Abstract
Context
Characterizing where people die is needed to inform palliative care programs in Mexico.
Objectives
To determine whether access to health care influences the place of death of older Mexicans and examine the modifying effects of demographic and clinical characteristics.
Methods
We analyzed 2001 baseline and 2003 follow-up data from the Mexican Health and Aging Study. Cases included adults who completed the baseline interview and died before the follow-up interview and for whom a proxy interview was obtained in 2003. The main outcome variable was the place of death (hospital vs. home). The predictors of the place of death were identified using logistic regression analysis.
Results
The study group included 473 deceased patients; 52.9% died at home. Factors associated with hospital death were having spent at least one night in a hospital during the last year of life (odds ratio [OR]: 6.73; 95% confidence interval [CI]: 3.29, 13.78) and dying in a city other than the city of usual residence (OR: 4.68, 95% CI: 2.56, 8.57). Factors associated with home death were not having health care coverage (OR: 2.78, 95% CI: 1.34, 5.88), living in a city of less than 100,000 residents (OR: 2.44, 95% CI: 1.43, 4.17), and older age (OR: 1.03, 95% CI: 1.01, 1.05).
Conclusion
Older Mexicans with access to health care services were more likely to die in the hospital even after controlling for important clinical and demographic characteristics. Findings from the study may be used to plan the provision of accessible end-of-life hospital and home-based services.
Keywords: Access to health care, place of death, palliative care, aging, Mexico
Introduction
Providing quality care at the end of life for older persons is increasingly being recognized as a public health priority worldwide.1 A critical first step in the planning of palliative care programs involves assessing the needs of the _target population. Characterizing where people currently die and the factors that influence their site of death is needed to inform the development and implementation of quality palliative care programs, particularly in developing countries such as Mexico, where palliative care programs are critically and increasingly needed. This study identified the associations between the place of death of older Mexicans and access to health care, as well as the demographic and clinical characteristics of the study participants, using data from a national health survey of older Mexicans.
Palliative care programs are relatively new and evolving in Latin America. Although important new palliative care programs have emerged throughout Latin America in recent years, critical services are still unavailable or inaccessible to much of the population. The urgency for palliative care programs is especially pronounced in countries such as Mexico, where the demographic and health needs of the population are rapidly changing. The development of far-reaching palliative care programs in the region is necessitated by the increasing prevalence of chronic diseases and causes of death, the rapid aging of the population, and the late-stage diagnosis of disease and limited curative facilities in poor regions.2,3 Obstacles to the growth of palliative care in Latin America identified to date include poverty, inadequate health care coverage, unavailability and/or high cost of opioids and other medications, lack of knowledge and training related to palliative care and pain management, the fragmentation of initiatives and efforts, limited research on palliative care, and inadequate political commitment as reflected in the low prioritization of palliative care when formulating health care and health education policies.2–5
The World Health Organization (WHO) promotes a public health approach to palliative care in which comprehensive palliative care programs are integrated into the existing health systems and adapted to the specific cultural and social context of the _target populations.6 The contexts in which palliative care evolves can differ greatly across countries, as reflected by the divergent health care systems into which palliative care programs must be integrated, the varying levels of available resources, and the cultural differences in attitudes toward death and dying. The WHO has issued general recommendations for countries according to the available resources that can be tailored to specific situations. In both low- and medium-resource settings (i.e., most developing nations), the WHO recommends high coverage of patients through services provided via home-based care.6
Research, largely from developed nations, suggests that most people with progressive illness wish to die at home.1,7–11 A variety of studies also have found that more than 50% of people receiving care for a serious illness favor home care at the end of life.1 Despite the prominent preference for home care and home death, hospital deaths predominate in many countries and only a minority of persons throughout the world has access to professional end-of-life home care and the opportunity to receive this type of care when dying at home.1,7,9,12,13 Nonetheless, recent evidence from countries such as the United States, England, and Canada indicates that more people are dying outside of hospitals,14 a phenomenon that may be largely attributable to the development of successful integrated palliative care programs in these countries.13,15
Yet, the rates and trends of hospital vs. home deaths can vary greatly both within and across countries, and greater rates of home deaths in some contexts do not necessarily indicate the existence of hospice or palliative home health care programs.1 For instance, in countries such as the United States, Italy, and Spain, people in rural areas are more likely to die at home, most likely without access to palliative home care.7 Thus, variations in the place of death suggest that factors related to the health care system prominently predict the place of death, as reflected by recent U.S. data indicating that higher rates of hospital deaths are primarily influenced by the availability of hospital beds.12,16,17 Studies to date generally examined the influence of individual, clinical, social, and health care system characteristics on place of death.7–9,18 A recent systematic review on place of death in terminally ill patients found that the strongest predictors of dying at home included factors related to the illness, the individual, and the environment, specifically, low functional status, patients’ preferences, the use of home care services, and extended family support.7
In many nations, older persons are particularly vulnerable because the health care systems are fragmented,19 very few receive a pension, and frequently they do not have access to palliative care.1 In 2005, the proportion of Mexicans aged 60 years and older was 8% and is projected to increase to 13% by 2020.20 This rapid aging of the population means that patterns of disease in the last years of life also are changing, as more people are dying from serious chronic diseases such as cardiovascular disease, cancer, and diabetes, rather than from acute illnesses.21–24 Currently, almost 50% of deaths in Mexico occur in people aged 60 years and older,25 and the few studies that have addressed palliative care have focused exclusively on cancer.3,18,26–28 Therefore, little is known about the end-of-life needs of Mexicans who are old, the quality of care they receive, or even where they die. Decision makers and health administrators need to plan for the health needs of this rapidly growing group in Mexico23 and require evidence that identifies patterns related to place of death and the factors associated with hospital and home deaths to inform the development of palliative care programs and services in multiple settings.
The primary goal of the study was to determine if access to health care influences the place of death of older Mexicans and examine if and how this association is modified by the demographic and clinical characteristics of the study participants, using data from the Mexican Health and Aging Study (MHAS). Guided by the Phillips, et al.29 “Behavioral Model of Health Services Utilization,” we aimed to identify which groups of older persons may potentially require (use) either home- or hospital-based end-of-life services by evaluating the associations between the place of death and measures of access to health care (i.e., hospital utilization in the last year of life) and other participant characteristics (i.e., age, size of city of residence, cause of death, and health insurance coverage).
