Abstract
We investigated the role of nuclear factor erythroid 2–related factor 2 (Nrf2) in renin-angiotensin system (RAS) gene expression in renal proximal tubule cells (RPTCs) and in the development of systemic hypertension and kidney injury in diabetic Akita mice. We used adult male Akita Nrf2 knockout mice and Akita mice treated with trigonelline (an Nrf2 inhibitor) or oltipraz (an Nrf2 activator). We also examined rat immortalized RPTCs (IRPTCs) stably transfected with control plasmids or plasmids containing rat angiotensinogen (Agt), angiotensin-converting enzyme (ACE), angiotensin-converting enzyme-2 (Ace2), or angiotensin 1-7 (Ang 1-7) receptor (MasR) gene promoters. Genetic deletion of Nrf2 or pharmacological inhibition of Nrf2 in Akita mice attenuated hypertension, renal injury, tubulointerstitial fibrosis, and the urinary albumin/creatinine ratio. Furthermore, loss of Nrf2 upregulated RPTC Ace2 and MasR expression, increased urinary Ang 1-7 levels, and downregulated expression of Agt, ACE, and profibrotic genes in Akita mice. In cultured IRPTCs, Nrf2 small interfering RNA transfection or trigonelline treatment prevented high glucose stimulation of Nrf2 nuclear translocation, Agt, and ACE transcription with augmentation of Ace2 and MasR transcription, which was reversed by oltipraz. These data identify a mechanism, Nrf2-mediated stimulation of intrarenal RAS gene expression, by which chronic hyperglycemia induces hypertension and renal injury in diabetes.
New insights into Nrf2 stimulation of intrarenal RAS activation and hypertension development in diabetes.
Nuclear factor erythroid 2–related factor 2 (Nrf2) functions as a master regulator of redox balance in cellular cytoprotective responses (1). Under baseline conditions, Nrf2 is sequestered in the cytoplasm, stabilized by Kelch-like ECH-associated protein 1 (Keap1), and rapidly degraded by proteasomes. In the presence of oxidative stress, Nrf2 is released from Keap1, translocates to the nucleus, and forms heterodimers with small musculoaponeurotic fibrosarcoma proteins, which bind to the antioxidant response element (RE) in the promoters of various genes, including antioxidant and detoxifying genes, and enhances their expression (1–3). Although Nrf2 is abundantly expressed in nondiabetic and diabetic kidneys (4–6), its physiological role in the kidneys is undefined.
Studies in rodents with the Nrf2 activators bardoxolone methyl (BM) analogues RTA 405 and dh404 have yielded conflicting results. BM analogues were reported to exert potent antidiabetic effects in mice with diet-induced diabetes and in rodent models of type 2 diabetes (T2D) and obesity (7, 8). Others found that BM analogues increased albuminuria and blood pressure along with weight loss in Zucker diabetic fatty rats (9) and, at high doses, worsened diabetes-associated atherosclerosis and kidney disease in diabetic apoE−/− mice (10). A phase 2 clinical trial with BM in human T2D with stage 3b or 4 chronic kidney disease reported reductions of serum creatinine levels and slight increases of estimated glomerular filtration rate (GFR) (11), suggesting a renoprotective action. However, phase 3 clinical trials with BM involving patients with T2D and stage 4 (advanced) diabetic kidney disease were discontinued after 9 months of follow-up because of increased mortality and heart failure rates, as well as development of hypertension and albuminuria without favorable effects on the GFR (12). Thus, whether Nrf2 activation is beneficial in patients with diabetes and kidney disease remains to be investigated. Currently, three phase 2/3 clinical trials are under way to test the safety and efficacy of BM.
We reported previously that catalase (Cat) overexpression, specifically in renal proximal tubule cells (RPTCs), curbed systemic hypertension and RPTC apoptosis (13–15) and prevented oxidative stress and Nrf2 stimulation of angiotensinogen (Agt) gene transcription in diabetic Akita Cat-transgenic (Tg) mice (5), indicating that Nrf2 stimulation of intrarenal Agt gene expression contributes to the development of systemic hypertension and nephropathy in diabetes. However, little information is available as to whether Nrf2 affects the expression of other renin-angiotensin system (RAS) components, including angiotensin-converting enzyme (ACE), angiotensin-converting enzyme-2 (Ace2), and angiotensin 1-7 receptor (MasR) in diabetic RPTCs, which may be crucial in the development of hypertension and nephropathy in diabetes.
