in settings of chronic autoimmunity. However, they observed minimal interconversion in the setting of acute dermal candidiasis, where γδ-TCR+ cells were found to predominate (42). We found that the Th17 recall response is stable and specific, as there was little generation of either IL-17/IFNγ double-expressing cells or IFNγ-expressing cells, and no IFNγ was detected in the oral mucosa upon adoptive transfer of primed CD4+ T cells into Rag1−/− hosts (Fig 2H). This agrees with our observation that IL-23−/− and IL-17RA−/− mice remain chronically infected (Fig 1) (6), though contrasts with a report that Candida responsive Th17 cells in humans often co-express IFNγ, particularly after in vitro culture (13).
Resistance to OPC in CD4−/− and CD8−/− mice differs from the overt disease seen in IL-23−/− and IL-17R−/− mice at both short and long time points (6) (Fig 1). These findings suggest the existence of a powerful innate IL-17 response, which is presumably still operative during adaptive responses. In that regard, many innate sources of IL-17 have been identified, including NKT, γδ T, and ILCs (44, 45). Indeed, models of dermal candidiasis implicate innate γδ-T cells rather than adaptive IL-17-expressing cells (42, 46). However, surprisingly little is known about oral mucosal immunity in mice, or how accurately such responses translate to humans. Mice are coprophagic and may routinely mount powerful antimicrobial responses to prevent disease transmission from fecal matter. Saliva is another important facet of oral innate immunity; IL-23−/− and IL-17RA−/− mice as well as HIES patients (who are Th17 deficient) have defects in salivary anti-Candida activity, associated with reduced expression of antimicrobial proteins such as defensins and histatins (6). An intriguing new report indicates that monocytes exhibit epigenetic modifications following Candida infection that contributes to a protective response (47). Therefore, immunity to OPC involves orchestration of both innate and adaptive sources of IL-17.
Regardless of source, IL-17 is essential for host defense against Candida infections (26, 48, 49). The mechanisms by which IL-17 mediates antifungal immunity are not fully delineated, but a major function of IL-17 is to mobilize neutrophils. IL-17 induces expression of neutrophil-recruiting cytokines and genes such as G-CSF, CXCL1, CXCL2 and CXCL5, and neutrophil influx correlates with disease protection (50, 51). Intriguingly, Candida appears to evade the IL-17 response through a virulence factor that skews towards a Th1 phenotype through manipulation of the IDO pathway, supporting the idea that IL-17 is vital for defense (52).
While there are parallels between instinal and oral mucosa, there are key differences. The oral cavity has no M cells or Peyer’s Patches (53). The composition of the oral microbiome is also unique (54), and it is not known whether particular species of oral microbes dictate Th17 cell levels in the mouth as they do in the intestine (55). We do not detect basal levels of IL-17 in tongue even by sensitive RT-PCR methods, suggesting that oral flora does not promote a tonic level of IL-17-expressing cells (data not shown). It is noteworthy that IL-17 and IL-23 appear to be pathogenic in a model of gastric candidiasis (11, 56), though gastric infection with Candida in humans is not a clinical problem. In vaginal candidiasis the role of the Th17/IL-17 pathway is unclear, with some evidence supporting a role for IL-17 (57) but studies in mice suggesting that innate effectors such as S100 proteins and annexins are more important (1, 58, 59). This dichotomy of IL-17-dependent protection versus pathology in different models of mucosal candidiasis illustrates the point that lessons from the gut mucosa cannot always be applied to the mouth.
Methods and Materials
Mice
Mice were on the C57BL/6 background and were age- and sex-matched. IL-23p19−/− mice were provided by Genentech (S. San Francisco, CA) and bred in-house. All other mice were from The Jackson Laboratory (Bar Habor, ME). Protocols were approved by the University of Pittsburgh IACUC, and adhered to guidelines in the Guide for the Care and Use of Laboratory Animals of the NIH.