Methods
Data Sets
We conducted a retrospective analysis using data collected by the MHAS. In the MHAS, adults born before 1951 and their spouses or partners completed baseline interviews in 2001 and a follow-up interview in 2003. The data from the interviews are public data sets maintained by the Population Studies Center of the University of Pennsylvania. The MHAS at baseline is considered a nationally representative sample of the 13 million Mexicans born before 1951 and has urban/rural representations.30 The secondary analysis of these data was identified as exempt research from institutional review board (IRB) full review and approved by our institution's IRB.
The population sample used in the MHAS was drawn from the National Employment Survey (Encuesta Nacional de Empleo, ENE), conducted by the Mexican Instituto Nacional de Estadística, Geografía e Informática, equivalent to the U.S. Bureau of the Census. Details of the MHAS study have been disseminated previously.31,32
During the 2001 MHAS baseline interviews, 11,000 households contacted had an older resident adult and were eligible to participate.33 If more than one older adult was living at the home, only one was randomly selected to participate. If the _target participant had a spouse or partner, they too were interviewed. A total of 15,402 participants from 9862 households were interviewed. If the participant had died at the time of the 2003 follow-up, the interviewer attempted to conduct the interview with the widow or widower, a proxy, or next of kin. For the 2003 follow-up survey, 15,275 people in 7184 households were interviewed.33
For our study, we included patients if they were interviewed in 2001 and were reported deceased during the 2003 follow-up survey. We also included households from which both the original participant and the participant's spouse or partner were reported dead in 2003. After exclusion of 18 cases because death had occurred in a place other than home or hospital, seven cases because the place of death was unknown, and 48 cases because of unknown cause of death, a total of 473 cases remained for the study.
Measures and Theoretical Model
We defined “deceased” as the original participants who completed the baseline interview in 2001 and died before the 2003 follow-up interview. Included in this definition were the spouses or partners who died between the 2001 and 2003 interviews as reported in the MHAS files. We defined “respondent” as a widow or widower, proxy, or next of kin who answered the follow-up survey in 2003. The place of death was categorized as home or hospital.
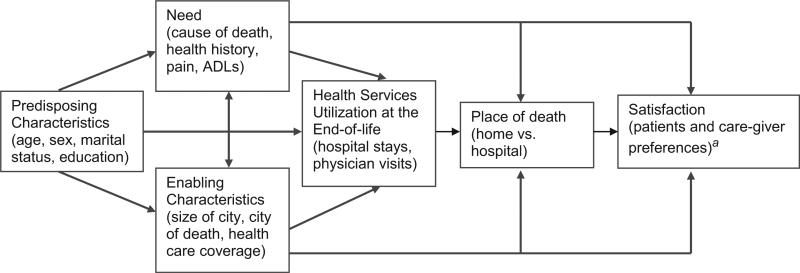
We used a modified version of the Behavioral Model of Health Services Utilization developed by Phillips et al.29 to analyze the health care system level and clinical and individual factors associated with the place of death (dependent variable) (Fig. 1). The model suggests that societal, health services system, and individual factors determine the use of health services and that access to health care can be conceptualized as a process through which input variables, such as characteristics of the health care system and the population at risk, affect outcomes (outputs), such as the actual utilization of services and consumer satisfaction with the medical care received.
Fig. 1.
Theoretical model of the effects of access to health care on the place of death and the modifying effects of predisposing, need, and enabling characteristics. aNot evaluated in the present study.
To understand the relationships between the place of death and measures of access to care, and the clinical, demographic, and individual characteristics of the study subjects, we included variables measuring need, enabling, and predisposing factors. In our model, need was subsumed under cause of death, history of health conditions, presence of pain, and performing activities of daily living (ADLs). The cause of death was categorized in the MHAS files as cardiovascular disease, cancer, diabetes, stroke, and other. The history of health conditions includes diseases diagnosed by a physician during the previous year of life. These health conditions were classified as hypertension, diabetes, cancer, respiratory illness, heart attack, stroke, and fall during the previous months. Additionally, respondents were asked to assess the frequency and severity of pain (rated by the respondent as mild, moderate, or severe) of the deceased before death. The respondent was asked whether the deceased required assistance with any of the ADLs, such as walking across the room, bathing or showering, eating, getting in and out of bed, or using the toilet, and to give the deceased's relationship to the person who provided this help. ADLs were reported in two categories: (1) no assistance needed and (2) assistance for one or more of the ADLs mentioned above. Traditionally, the ADLs scores independently assess the ability to perform each activity;33 thus, the classification used by the MHAS is equivalent to a score of 0 for those who did not need assistance and a score greater than 0 for those who needed assistance for one or more ADLs.
Enabling factors were operationalized as size of the city of usual residence, whether the death occurred in the city of usual residence, and health care coverage. The size of the city of usual residence was reported in three subcategories: (1) 100,000 or more inhabitants, (2) less than 100,000 inhabitants, and (3) unknown. The type of city (urban or rural) of usual residence was obtained from the 2001 files. Health care coverage was assessed by asking the proxy respondent if the deceased had health care coverage through a health care institution or insurance company. Because Mexico does not have a single-payer national health program, there are several governmental institutions that provide health care and cover specific segments of the population.19 Health care coverage in this study can be interpreted as those who reported either being affiliated with any of the institutions of the social security system in Mexico (i.e., Instituto Mexicano del Seguro Social, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Secretaria de Salud, Petroleos Mexicanos, and Armed Forces Health System) or those with private health care insurance.
Predisposing factors included age, sex, marital status, and years of education. We dichotomized marital status into two subcategories: (1) married or in a married-like situation and (2) not married. We extracted data on the years of education as reported in the 2001 files; the rest of the data were collected from the 2003 files.