In the current study, we investigated the relationship between Nrf2 and intrarenal RAS gene expression, systemic hypertension and renal injury in Akita mice, a murine model of type 1 diabetes mellitus, and in RPTCs cultured in a high-glucose (HG) milieu.
Materials and Methods
Chemicals and constructs
d-glucose, d-mannitol, the alkaloid trigonelline (C7H7NO2, an Nrf2 inhibitor), and oltipraz (an Nrf2 activator) were purchased from Sigma-Aldrich Canada Ltd. (Oakville, ON, Canada). Normal glucose (NG; 5 mmol/L d-glucose)–Dulbecco’s modified Eagle medium (DMEM; Catalog No. 12320), penicillin/streptomycin, and fetal bovine serum were procured from Invitrogen, Inc. (Burlington, ON, Canada).
The antibodies used in the current study are listed in Table 1. pGL4.20 vector containing luciferase reporter was obtained from Promega (Sunnyvale, CA). pGL4.20 containing rat Agt gene promoter (N-1495/N+18) and rat Ace2 gene promoter (N-1091/+83) has been described previously (17, 18). The rat ACE gene promoter (N-1675/+95) and the rat MasR gene promoter (N-1811/+100) were cloned from rat genomic DNA with specific primers (Table 2) and then inserted into pGL4.20 plasmid at Bgl II/Xho I restriction sites. Scrambled (Scr) Silencer Negative Control #1 and Nrf2 small interfering RNAs (siRNAs) were obtained from Ambion, Inc. (Austin, TX). Oligonucleotides were synthesized by Integrated DNA Technologies, Inc. (Coralville, IA). Restriction and modifying enzymes were procured from commercial sources.
Table 1.
Antibodies
| Name of Antibody | Source of Antibody | Species Raised in; Monoclonal/Polyclonal | RRID | Dilution for WB and/or IHC |
|---|---|---|---|---|
| Nrf2 | Abcam | Rabbit; polyclonal | AB_881705 | WB (1:2000); IHC (1:400) |
| NQO-1 | Santa-Cruz Biotechnology | Goat; polyclonal | AB_2154339 | WB (1:2000) |
| NQO-1 | Abcam | Mouse; monoclonal | AB_881738 | IHC (1:400) |
| Keap1 | Abcam | Rabbit; polyclonal | AB_1141055 | WB (1:2000); IHC (1:400) |
| Angiotensinogen (Agt) | Generated in our laboratory (16) | Rabbit; polyclonal | AB_2631321 | WB (1:2000); IHC (1:200) |
| ACE | Santa Cruz Biotechnology | Goat; polyclonal | AB_2273625 | WB (1:2000); IHC (1:250) |
| Ace2 | R&D Systems | Goat; polyclonal | AB_355722 | WB (1:2000); IHC (1:250) |
| MasR | Novus Biologicals | Rabbit; polyclonal | AB_11039164 | WB (1:2000); IHC (1:200) |
| β-Actin | Sigma-Aldrich | Mouse; monoclonal | AB_476744 | WB (1:20,000) |
Abbreviations: IHC, immunohistochemistry; NQO-1, NAD(P)H quinone oxidoreductase 1; RRID, Research Resource Identifier, WB, Western blotting.
Table 2.