OPC recall infection model
Mice aged 5–6 weeks (minimum n=3 per cohort) were inoculated sublingually with a 0.0025g cotton ball saturated in a C. albicans suspension of 2 × 107 CFU/ml for 75 mins under anesthesia (6, 29). Six weeks after the primary infection, mice were re-challenged by the same procedure. The oral cavity was swabbed immediately prior to each infection and streaked on YPD to verify the absence of Candida. 1–5 d post re-challenge, the tongue was homogenized on a Gentle MACS Dissociator (Miltenyi Biotec Auburn, CA) and plated on YPD-AMP for 48 h at 30°C followed by colony enumeration in triplicate. For cell transfer experiments, cLN cells were harvested from WT mice 3 days after re-challenge and pooled. CD4+ cells were isolated by positive selection using Miltenyi Biotec CD4 (L3T4) MicroBeads and LS columns. The resulting CD4+, CD4-, CD8+ or CD4-CD8- (DN) fractions were transferred into Rag1−/− recipients (stock number 002216) i.p., and 24 h later mice were infected orally as described above. A total of 107 CD4+ cells and 2 × 107 CD4- cells were transferred in 200µl PBS. For sham transfers, transferred cells were from total body LN. Data were analyzed on Graphpad Prism (v. 5) using t-tests with Mann-Whitney correction (p<0.05 considered significant).
Culture of C. albicans and stimulation in vitro
C. albicans (strain CAF2-1) was cultured in YPD at 30°C overnight with agitation. A heat-killed (HK) extract was prepared with 1 ml (~ 4×108 cells) culture boiled for 45 mins. ALS1/3 peptide (KGLNDWNYPVSSESFSYT) (33) was obtained from Biosynthesis (Lewisville, TX). Cervical LN stimulation was performed by plating 106 cells per well in the presence or absence of 2×106 HK C. albicans or 5–10 µg/ml ALS1/3 peptide (pals) diluted in serum-free AIM V media (GIBCO, Invitrogen) with 20 U/ml IL-2 ± anti-CD4 Abs (BD Biosciences, clone RM4-5, 5µg/ml) or anti-MHC II (eBiosciences, clone M5/114.15.2, 10µg/ml). Supernatants were analyzed in duplicate for IL-17 and IFNγ by ELISA (eBiosciences).
Intracellular cytokine staining and flow cytometry
106 cLN cells/well were rested overnight at 37°C in serum-free AIM V media + 20 U/ml IL-2. Cells were stimulated with 50 ng/ml PMA and 500 ng/ml Ionomycin (Sigma, St Louis MO) for 4 h in the presence of Golgi Plug (BD Biosciences, San Diego, CA). Following stimulation, cells were stained for CD3 APC-Cy7 (clone 145-2C11), CD4 FITC (clone GK1.5) and CD8 PerCP (clone 53–6.7). IL-17 and IFNγ were detected with anti-IL-17-PE and anti-IFNγ-APC. Activation markers were assessed with CD44 eFluor 450 (clone IM7) and CD27 APC (clone LG.7F9). Dead cell exclusion was performed using Live/Dead Violet Viability/Vitality Dye Kit (Molecular Probes/Invitrogen). ICS was performed with the Cytofix Cytoperm kit (BD Biosciences). Data was acquired on an LSR II and analyzed with Flowjo.
RNA extraction and real time RT-PCR
Frozen tongue was homogenized in RLT lysis buffer (RNAeasy Kit, Qiagen) with a GentleMACS Dissociator (M-tubes, RNA02 program, Miltenyi). RNA was extracted with RNAeasy Kit. 1µg total RNA was used to synthesize cDNA with a SuperScript III First-Strand Synthesis System (Invitrogen Carlsbad CA). Relative quantification of indicated genes was determined by real-time PCR with SYBR Green (Quanta BioSciences, Inc.) normalized to GAPDH. Primers were from SA Biosciences (Qiagen Valencia, CA). Results were analyzed on a 7300 Real Time PCR System (Applied Biosystems Carlsbad, CA).
Supplementary Material
A. CD4+ and CD4- cLN cell fractions were isolated from WT mice 3 days post re-challenge and transferred into Rag1−/− hosts 24 hours prior to 1° infection. Four days after infection the tongues of recipient mice were analyzed for fungal burden and IL-17 mRNA. As controls for both fungal burden and baseline IL-17 mRNA expression, Sham- or Candida-infected Rag1−/− mice that did not receive cells were included. B. CD4+, CD8+ and CD4-CD8-(DN) cLN cell fractions were isolated from WT or CD4−/− mice 3 days post re-challenge and transferred into Rag1−/− hosts 24 hours prior to 1° infection. Four days after infection the tongue of recipient Rag1−/− mice was analyzed for fungal burden and CD3ε, CD4 and CD8 mRNA levels. Controls are as in panel A above.