We included measures of health care utilization in the last year of life such as number of hospital stays and physician visits. The direct nonmedical costs for medical services incurred by the deceased or family members were also included. Direct nonmedical costs include all costs not directly related to medical services, such as transportation.34 The respondents were asked about the expenditures (Mexican pesos) for the care received by the deceased during the last year of life. The exchange rate of the Mexican peso to the U.S. dollar in June 2003 was estimated at 10.54. Measures of satisfaction with care that are included in the Behavioral Model of Health Services Utilization29 were not collected by the MHAS and consequently not included in our analysis.
Statistical Analysis
We examined frequencies and measures of central tendency and reported counts (with percentages) or means, medians, minimum, and maximum values depending on the distribution. For the bivariate analysis, we used the Mann-Whitney U test for continuous variables and the t-test when appropriate. Categorical and ordinal variables were analyzed with the Chi-square test.
We constructed a logistic regression model to examine the relative importance of outcome-associated factors. Based on previous research findings,13,35 age and education were included a priori in the multivariate model. To increase the accuracy, we assessed collinearity among the covariates included in the multivariate model. Covariates were included in the multivariate model if a P-value <0.20 was obtained in the bivariate analysis. The goodness-of-fit test was checked with the Hosmer and Lemeshow test.
Because variables identifying direct non-medical costs to the deceased or family members (expenditures for utilization of health services), such as overnight hospital stays or doctor visits during the last year of life, were available in the data set, we identified subgroups of participants with different patterns of utilization of services. Therefore, we constructed a second logistic regression model that included only participants who reported direct nonmedical costs for overnight hospital stays or doctors’ visits during the last year of life. We included two dichotomous covariates assessing if participants had paid for the overnight hospital stays or doctors’ visits. As we did in the previous model, age and education were included a priori, and we examined collinearity among covariates and reported on the goodness of fit of the model using the Hosmer and Lemeshow test.
All statistical analyses were conducted using SPSS version 11.01 (SPSS Inc., Chicago, IL). For all analyses, significance was set at P < 0.05 (two-tailed).
Results
More than half (250, 52.9%) of the deceased died at home, and the mean age at death was 73.5 years. Table 1 details the characteristics of the study participants and displays the bivariate associations between the demographic factors and the primary outcome variable, place of death. The average number of years of schooling was second grade. For 160 (33.8%) participants, the widow or widower of the deceased completed the follow-up interview and the next of kin completed the rest of the interviews. For 12.0% of the deceased, someone had moved into his or her household to help provide care and 10% of the deceased had moved in with someone else, usually a close family member, to receive care. The most common specified cause of death was cardiovascular disease (22.0%), followed by cancer (19.2%).
Table 1.
Bivariate Analysis of Demographic Characteristics Associated with the Place of Death of Older Mexican Adults
| No. Deceased (%) by Place of Death |
||||
|---|---|---|---|---|
| Demographic Characteristics | Hospital, n (%) | Home, n (%) | P-value | |
| Total, n (%) | 473 (100) | 223 (47.1) | 250 (52.9) | NA |
| Mean age (median), yr | 73.5 (73) | 71.1 (72) | 75.7 (76) | ≤0.001 |
| Cause of death | 0.17 | |||
| Cardiovascular disease | 104 (22.0) | 47 (21.1) | 57 (22.8) | |
| Cancer | 91 (19.2) | 37 (16.6) | 54 (21.6) | |
| Diabetes | 71 (15.0) | 41 (18.4) | 30 (12.0) | |
| Stroke | 39 (8.2) | 22 (9.9) | 17 (6.8) | |
| Other | 168 (35.5) | 76 (34.1) | 92 (36.8) | |
| Sex | 0.82 | |||
| Female | 238 (49.7) | 111 (49.8) | 127 (50.8) | |
| Male | 235 (50.3) | 112 (50.2) | 123 (49.2) | |
| Marital status | 0.10 | |||
| Married or in a married-like situation | 246 (52.0) | 125 (56.1) | 121 (48.4) | |
| Not married | 227 (48.0) | 98 (43.9) | 129 (51.6) | |
| Years of schooling (median), yr | 2 (2) | 3 (3) | 2 (2) | 0.14 |
| Died in city of usual residence | ≤0.001 | |||
| Yes | 376 (79.5) | 154 (69.1) | 222 (88.8) | |
| No | 97 (20.5) | 69 (30.9) | 28 (11.2) | |
| Size of city of usual residence | ≤0.001 | |||
| Less than 100,000 residents | 156 (33.0) | 53 (23.8) | 103 (41.2) | |
| 100,000 or more residents | 317 (67.0) | 170 (76.2) | 147 (58.8) | |
| Health care coverage | ≤0.001 | |||
| Yesa | 363 (76.7) | 189 (84.8) | 174 (69.6) | |
| No | 58 (12.3) | 15 (6.7) | 43 (17.2) | |
| Unknown | 52 (11.0) | 19 (8.5) | 33 (13.2) | |
Percentages may not add to 100 because of rounding.
Includes Instituto Mexicano del Seguro Social, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Secretaría de Salud, Seguro Popular, Secretaría de Marina, Secretaría de la Defensa National, Petróleos Mexicanos, health insurance companies, and others.
Demographic and Geographic Factors
Most (79.5%) deceased died in their city of usual residence, and a slightly higher proportion of women (24%) than men (17%) died somewhere other than their usual city of residence (P = 0.06). This finding, however, was not significant at the P < 0.05 criterion. Age was significantly associated with place of death, and patients who died at home were older (mean age: 75.7 years) than those who died in hospitals (mean age: 71.1 years; P ≤ 0.001). This association held after adjustment for sex. Patients who died in their city of usual residence were more likely to die at home than those who died in another city (P ≤ 0.001). Patients who lived in larger cities (100,000 or more residents) were significantly more likely to die in a hospital (P ≤ 0.001). The association between living in a larger city and dying in a hospital held after adjustment for age.
Eighty-nine percent responded to a question about health care coverage, and 13.8% reported no affiliation to a source of health care, such as an institution or health insurance company. Details of the institutions and companies providing coverage are shown in the footnote of Table 1. Health care coverage was significantly associated with the place of death. Among those without health care coverage, the proportion of home deaths was higher than the proportion of hospital deaths, 74.1% vs. 25.9% (P ≤ 0.001). Other demographic factors were not associated with the place of death (Table 1).