Primer Sequences for Genotyping and RT-qPCR
| Gene (Species) | Sense and Anti-Sense Primers | Reference Sequence |
|---|---|---|
| Primers for genotyping | ||
| Ins2 (mouse) | S: TGCTGATGCCCTGGCCTGCT | NT_039437.7 |
| AS: TGGTCCCACATATGCACATG | ||
| Nrf2 (mouse genotyping) | Common-S: GCCTGAGAGCTGTAGGCCC | |
| WT-AS: GGAATGGAAAATAGCTCCTGCC | ||
| Mutant-AS: GACAGTATCGGCCTCAGGAA | ||
| Primers for RT-qPCR | ||
| Nrf2 (mouse/rat) | S: CGCCGCCTCACCTCTGCTGCCAGTAG | NM_010902.3 |
| AS: AGCTCATAATCCTTCTGTCG | ||
| Keap1 (mouse/rat) | S: CATCCACCCTAAGGTCATGGA | NM_016679.4 |
| AS: GACAGGTTGAAGAACTCCTCC | ||
| NQO-1 (mouse/rat) | S: TATCCTTCCGAGTCATCTCTAGCA | NM_008706.5 |
| AS: TCTGCAGCTTCCAGCTTCTTG | ||
| Nox4 (mouse) | S: TGGCCAACGAAGGGGTTAAA | NM_015760.4 |
| AS: GATGAGGCTGCAGTTGAGGT | ||
| Catalase (mouse) | S: CGACCAGATGAAGCAGTGGA | NM_009804.2 |
| AS: CCACTCTCTCAGGAATCCGC | ||
| Agt (mouse/rat) | S: CCACGCTCTCTGGATTTATC | NM_031144.3 |
| AS: ACAGACACCGAGATGCTGTT | ||
| ACE (mouse) | S: AGGAGTTTGCAGAGGTCTGG | NM_207624 |
| AS: GGAAGCAGACCTTGCCAGTG | ||
| ACE (rat) | S: GAGCCATCCTTCCCTTTTTC | NM_012544.1 |
| As: GGCTGCAGCTCCTGGTATAG | ||
| Ace2 (mouse) | S: AGGAGGAAGTTGATGGATACCTA | NM_027286 |
| AS: GGCTCAGTCAGCATAGAGTTT | ||
| Ace2 (rat) | S: ACAGTTCCTTTTGGGGAGGC | NM_001012006.1 |
| AS: GTGACAGGAGGCTCGTAAGG | ||
| MasR (mouse) | S: GCATTCGTCTGTGCCCTTCT | NM_008552.4 |
| AS: TTCCGTATCTTCACCACCAAGA | ||
| Tgf-β (mouse) | S: CCAAACTAAGGCTCGCCAGTC | NM_011577 |
| AS: GGCACTGCTTCCCGAATGTC | ||
| FN1 (mouse) | S: TAGCAGGCTACCGACTGACCG | NM_001276413.1 |
| AS: CACCCAGCTTGAAGCCAATCC | ||
| Col 1 (mouse) | S: ATCTCCTGGTGCTGATGGAC | NM_007742.3 |
| AS: ACCTTGTTTGCCAGGTTCAC | ||
| β-Actin (human/mouse/rat) | S: ACGATTTCCCTCTCAGCTT | NM_031144.3 |
| AS: TACAATGAGCTGCGTGTGGC |
Abbreviations: Col 1, collagen 1; FN1, fibronectin-1; Nox4, nicotinamide adenine dinucleotide phosphate oxidase 4; NQO-1, NAD(P)H quinone oxidoreductase 1; RT-qPCR, real-time quantitative polymerase chain reaction.
Generation of Akita Nrf2 knockout mice
Fertile heterozygous Akita mice with spontaneous mutation of insulin 2 (Ins2) gene (C57BL/6-Ins2Akita/J) and homozygous Nrf2−/− knockout (KO) (B6.129X1-Nef2/2tm1Ywk/J) mice were purchased from Jackson Laboratories (Bar Harbor, ME). We generated Akita Nrf2 KO mice by cross-breeding female homozygous Nrf2 KO mice with male heterozygous Akita mice [N.B.: homozygous Nrf2 KO mice are viable and fertile (4), whereas homozygous Akita mice are infertile]. Akita Nrf2 KO mice are homozygous for Nrf2 KO but heterozygous for Ins2 gene mutation.
Pathophysiology
Male adult (12-week-old) non-Akita wild-type (WT), Nrf2 KO, Akita, and Akita Nrf2 KO mice (10 per group) were studied. All animals received standard mouse chow and water ad libitum. Animal care and experimental procedures were approved by the CRCHUM Animal Care Committee.
Systolic blood pressure (SBP) level was tracked with a BP-2000 tail-cuff pressure monitor (Visitech Systems, Apex, NC) every morning, at least 2 or 3 times per week, for 8 weeks (5, 6, 14, 15, 17–23). Each animal was habituated to the procedure for at least 15 to 20 minutes per day for 5 days before the first SBP measurement. SBP values are presented as mean ± standard error of the mean of two or three determinations per week per mouse per group.
GFR was estimated with fluorescein isothiocyanate-inulin, as recommended by the Animal Models of Diabetic Complications Consortium (http://www.diacomp.org/) with slight modifications (5, 6, 17, 18).
Blood glucose (BG) levels after 4 to 5 hours of fasting were measured with the Accu-Chek Performa System (Roche Diagnostics, Laval, QC, Canada). The mice were housed individually in metabolic cages for 8 hours during the daytime before euthanasia at the age of 20 weeks. Body weight (BW) was recorded. Urine samples were collected and assayed for albumin and creatinine by albumin enzyme-linked immunosorbent assay (Albuwell and Creatinine Companion; Exocell, Inc., Philadelphia, PA) (5, 6, 17, 18).