A. CD4+ cells but not CD8+ cells express IL-17 five days after recall infections with Candida albicans. cLN cells from mice subjected to Sham infection or re-challenge (1°+2° infection) were isolated 5 days later, and subjected to surface and ICS for IL-17 and IFNγ. Lymphocytes (determined by forward and side scatter profiles) were gated on CD3 and CD4, and IL-17+ and IFNγ+ cell frequencies (normalized to isotype) are depicted. B. CD3-negative cells in WT mice express baseline levels of IL-17 and IFNγ, but are unchanged upon infection with Candida. CD3- negative populations from cLN of WT mice subjected to the re-challenge model were analyzed for IL-17 and IFNγ by ICS. Data are normalized to isotype controls (not shown). *p<0.05 by Mann-Whitney t-test. N.s., not significant. C. CD3- negative cells from CD4−/− mice express baseline levels of IL-17 and IFNγ similar to WT mice, but are unchanged upon infection with Candida. CD3-negative populations from cLN of CD4−/− mice subjected to the re-challenge model were analyzed for IL-17 and IFNγ by ICS. Data are normalized to the isotype control (not shown). * p<0.05.
Acknowledgments
SLG was supported by NIH grants AR054389 and DE022550.
KCM was supported by EY018355 and SK by HL105427. ACP was supported by the Medical Scientist Training Program at the University of Pittsburgh. NHS was supported by NIH Training Grant T32-CA082084. ARH was supported by Children’s Hospital of Pittsburgh of UPMC and a Pediatric Infectious Disease Society Award (funded by the Stanley A Plotkin Sanofi Pasteur Fellowship Award). We thank Genentech (South San Francisco) for kindly providing IL-23−/− mice. We thank EC Childs, A Mamo and M Bridi for assistance. We are grateful to Drs. M McGeachy, LA Darville, JK Kolls, S Nanjappa, BS Klein and HR Conti for critical reading and helpful suggestions.
Abbreviations
- APS-1
autoimmune polyendocrinopathy syndrome 1
- AMP
antimicrobial peptide
- BD
β defensin
- CFU
colony forming units
- cLN
cervical lymph node
- CMC
chronic mucocutaneous candidiasis
- DN
double negative
- ICS
intracellular cytokine staining
- HK
heat killed
- OPC
oropharyngeal candidiasis
- TCR
T cell receptor
Footnotes
Conflicts of interest: SLG has received a research grant from Amgen, honoraria and travel reimbursements from Novartis, and consults for Lycera Corp.
References
- 1.Dongari-Bagtoglou A, Fidel P. The host cytokine responses and protective immunity in oropharyngeal candidiasis. J Dent Res. 2005;84:966–977. doi: 10.1177/154405910508401101. [DOI] [PubMed] [Google Scholar]
- 2.Klein RS, Harris CA, Small CB, Moll B, Lesser M, Friedland GH. Oral candidiasis in high-risk patients as the initial manifestation of the acquired immunodeficiency syndrome. N Engl J Med. 1984 Aug 9;311(6):354–358. doi: 10.1056/NEJM198408093110602. [DOI] [PubMed] [Google Scholar]
- 3.Dong C. Diversification of T-helper-cell lineages: finding the family root of IL-17-producing cells. Nat Rev Immunol. 2006 Apr;6(4):329–333. doi: 10.1038/nri1807. [DOI] [PubMed] [Google Scholar]
- 4.Steinman L. A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage. Nature Med. 2007 Feb;13(2):139–145. doi: 10.1038/nm1551. [DOI] [PubMed] [Google Scholar]
- 5.Farah C, Hu Y, Riminton S, Ashman R. Distinct roles for interleukin-12p40 and tumour necrosis factor in resistance to oral candidiasis defined by gene _targeting. Oral Microbiol Immunol. 2006;21:252–255. doi: 10.1111/j.1399-302X.2006.00288.x. [DOI] [PubMed] [Google Scholar]