Clinical Factors
We also examined the association between medical conditions assessed by a physician during the last 12 months of life and place of death (Table 2). We found that patients who had a history of diabetes or heart attack were more likely to die in a hospital than were those without a history of diabetes (P ≤ 0.001) or heart attack (P = .04). Both associations held after adjustment for age. A higher proportion of patients with a history of cancer (22.6%) than of those without a history of cancer (16.3%) died at home (P = 0.09). After adjustment for age, this difference approached but did not reach significance (P = 0.05).
Table 2.
Medical Conditions and Symptoms in the Last 12 Months of Life Associated with the Place of Death of Participants in the MHAS Survey
| No. Deceased (%) by Place of Death |
||||
|---|---|---|---|---|
| Health Conditionsa | Deceased, n (%) | Hospital, n (%) | Home, n (%) | P-value |
| Hypertension | 231 (50.0) | 117 (52.5) | 114 (47.8) | 0.30 |
| Diabetes | 146 (31.1) | 87 (39.2) | 59 (23.8) | ≤0.001 |
| Cancer | 92 (19.6) | 36 (16.3) | 56 (22.6) | 0.09 |
| Respiratory illness | 79 (16.8) | 38 (17.2) | 41 (16.5) | 0.83 |
| Heart attack | 88 (18.7) | 50 (22.5) | 38 (15.3) | 0.04 |
| Stroke | 55 (11.6) | 30 (13.5) | 25 (10.0) | 0.24 |
| Fall | 193 (41) | 94 (42.3) | 99 (39.8) | 0.57 |
| Physical pain | 276 (58.4) | 131 (58.7) | 145 (58.9) | 0.97 |
Health conditions and symptoms were not mutually exclusive, and participants may have reported more than one.
More than half of the respondents reported that the deceased had experienced frequent physical pain during the last year of life, and 57% rated the pain as severe. Pain, however, was not significantly associated with place of death. All of the deceased had received help for ADLs (score >0). For the majority (61%), the deceased's spouse was the person who provided assistance.
Utilization and Expenditures for Health Care
Results of the bivariate analysis of the association between the utilization of health services and the direct nonmedical costs for health care incurred by the deceased or family members by the place of death are presented in Table 3. We found no association between the mean number of overnight hospital stays during the last year of life and place of death. However, older patients were less likely to stay in the hospital than younger ones (P ≤ 0.01).
Table 3.
The Utilization of Health Services and Expenditures for Care During the Last Year of Life by Place of Death
| No. Deceased (%) by Place of Death |
|||
|---|---|---|---|
| Utilization and Expenditures | Hospital, n (%) | Home, n (%) | P-value |
| Total | 223 (47.1) | 250 (52.9) | NAa |
| Utilization of health services | |||
| Stayed overnight in a hospital | ≤0.001 | ||
| Yes | 207 (92.8) | 157 (62.8) | |
| No | 16 (7.2) | 93 (37.2) | |
| Visited a doctor | 0.63 | ||
| Yes | 193 (86.5) | 213 (85.2) | |
| No | 13 (5.8) | 20 (8.0) | |
| Unknown | 17 (7.6) | 17 (6.8) | |
| Expenditures for utilization of health services (only includes cases who stayed at least one night in the hospital and/or paid for doctor visits) | |||
| Total included | 207 (92.8) | 157 (62.8) | |
| Paid for overnight hospital staysb | ≤0.01 | ||
| Yes | 44 (21.3) | 54 (34.4) | |
| No | 141 (68.1) | 80 (51.0) | |
| Unknown | 22 (10.6) | 23 (14.6) | |
| Mean amount paid for hospital stay for those who reported an overnight stay (median) | 24,650.00c (8000) | 27,855.00c (5900) | 0.74d |
| Total included | 193 (86.5) | 213 (85.2) | |
| Paid for doctor visitse | ≤0.01 | ||
| Yes | 69 (35.8) | 104 (48.8) | |
| No | 101 (52.3) | 77 (36.2) | |
| Unknown | 23 (11.9) | 32 (15.0) | |
| Mean amount paid for doctor visits (median) | 10,128.80c (3100) | 14,805.90c (2000) | 0.56d |
Percentages may not add to 100 because of rounding.
Not applicable.
Includes only cases who reported at least one overnight hospital stay.
Mexican pesos 2003. The exchange rate of the Mexican peso to the U.S. dollar in June 2003 was estimated at 10.53.
Mann-Whitney test.
Includes only cases who reported at least one doctor visit.
Three hundred sixty-four (77.0%) deceased patients stayed at least one night in a hospital during their last year of life. Among those who stayed in a hospital, the mean length of the stay was 18.3 nights and the median was eight nights (range: 1–365 nights). Ninety-eight (20.7%) of the deceased reported direct nonmedical costs to the patient or family for using hospitals, and the mean total direct nonmedical cost of hospitalization during the last year of life was 26,416.12 Mexican pesos (median: 6400 Mexican pesos; range: 100–450,000). Most of the deceased (86.0%) visited a doctor during their last year of life. The mean number of doctor visits was 15.2 (median: 10; range: 1–166), and no significant difference was observed in the mean number of doctor visits by place of death. Among those who visited a doctor, 173 of the deceased (36.6%) had to pay for the visits. The mean total direct nonmedical cost incurred by the deceased or the family for visits to a doctor during the last year of life was 12,956.02 Mexican pesos (median: 3000; range: 4–594,000). According to respondents, a family member or other person paid the health expenditures of 49.4% of the deceased, while the expenditures were covered by the deceased or a spouse for 14.0% of the deceased. Slightly more than one-third (35.5%) of the deceased did not report direct nonmedical costs, and only four respondents informed that they did not know about who had paid for the direct nonmedical costs of the deceased.
Included in the first multivariate logistic regression model were the age at death, marital status, years of education, whether death occurred in the city of usual residence, population size of city of residence, cause of death, whether the deceased stayed overnight in a hospital during the last year of life, and health care coverage. To avoid collinearity between covariates, we excluded from the model variables assessing a history of diabetes, cancer, and heart attack because those variables were significantly associated with the cause of death variable.