- 6.Conti H, Shen F, Nayyar N, Stocum E, JN S, Lindemann M, et al. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J Exp Med. 2009;206(2):299–311. doi: 10.1084/jem.20081463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ho A, Shen F, Conti H, Patel N, Childs E, Peterson A, et al. IL-17RC is required for immune signaling via an extended SEFIR domain in the cytoplasmic tail. J Immunol. 2010;185:1063–1070. doi: 10.4049/jimmunol.0903739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin L, Ibrahim AS, Xu X, Farber JM, Avanesian V, Baquir B, et al. Th1–Th17 cells mediate protective adaptive immunity against Staphylococcus aureus and Candida albicans infection in mice. PLoS Pathog. 2009 Dec;5(12) doi: 10.1371/journal.ppat.1000703. e1000703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wuthrich M, Gern B, Hung CY, Ersland K, Rocco N, Pick-Jacobs J, et al. Vaccine-induced protection against 3 systemic mycoses endemic to North America requires Th17 cells in mice. J Clin Invest. 2011 Feb 1;121(2):554–568. doi: 10.1172/JCI43984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nanjappa SG, Heninger E, Wuthrich M, Gasper DJ, Klein BS. Tc17 Cells Mediate Vaccine Immunity against Lethal Fungal Pneumonia in Immune Deficient Hosts Lacking CD4(+) T Cells. PLoS Pathog. 2012 Jul;8(7) doi: 10.1371/journal.ppat.1002771. e1002771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zelante T, De Luca A, Bonifazi P, Montagnoli C, Bozza S, Moretti S, et al. IL-23 and the Th17 pathway promote inflammation and impair antifungal immune resistance. Eur J Immunol. 2007 Sep 26;37(10):2695–2706. doi: 10.1002/eji.200737409. [DOI] [PubMed] [Google Scholar]
- 12.Acosta-Rodriguez EV, Rivino L, Geginat J, Jarrossay D, Gattorno M, Lanzavecchia A, et al. Surface phenotype and antigenic specificity of human interleukin 17-producing T helper memory cells. Nature Immunol. 2007 May 7;8:639–646. doi: 10.1038/ni1467. [DOI] [PubMed] [Google Scholar]
- 13.Zielinski CE, Mele F, Aschenbrenner D, Jarrossay D, Ronchi F, Gattorno M, et al. Pathogen-induced human T(H)17 cells produce IFN-gamma or IL-10 and are regulated by IL-1beta. Nature. 2012 Apr 1; doi: 10.1038/nature10957. [DOI] [PubMed] [Google Scholar]
- 14.Huppler AR, Bishu S, Gaffen SL. Mucocutaneous candidiasis: the IL-17 pathway and implications for _targeted immunotherapy. Arthritis Res Ther. 2012 Jul 23;14(4):217. doi: 10.1186/ar3893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klatt NR, Brenchley JM. Th17 cell dynamics in HIV infection. Curr Opin HIV AIDS. 2010 Mar;5(2):135–140. doi: 10.1097/COH.0b013e3283364846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Z, Laurence A, Kanno Y, Pacher-Zavisin M, Zhu BM, Tato C, et al. Selective regulatory function of Socs3 in the formation of IL-17-secreting T cells. Proc Natl Acad Sci U S A. 2006 May 12;103(21):8137–8142. doi: 10.1073/pnas.0600666103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang XO, Panopoulos AD, Nurieva R, Chang SH, Wang D, Watowich SS, et al. STAT3 regulates cytokine-mediated generation of inflammatory helper T cells. J Biol Chem. 2007 Mar 30;282(13):9358–9363. doi: 10.1074/jbc.C600321200. [DOI] [PubMed] [Google Scholar]
- 18.Freeman AF, Holland SM. The hyper-IgE syndromes. Immunology and allergy clinics of North America. 2008 May;28(2):277–291. doi: 10.1016/j.iac.2008.01.005. viii. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma CS, Chew GY, Simpson N, Priyadarshi A, Wong M, Grimbacher B, et al. Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. J Exp Med. 2008 Jul 7;205(7):1551–1557. doi: 10.1084/jem.20080218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milner JD, Brenchley JM, Laurence A, Freeman AF, Hill BJ, Elias KM, et al. Impaired T(H)17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 2008 Mar 12;452:773–776. doi: 10.1038/nature06764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van de Veerdonk FL, Plantinga TS, Hoischen A, Smeekens SP, Joosten LA, Gilissen C, et al. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N Engl J Med. 2011 Jul 7;365(1):54–61. doi: 10.1056/NEJMoa1100102. [DOI] [PubMed] [Google Scholar]
- 22.Liu L, Okada S, Kong XF, Kreins AY, Cypowyj S, Abhyankar A, et al. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J Exp Med. 2011 Jul 4;208:1635–1648. doi: 10.1084/jem.20110958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glocker EO, Hennigs A, Nabavi M, Schaffer AA, Woellner C, Salzer U, et al. A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N Engl J Med. 2009 Oct 29;361(18):1727–1735. doi: 10.1056/NEJMoa0810719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Plantinga TS, van der Velden WJ, Ferwerda B, van Spriel AB, Adema G, Feuth T, et al. Early stop polymorphism in human DECTIN-1 is associated with increased candida colonization in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2009 Sep 1;49(5):724–732. doi: 10.1086/604714. [DOI] [PubMed] [Google Scholar]
- 25.Puel A, Doffinger R, Natividad A, Chrabieh M, Barcenas-Morales G, Picard C, et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J Exp Med. 2010 Feb 15;207(2):291–297. doi: 10.1084/jem.20091983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Browne SK, Holland SM. Immunodeficiency secondary to anticytokine autoantibodies. Curr Opin Allergy Clin Immunol. 2010 Dec;10(6):534–541. doi: 10.1097/ACI.0b013e3283402b41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kisand K, Boe Wolff AS, Podkrajsek KT, Tserel L, Link M, Kisand KV, et al. Chronic mucocutaneous candidiasis in APECED or thymoma patients correlates with autoimmunity to Th17-associated cytokines. J Exp Med. 2010 Feb 15;207(2):299–308. doi: 10.1084/jem.20091669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Puel A, Cypowji S, Bustamante J, Wright J, Liu L, Lim H, et al. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–68. doi: 10.1126/science.1200439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kamai Y, Kubota M, Kamai Y, Hosokawa T, Fukuoka T, Filler S. New model of oropharyngeal candidiasis in mice. Anti-microb Agents Chemo. 2001;45:3195–3197. doi: 10.1128/AAC.45.11.3195-3197.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pearson C, Uhlig HH, Powrie F. Lymphoid microenvironments and innate lymphoid cells in the gut. Trends Immunol. 2012 Jun;33(6):289–296. doi: 10.1016/j.it.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Buonocore S, Ahern PP, Uhlig HH, Ivanov II, Littman DR, Maloy KJ, et al. Innate lymphoid cells drive interleukin-23-dependent innate intestinal pathology. Nature. 2010 Apr 29;464(7293):1371–1375. doi: 10.1038/nature08949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scurlock AM, Frazer LC, Andrews CW, Jr, O'Connell CM, Foote IP, Bailey SL, et al. Interleukin-17 contributes to generation of Th1 immunity and neutrophil recruitment during Chlamydia muridarum genital tract infection but is not required for macrophage influx or normal resolution of infection. Infect Immun. 2011 Mar;79(3):1349–1362. doi: 10.1128/IAI.00984-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bär E, Gladiator A, Bastidas S, Roschitzki B, Acha-Orbea H, Oxenius A, et al. A novel Th cell epitope of Candida albicans mediates protection from fungal infection. J Immunol. 2012 Jun 1;188(11):5636–5643. doi: 10.4049/jimmunol.1200594. [DOI] [PubMed] [Google Scholar]
- 34.Spellberg BJ, Ibrahim AS, Avanesian V, Fu Y, Myers C, Phan QT, et al. Efficacy of the anti-Candida rAls3p-N or rAls1p-N vaccines against disseminated and mucosal candidiasis. J Infect Dis. 2006 Jul 15;194(2):256–260. doi: 10.1086/504691. [DOI] [PubMed] [Google Scholar]
- 35.Bozza S, Montagnoli C, Gaziano R, Rossi G, Nkwanyuo G, Bellocchio S, et al. Dendritic cell-based vaccination against opportunistic fungi. Vaccine. 2004 Feb 17;22(7):857–864. doi: 10.1016/j.vaccine.2003.11.031. [DOI] [PubMed] [Google Scholar]