Results of this multivariate analysis are provided in Table 4. Compared with patients who died at home, those who died in a hospital were more likely to die someplace other than their city of usual residence (odds ratio [OR]: 4.68, 95% confidence interval [CI]: 2.56, 8.57) and had spent at least one night at a hospital during the last year of life (OR: 6.73, 95% CI: 3.29, 13.78). Factors significantly associated with dying at home were older age (OR: 0.97, 95% CI: 0.95, 0.99), residing in a city of less than 100,000 inhabitants (OR: 0.41, 95% CI: 0.24, 0.70), and not having health care coverage (OR: 0.36, 95% CI: 0.17, 0.75).
Table 4.
Multivariate Logistic Regression Model of the Factors Associated with Death in a Hospital of Deceased Participant in the MHAS
| Covariates | Estimate (B) | Wald Chi-Square | P-value | OR (95% CI) |
|---|---|---|---|---|
| Intercept | –0.762 | 0.625 | 0.43 | 0.47 |
| Demographic and geographic factors | ||||
| Age | –0.030 | 8.151 | ≤0.01 | 0.97 (0.95, 0.99) |
| Married or in a married-like situation | –0.045 | 0.240 | 0.85 | 0.96 (0.60, 1.53) |
| Years of schooling | –0.035 | 1.195 | 0.27 | 0.97 (0.91, 1.03) |
| Dying in a city other than the city of usual residency | 1.544 | 25.039 | ≤0.001 | 4.68 (2.56, 8.57) |
| Living in a city of less than 100,000 residents | –0.899 | 10.590 | ≤0.01 | 0.41 (0.24, 0.70) |
| Clinical factors | ||||
| Cause of death | 5.800 | 0.22 | ||
| Cancer | –0.398 | 1.614 | 0.20 | 0.67 (0.36, 1.24) |
| Diabetes | 0.012 | 0.001 | 0.97 | 1.01 (0.52, 1.98) |
| Stroke | 0.471 | 1.206 | 0.27 | 1.60 (0.69, 3.72) |
| Cardiovascular | 0.381 | 1.303 | 0.25 | 1.46 (0.76, 2.81) |
| Other | Reference | |||
| Access to health care | ||||
| No health care coverage | –1.016 | 7.377 | ≤0.01 | 0.36 (0.17, 0.75) |
| At least one overnight hospital staya | 1.906 | 27.165 | ≤0.001 | 6.73 (3.29, 13.78) |
Hosmer and Lemeshow Chi-square test, 7.99; df, 8; P-value, 0.43; Nagelkerke R-squared, 0.31.
Hospital stays during the last year of life.
The second logistic regression model constructed to determine the influence of health services expenditures (direct nonmedical costs) on place of death included the cases that used health care services in their last year of life. In this model, we included covariates from the first model and added dichotomous covariates evaluating if the deceased had paid for hospital stays (yes/no) or had paid for doctors’ visits (yes/no) during the last year of life. The independent predictors of hospital deaths were dying of stroke (OR: 4.17, 95% CI: 1.17, 14.90) and dying someplace other than their city of usual residence (OR: 3.94, 95% CI: 1.85, 8.43). The factors associated with home death were old age (OR: 0.97, 95% CI: 0.95, 0.99), dying in a city of less than 100,000 inhabitants (OR: 0.48, 95% CI: 0.24, 0.98), and having paid for hospital stays during the last year of life (OR: 0.24, 95% CI: 0.10, 0.59). Cancer as the cause of death was marginally associated with home deaths (P = 0.06). The goodness of fit measured by the Hosmer and Lemeshow test was a Chi-square value of 6.73, degrees of freedom = 8, and P = 0.57. The Nagelkerke R-squared was 0.24.
Discussion
In this sample of older Mexicans, we identified measures of access to and availability of health services, and a series of clinical, demographic, and geographic factors that influenced the place of death. Studies examining site of death have largely been limited to specific patient populations and institutions.7,9 Importantly, this is the first large-scale national study to investigate the factors that influence the site of death in a national representative sample of older Mexicans who died from multiple causes. Our finding that approximately 53% of older Mexican adults die at home is similar to results from a previous study examining the factors associated with place of death of cancer patients in the Mexico City metropolitan area, which found that 54% of cancer patients in the Mexico City area died at home.18
Geographic Factors and Access and Availability of Health Services
Consistent with our theoretical model, our findings suggest that place of death is reflective of the utilization and availability of health services at the end of life. It is significant that the three strongest predictors of hospital deaths were measures of accessibility and availability of health care services: (1) spending at least one night in the hospital during the last year of life, (2) dying in a city other than the city of usual residence, and (3) residing in a city of more than 100,000 inhabitants. Conversely, lack of health care coverage was a robust determinant of dying at home. Our sample was taken from a large sample established with census methodology, and rural and urban areas were well represented.
The strongest predictor of hospital deaths in our first model, spending time in a hospital in the last year of life, confirms findings from previous studies from other parts of the world.36 Our results confirm results of studies observing increased rates of hospital deaths in regions with greater hospital bed availability as well.12,16 Thus, the predictive influences of hospital stays, urban residency, health care coverage, and traveling to another city to obtain health care on place of death strongly indicate that home health care in Mexico is not readily available for most. This conclusion is corroborated by a largely urban survey of advanced cancer care clinicians in Latin America28 that revealed very low rates of professional home care in Mexico. Moreover, compared with residents of urban areas, terminally ill patients in small communities probably have even less access to professional home care. Our finding that Mexicans from smaller, mainly rural, areas were 2.44 times more likely to die at home than those living in urban areas confirms the findings of studies from other parts of the world. Studies in China,37 Belgium,38 Italy, and Spain7 showed that patients who died at home were more likely to live in rural areas or less developed communities than patients who died in hospitals.