- 36.Casadevall A, Pirofski LA. Immunoglobulins in defense, pathogenesis, and therapy of fungal diseases. Cell Host Microbe. 2012 May 17;11(5):447–456. doi: 10.1016/j.chom.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tyznik AJ, Sun JC, Bevan MJ. The CD8 population in CD4-deficient mice is heavily contaminated with MHC class II-restricted T cells. J Exp Med. 2004 Feb 16;199(4):559–565. doi: 10.1084/jem.20031961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fidel PL., Jr Candida-Host Interactions in HIV Disease: Implications for Oropharyngeal Candidiasis. Adv Dent Res. 2011 Apr;23(1):45–49. doi: 10.1177/0022034511399284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fenoglio D, Poggi A, Catellani S, Battaglia F, Ferrera A, Setti M, et al. Vδ1 T lymphocytes producing IFN-γ and IL-17 are expanded in HIV-1-infected patients and respond to Candida albicans. Blood. 2009 Jun 25;113(26):6611–6618. doi: 10.1182/blood-2009-01-198028. [DOI] [PubMed] [Google Scholar]
- 40.Nigam P, Kwa S, Velu V, Amara RR. Loss of IL-17-producing CD8 T cells during late chronic stage of pathogenic simian immunodeficiency virus infection. J Immunol. 2011 Jan 15;186(2):745–753. doi: 10.4049/jimmunol.1002807. [DOI] [PubMed] [Google Scholar]
- 41.Lee YK, Turner H, Maynard CL, Oliver JR, Chen D, Elson CO, et al. Late developmental plasticity in the T helper 17 lineage. Immunity. 2009 Jan;30(1):92–107. doi: 10.1016/j.immuni.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hirota K, Duarte JH, Veldhoen M, Hornsby E, Li Y, Cua DJ, et al. Fate mapping of IL-17-producing T cells in inflammatory responses. Nature immunology. 2011 Mar;12(3):255–263. doi: 10.1038/ni.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pepper M, Linehan JL, Pagan AJ, Zell T, Dileepan T, Cleary PP, et al. Different routes of bacterial infection induce long-lived TH1 memory cells and short-lived TH17 cells. Nature Immunol. 2010 Jan;11(1):83–89. doi: 10.1038/ni.1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat Rev Immunol. 2010 Jul;10(7):479–489. doi: 10.1038/nri2800. [DOI] [PubMed] [Google Scholar]
- 45.Dungan LS, Mills KH. Caspase-1-processed IL-1 family cytokines play a vital role in driving innate IL-17. Cytokine. 2011 Oct;56(1):126–132. doi: 10.1016/j.cyto.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 46.Kagami S, Rizzo HL, Kurtz SE, Miller LS, Blauvelt A. IL-23 and IL-17A, but not IL-12 and IL-22, are required for optimal skin host defense against Candida albicans. J Immunol. 2010 Nov 1;185(9):5453–5462. doi: 10.4049/jimmunol.1001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quintin J, Saeed S, Martens JH, Giamarellos-Bourboulis EJ, Ifrim DC, Logie C, et al. Candida albicans Infection Affords Protection against Reinfection via Functional Reprogramming of Monocytes. Cell Host Microbe. 2012 Aug 16;12(2):223–232. doi: 10.1016/j.chom.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hernández-Santos N, Gaffen SL. Th17 cells in immunity to Candida albicans. Cell Host Microbe. 2012;11:425–435. doi: 10.1016/j.chom.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Puel A, Picard C, Cypowyj S, Lilic D, Abel L, Casanova JL. Inborn errors of mucocutaneous immunity to Candida albicans in humans: a role for IL-17 cytokines? Curr Opin Immunol. 2010 Aug;22(4):467–474. doi: 10.1016/j.coi.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Iwakura Y, Ishigame H, Saijo S, Nakae S. Functional specialization of interleukin-17 family members. Immunity. 2011;34:149–162. doi: 10.1016/j.immuni.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 51.Naglik J, Moyes D. Epithelial cell innate response to Candida albicans. Adv Dent Res. 2011;23:50–55. doi: 10.1177/0022034511399285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cheng SC, van de Veerdonk F, Smeekens S, Joosten LA, van der Meer JW, Kullberg BJ, et al. Candida albicans Dampens Host Defense by Downregulating IL-17 Production. J Immunol. 2010 Jul 12;185:2450–2457. doi: 10.4049/jimmunol.1000756. [DOI] [PubMed] [Google Scholar]