In the group of participants who used health services such as hospital stays or physician visits, we found that persons who incurred direct nonmedical costs during the last year of life were more than four times more likely to die at home than those who had not incurred such costs. Research suggests that the quality and extent of health services offered by various health institutions and insurance companies vary in Mexico across geographic regions, as evidenced by the disparity in health outcomes, as well as access to care. The result is a system characterized by low levels of public spending in health care and a high burden of out-of-pocket charges to the population.39 The burden of charges increases when coverage is incomplete and must be supplemented by private providers paid completely by the patient or family. Conclusions drawn from findings from developed nations regarding the place of death cannot be generalized to developing nations such as Mexico. In China, for instance, Gu et al.37 described a similar finding from a study of older Chinese adults in a population-based health survey in which those with resources (i.e., those with a combination of receiving a pension, public, or collective free medical services) were less likely to die at home. We hypothesize that, in our study, the group of patients who died at home and who had paid for hospital stays in the last year of life had exhausted their financial resources and did not have adequate access to end-of-life services because home-based health services are at an early stage of development in Mexico.
A survey to assess preferences related to place of death has never been conducted in Mexico. The evidence from the developing nations strongly suggests that most people, if presented with options, prefer to die at home. However, in developing nations such as Mexico, end-of-life care options are primarily limited to either hospital care (for those with resources) or spending the last period of life at home, and dying at home, without receiving professional home care. Yet, we still do not know, if presented with more comprehensive options, where Mexicans would prefer to die. In addition, the direct nonmedical costs for utilization of health services to the deceased or their families could have included a wide array of charges, such as out-of-pocket payments for co-payments and deductibles, payments to supplement health care not covered by the providers (either institutions or private insurances), or hospital expenditures because of self-coverage.
Clinical Factors
The cause of death has been associated with the place of death, and this study supports previous observations that deaths from stroke are more frequent in hospitals.38 Deaths resulting from an acute onset and rapid disease progression, such as stroke, may require different approaches to end-of-life care than other causes of death. Thus, patients who suffer a stroke may be rushed to the hospital after sudden presentation of symptoms, and many stroke patients are still receiving initial and follow-up care in the hospital when they die.
Patients with cancer, on the other hand, may be prone to die at home because of the chronic and sometimes slow progression of this disease. Although only marginally associated with home deaths in the final model, our findings suggest that persons with cancer in Mexico (59% of cancer cases) are more likely to die at home than those dying from other causes. This finding also confirms a previous study in which 59% of Mexican clinicians who care for patients with advanced cancer reported that most of their patients died at home.28 Identifying what types of patients die at home vs. hospital should be accounted for when planning and developing palliative care services in the multiple settings in which they die.
The large proportion of respondents in our study who indicated that their deceased relative had complained of frequent physical pain during the last 12 months of life (more than 50%, and 57% of those reported the pain as severe) supports the need for improved palliative care across the system—both in hospitals and at home. Symptom control is clearly an important factor that may affect not only how end-of-life care is delivered but also the place where death occurs; thus, more research in this area is warranted.12 Evidence from a recent systematic review, as well as a national U.S. study on where people die, suggests that functional decline prominently predicts dying at home.7,9 In our study, we found no association between the functional status measured by the need of help for ADLs and the place of death. A limitation of our study is that need of help for ADLs was collected as a categorical variable measuring if help was needed for any ADLs vs. not. Further studies, preferably using more sensitive measures and prospective designs, would be important to understand the association between this clinical variable and place of death in the context of Mexico.
Demographic and Individual Factors
Numerous studies have found significant associations between age and place of death. These studies, however, emanated largely from developed nations and have yielded very mixed results.7,36 Older age in this study was an independent determinant of dying at home. This finding confirms previous study results examining the factors associated with place of death of cancer patients in Mexico City.18 These findings may reflect patient and/or family preferences for less aggressive treatment near the end of life. More research is needed in the area of end-of-life decision making that addresses the greater value placed on family roles in decision making in Mexican culture.40
Most studies on place of death have concluded that most terminally ill patients die at home.7,8,10,12,41 However, most studies evaluating preferences for place of death have been conducted in developed nations with more matured and integrated palliative care programs. Unfortunately, information about the patients’ or families’ preference for the place of death was not available from the MHAS data set, and we were unable to determine whether patients died in their setting of choice. Accurately assessing and respecting the preferences for the place of death as well as the personal decisions about terminal care is paramount for achieving quality end-of-life care. Understanding the relationship between preferences and what actually occurs when Mexicans die is an important area for further research.
This study had several limitations. Information about the deceased was retrospectively obtained from proxy respondents. However, proxy respondents have been used successfully as informants in several studies of older adults and end-of-life care.42–46 Although we were limited to the items included in the MHAS, we were able to draw important conclusions regarding the predictors of place of death in a national representative sample of older Mexicans.
The study identified disparities regarding end-of-life care potentially experienced by older Mexicans without access to health services. Decision makers and health planners could use these results to characterize the population at risk of dying at home or in the hospital, identify the needs of the terminally ill according to their place of death, and inform the allocation of future palliative care programs. Hospital-based services would be more likely to be located in urban communities, would care for patients who could be referred from smaller clinics to regional or specialized hospitals, and provide the care for stroke victims. Home-based services could be located in small communities and provide care for the patients not affiliated with health care institutions, those dying after discharge from a hospital, those having paid for hospital stays, or patients dying of cancer.
In developing countries such as Mexico, the population is aging while family structures and arrangements that historically provided the informal safety net for the ill and elderly are changing, and socioeconomic and health care support for older persons is waning.47 Because developing nations with accelerating aging patterns have less time to adapt to the needs of their aging populations than developed nations, it is imperative that they start planning for the needs of the older segments of their populations now.
Researchers and decision makers in developing nations should be alert to the forthcoming challenges associated with the care of older people. Future health and aging surveys in Mexico should collect details on the satisfaction with health services received and preferences related to end-of-life home and hospital care. Further research including caregivers and families in the Mexican context is needed to inform the development of cost-effective community-based programs and develop policies to reduce suffering and improve the quality of care at the end of life. These relevant topics must be evaluated to provide accessible affordable quality health care to older and terminally ill Mexicans.
Acknowledgments
Dr. Isabel Torres-Vigil was supported in part by the National Cancer Institute (3R01CA12229203S1). The authors wish to thank John Le Bas and Allison De la Rosa for their editorial assistance in completing this article.
Footnotes
Disclosures
The authors declare no conflicts of interest.
References
- 1.Davies E, Higginson IJ, editors. Better palliative care for older people. World Health Organization Regional Office for Europe; Copenhagen, Denmark: 2004. [April 4, 2010]. Available from http://www.euro.who.int/document/E82933.pdf. [Google Scholar]
- 2.Wenk R, Bertolino M. Palliative care development in South America: a focus on Argentina. J Pain Symptom Manage. 2007;33:645–650. doi: 10.1016/j.jpainsymman.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Torres Vigil I, Aday LA, De Lima L, Cleeland CS. What predicts the quality of advanced cancer care in Latin America? A look at five countries: Argentina, Brazil, Cuba, Mexico, and Peru. J Pain Symptom Manage. 2007;34:315–327. doi: 10.1016/j.jpainsymman.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Wenk R, Ochoa J. Argentina: status of cancer pain and palliative care. J Pain Symptom Manage. 1996;12:97–98. doi: 10.1016/0885-3924(96)00079-6. [DOI] [PubMed] [Google Scholar]
- 5.De Lima L, Bruera E, Joranson DE, et al. Opioid availability in Latin America: the Santo Domingo report progress since the Declaration of Florianopolis. J Pain Symptom Manage. 1997;13:213–219. doi: 10.1016/s0885-3924(96)00325-9. [DOI] [PubMed] [Google Scholar]
- 6.Sepulveda C, Marlin A, Yoshida T, Ullrich A. Palliative care: the World Health Organization's global perspective. J Pain Symptom Manage. 2002;24:91–96. doi: 10.1016/s0885-3924(02)00440-2. [DOI] [PubMed] [Google Scholar]
- 7.Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ. 2006;332:515–521. doi: 10.1136/bmj.38740.614954.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cardenas-Turanzas M, Grimes RM, Bruera E, Quill B, Tortolero-Luna G. Clinical, sociodemo-graphic, and local system factors associated with a hospital death among cancer patients. Support Care Cancer. 2006;14:71–77. doi: 10.1007/s00520-005-0819-2. [DOI] [PubMed] [Google Scholar]
- 9.Weitzen S, Teno JM, Fennell M, Mor V. Factors associated with site of death: a national study of where people die. Med Care. 2003;41:323–335. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- 10.Emanuel L, Von Gunten C, Ferris F. Gaps in end-of-life care. Arch Fam Med. 2000;10:1176–1180. doi: 10.1001/archfami.9.10.1176. [DOI] [PubMed] [Google Scholar]
- 11.Karlsen S, Addington-Hall J. How do cancer patients who die at home differ from those who die elsewhere? Palliat Med. 1998;12:279–286. doi: 10.1191/026921698673427657. [DOI] [PubMed] [Google Scholar]
- 12.Bruera E, Sweeney C, Russell N, Willey JS, Palmer JL. Place of death of Houston area residents with cancer over a two-year period. J Pain Symptom Manage. 2003;26:637–643. doi: 10.1016/s0885-3924(03)00204-5. [DOI] [PubMed] [Google Scholar]
- 13.Bruera E, Russell N, Sweeney C, Fisch M, Palmer JL. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol. 2002;20:2127–2133. doi: 10.1200/JCO.2002.08.138. [DOI] [PubMed] [Google Scholar]
- 14.McGregor MJ, Tate RB, Ronald LA, McGrail KM. Variation in site of death among nursing home residents in British Columbia, Canada. J Palliat Med. 2007;10:1128–1136. doi: 10.1089/jpm.2007.0018. [DOI] [PubMed] [Google Scholar]
- 15.Bruera E, Neumann CM, Gagnon B, et al. Edmonton Regional Palliative Care Program: impact on patterns of terminal cancer care. CMAJ. 1999;161:290–293. [PMC free article] [PubMed] [Google Scholar]
- 16.Pritchard R, Fisher E, Teno J, et al. Influence of patient preferences and local health system characteristics on the place of death. J Am Geriatr Soc. 1998;46:1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- 17.Center for Gerontology and Health Care Research Facts on dying: policy relevant data on care at the end of life. [April 19, 2010];Brown atlas of dying. Available from http://www.chcr.brown.edu/dying/brownat las.htm.
- 18.Cardenas-Turanzas M, Carrillo MT, Tovalin-Ahumada H, Elting L. Factors associated with place of death of cancer patients in the Mexico City Metropolitan area. Support Care Cancer. 2007;15:243–249. doi: 10.1007/s00520-006-0152-4. [DOI] [PubMed] [Google Scholar]
- 19.Verastegui E, Mohar A. Colorectal cancer in Mexico: should a middle income country invest in screening or in treatment? Eur J Health Econ. 2010;10:S107–S114. doi: 10.1007/s10198-009-0190-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. [April 15, 2010];Population Division of the Department of Economic and Social Affairs of the United Nations Secretariat. World population prospects: the 2008 revision population database. Available from http://esa.un.org/unpp.
- 21.Omran AR. The epidemiologic transition: a theory of the epidemiology of population change. Milbank Q. 1971;49:509–538. [PubMed] [Google Scholar]
- 22.Li RM, Iadarola AC, Malsano CC. Why population aging matters: A global perspective. National Institute on Aging. Available from http://www.nia.nih.gov/researchinformation/extramuralprograms/behavioralandsocialresearch/globalaging.htm. [Google Scholar]
- 23.Stevens G, Dias RH, Thomas KJ, et al. Characterizing the epidemiological transition in Mexico: national and subnational burden of diseases, injuries, and risk factors. PLoS Med. 2008;5:e125. doi: 10.1371/journal.pmed.0050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torres I, Lopez-Zetina J. Morbidity and mortality trends in developed and developing countries. In: Bruera E, Wenk R, editors. Palliative care in the developing world: Principles and practice. The International Association for Hospice and Palliative Care (IAHPC) Press; Houston, TX: 2004. pp. 11–21. [Google Scholar]
- 25.World Health Organization [April 13, 2010];Health situation analysis and trends summary 2007. Available from http://www.paho.org/English/DD/AIS/cp_484.htm.