- 53.Kweon M. Sublingual mucosa: A new vaccination route for systemic and mucosal immunity. Cytokine. 2011;54:1–5. doi: 10.1016/j.cyto.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 54.Bik EM, Long CD, Armitage GC, Loomer P, Emerson J, Mongodin EF, et al. Bacterial diversity in the oral cavity of 10 healthy individuals. ISME J. 2010 Aug;4(8):962–974. doi: 10.1038/ismej.2010.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ivanov II, Frutos Rde L, Manel N, Yoshinaga K, Rifkin DB, Sartor RB, et al. Specific microbiota direct the differentiation of IL-17-producing T-helper cells in the mucosa of the small intestine. Cell Host Microbe. 2008 Oct 16;4(4):337–349. doi: 10.1016/j.chom.2008.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zelante T, Iannitti R, De Luca A, Romani L. IL-22 in antifungal immunity. Eur J Immunol. 2011 Feb;41(2):270–275. doi: 10.1002/eji.201041246. [DOI] [PubMed] [Google Scholar]
- 57.Pietrella D, Rachini A, Pines M, Pandey N, Mosci P, Bistoni F, et al. Th17 cells and IL-17 in protective immunity to vaginal candidiasis. PLoS One. 2011;6(7):e22770. doi: 10.1371/journal.pone.0022770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lilly EA, Yano J, Fidel PL., Jr Annexin-A1 identified as the oral epithelial cell anti-Candida effector moiety. Mol Oral Microbiol. 2010 Aug;25(4):293–304. doi: 10.1111/j.2041-1014.2010.00579.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yano J, Lilly E, Barousse M, Fidel PL., Jr Epithelial cell-derived S100 calcium-binding proteins as key mediators in the hallmark acute neutrophil response during Candida vaginitis. Infect Immun. 2010 Dec;78(12):5126–5137. doi: 10.1128/IAI.00388-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. CD4+ and CD4- cLN cell fractions were isolated from WT mice 3 days post re-challenge and transferred into Rag1−/− hosts 24 hours prior to 1° infection. Four days after infection the tongues of recipient mice were analyzed for fungal burden and IL-17 mRNA. As controls for both fungal burden and baseline IL-17 mRNA expression, Sham- or Candida-infected Rag1−/− mice that did not receive cells were included. B. CD4+, CD8+ and CD4-CD8-(DN) cLN cell fractions were isolated from WT or CD4−/− mice 3 days post re-challenge and transferred into Rag1−/− hosts 24 hours prior to 1° infection. Four days after infection the tongue of recipient Rag1−/− mice was analyzed for fungal burden and CD3ε, CD4 and CD8 mRNA levels. Controls are as in panel A above.
A. CD4+ cells but not CD8+ cells express IL-17 five days after recall infections with Candida albicans. cLN cells from mice subjected to Sham infection or re-challenge (1°+2° infection) were isolated 5 days later, and subjected to surface and ICS for IL-17 and IFNγ. Lymphocytes (determined by forward and side scatter profiles) were gated on CD3 and CD4, and IL-17+ and IFNγ+ cell frequencies (normalized to isotype) are depicted. B. CD3-negative cells in WT mice express baseline levels of IL-17 and IFNγ, but are unchanged upon infection with Candida. CD3- negative populations from cLN of WT mice subjected to the re-challenge model were analyzed for IL-17 and IFNγ by ICS. Data are normalized to isotype controls (not shown). *p<0.05 by Mann-Whitney t-test. N.s., not significant. C. CD3- negative cells from CD4−/− mice express baseline levels of IL-17 and IFNγ similar to WT mice, but are unchanged upon infection with Candida. CD3-negative populations from cLN of CD4−/− mice subjected to the re-challenge model were analyzed for IL-17 and IFNγ by ICS. Data are normalized to the isotype control (not shown). * p<0.05.