- 26.Allende S, Carvell HC. Mexico: status of cancer pain and palliative care. J Pain Symptom Manage. 1996;12:121–123. doi: 10.1016/0885-3924(96)00093-0. [DOI] [PubMed] [Google Scholar]
- 27.Montejo-Rosas G, Galaviz-Muro A, Espinoza-Rodriguez LN, Cortez-Gutierrez L. Vol. 138. Gac Med Mex; 2002. Palliative care in advanced cancer. A 7-year experience at the Dr. Juan I. Menchaca Civil Hospital of Guadalajara, Jalisco, Mexico. [in Spanish]. pp. 231–234. [PubMed] [Google Scholar]
- 28.Torres-Vigil I, Aday LA, Reyes-Gibby C, et al. Health care providers’ assessments of the quality of advanced-cancer care in Latin American medical institutions: a comparison of predictors in five countries: Argentina, Brazil, Cuba, Mexico, and Peru. J Pain Palliat Care Pharmacother. 2008;22:7–20. doi: 10.1080/15360280801989195. [DOI] [PubMed] [Google Scholar]
- 29.Phillips KA, Morrison KR, Andersen R, Aday LA. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–596. [PMC free article] [PubMed] [Google Scholar]
- 30.Palloni A, Soldo B, Wong R. Health status in a national sample of elderly Mexicans. Center for Demography and Ecology, University of Wisconsin; Madison, WI: 2003. [Google Scholar]
- 31.Wong R, Espinoza M, Palloni A. Mexican older adults with a wide socioeconomic perspective: health and aging. [in Spanish]. Salud Publica Mex. 2007;49:S436–S447. doi: 10.1590/s0036-36342007001000002. [DOI] [PubMed] [Google Scholar]
- 32.Pagan JA, Puig A, Soldo BJ. Health insurance coverage and the use of preventive services by Mexican adults. Health Econ. 2007;16:1359–1369. doi: 10.1002/hec.1226. [DOI] [PubMed] [Google Scholar]
- 33.Wong R. Follow-up master file for the Mexican Health and Aging Study (MHAS/ENASEM) 2001-2003. Maryland Population Research Center, University of Maryland; College Park, MD: 2004. [November 30, 2010]. Available from http://www.mhas.pop.upenn.edu/english/documents/Tracker/Follow_Up-Master-File.pdf. [Google Scholar]
- 34.Cantor SB, Levy LB, Cárdenas-Turanzas M, et al. Collecting direct non-health care and time cost data: application to screening and diagnosis of cervical cancer. Med Decis Making. 2006;26:265–272. doi: 10.1177/027298906288679. [DOI] [PubMed] [Google Scholar]
- 35.Lock A, Higginson I. Patterns and predictors of place of cancer death for the oldest old. BMC Palliat Care. 2005;4:6. doi: 10.1186/1472-684X-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grande GE, Addington-Hall JM, Todd CJ. Place of death and access to home care services: are certain patient groups at a disadvantage? Soc Sci Med. 1998;47:565–579. doi: 10.1016/s0277-9536(98)00115-4. [DOI] [PubMed] [Google Scholar]
- 37.Gu D, Liu G, Vlosky D, Yi Z. Factors associated with place of death among the Chinese oldest old. J Appl Gerontol. 2007;26:34–57. [Google Scholar]
- 38.Cohen J, Bilsen J, Hooft P, et al. Dying at home or in an institution using death certificates to explore the factors associated with place of death. Health Policy. 2006;78:319–329. doi: 10.1016/j.healthpol.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 39.Oxley H. Health policy . Getting it right. OECD perspectives in policy challenges in Mexico. Organisation for Economic Co-Operation and Development; Paris, France: 2007. [July 22, 2010]. Available from http://www.oecd.org/dataoecd/12/27/38136757.pdf. [Google Scholar]
- 40.Talamantes MA, Cornell J, Espino DV, Lichtenstein MJ, Hazuda HP. SES and ethnic differences in perceived caregiver availability among young-old Mexican Americans and non-Hispanic whites. Gerontologist. 1996;36:88–99. doi: 10.1093/geront/36.1.88. [DOI] [PubMed] [Google Scholar]
- 41.Gruneir A, Mor V, Weitzen S, et al. Where people die: a multilevel approach to understanding influences on site of death in America. Med Care Res Rev. 2007;64:351–378. doi: 10.1177/1077558707301810. [DOI] [PubMed] [Google Scholar]
- 42.Ellis BH, Bannister WM, Cox JK, et al. Utilization of the propensity score method: an exploratory comparison of proxy-completed to self-completed responses in the Medicare Health Outcomes Survey. Health Qual Life Outcomes. 2003;1:1–47. doi: 10.1186/1477-7525-1-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iezzoni LI, Davis RB, Soukup J, O'Day B. Satisfaction with quality and access to health care among people with disabling conditions. Int J Qual Health Care. 2002;14:369–381. doi: 10.1093/intqhc/14.5.369. [DOI] [PubMed] [Google Scholar]
- 44.Lynn J, Knaus WA. Background for SUPPORT. J Clin Epidemiol. 1990;43:S1–S4. doi: 10.1016/0895-4356(90)90211-7. [DOI] [PubMed] [Google Scholar]
- 45.Kreling B, Robinson DK, Bergner M. Data collection strategies in SUPPORT. J Clin Epidemiol. 1990;43:S5–S9. doi: 10.1016/0895-4356(90)90212-8. [DOI] [PubMed] [Google Scholar]
- 46.Murphy DJ, Knaus WA, Lynn J. Study population in SUPPORT: patients (as defined by disease categories and mortality projections), surrogates, and physicians. J Clin Epidemiol. 1990;43:S11–S28. doi: 10.1016/0895-4356(90)90213-9. [DOI] [PubMed] [Google Scholar]
- 47.Palloni A, Pinto-Aguirre G, Pelaez M. Demographic and health conditions of ageing in Latin America and the Caribbean. Int J Epidemiol. 2002;31:762–771. doi: 10.1093/ije/31.4.762. [DOI] [PubMed] [Google Scholar]