After the animals were euthanized, the kidneys were removed, decapsulated, and weighed. Left kidneys were processed for histology and immunostaining. Right kidneys were harvested for isolation of renal proximal tubules (RPTs) by Percoll gradient (5, 6, 17, 18). Aliquots of freshly isolated RPTs from individual mice were immediately processed for total RNA and protein analyses.
In separate experiments, adult male Akita mice (age, 11 weeks) were divided into three groups (nine mice per group) and treated with 0.9% NaCl intraperitoneally or trigonelline (0.02 mg/kg/d intraperitoneally in 0.9% NaCl) from week 12 and then with or without oltipraz (150 mg/kg/d by gavage in corn oil) starting at week 14 every other day until week 17, according to published protocols including ours (5, 24, 25).
Histology
Four or five sections per kidney and three mouse kidneys per group were immunostained using the standard avidin-biotin-peroxidase complex method (ABC staining; Santa Cruz Biotechnology, Santa Cruz, CA) (5, 6, 17, 18). Tissue sections were counterstained with hematoxylin and analyzed by light microscopy by two investigators blinded to the treatments.
Oxidative stress in RPTs was assessed by dihydroethidium (DHE; Sigma) and 5-(6)-carboxy-2′,7′-dichlorodihydrofluorescein diacetate (DCFDA; Life Technologies, Burlington, ON, Canada) staining of frozen kidney sections and confirmed by standard assays of reactive oxygen species (ROS) generation (5, 6, 15, 17, 26) in isolated RPTs. Tubular luminal area, mean glomerular, and RPTC volumes were assessed, as described elsewhere (5, 6, 17, 18, 26).
Western blotting
Western blotting (WB) was performed as described previously (5, 6, 17, 18, 26). The relative densities of Nrf2, Keap1, NAD(P)H quinone oxidoreductase 1 (NQO-1), Agt, ACE, Ace2, MasR, and β-actin bands were quantified by densitometry with ImageQuant software (version 5.1; Molecular Dynamics, Sunnyvale, CA).
Real-time quantitative polymerase chain reaction
RPT Nrf2, Keap1, NQO-1, Agt, ACE, Ace2, MasR, and β-actin messenger RNA (mRNA) levels were quantified by real-time quantitative polymerase chain reaction (RT-qPCR) with forward and reverse primers (Table 2) (5, 6, 17, 18, 26).
Urinary angiotensin II and angiotensin 1-7 measurement
Urinary angiotensin II (Ang II) and angiotensin 1-7 (Ang 1-7) levels were quantified by enzyme-linked immunosorbent assay (Immuno-Biological Laboratories, Inc., Minneapolis, MN) and normalized by urinary creatinine levels, as described previously (6, 15, 17, 18, 21, 23, 26).
Cell culture
Rat immortalized renal proximal tubular cells (IRPTCs; passages 13 through 18) (27) were studied. The plasmids pGL4.20-Agt (N-1495/+18), pGL4.20-ACE (N-1675/+95), pGL4.20-Ace2 (N-1091/+83), and pGL4.20-MasR (N-1811/+100) were stably transfected into IRPTCs (17, 18).
To study the effects of HG, trigonelline, and oltipraz, IRPTCs at 75% to 85% confluency and stable transformants were synchronized overnight in serum-free DMEM containing NG (5 mmol/L d-glucose), then incubated in 5 mmol/L d-glucose plus 20 mmol/L d-mannitol or 25 mM d-glucose DMEM containing 1% depleted fetal bovine serum for 24 hours in the presence or absence of trigonelline ± oltipraz (5, 6). Agt, ACE, Ace2, and MasR mRNA levels were quantified by RT-qPCR, and corresponding Agt, ACE, Ace2, and MasR promoter activities were measured by luciferase activity assay (5, 6, 17, 18). IRPTCs stably transfected with the plasmid pGL4.20 served as controls.
In additional experiments, stable transformants were transiently transfected with Nrf2 or Scr siRNA (5, 6), and the effects of HG on Agt, ACE, Ace2, and MasR gene promoter activities were analyzed after 24 hours of incubation.
Statistical analysis
The data are expressed as mean ± standard error of the mean. Statistical comparisons were made by Student t test or one-way analysis of variance and the Bonferroni test as appropriate. P < 0.05 values were considered statistically significant.
Results
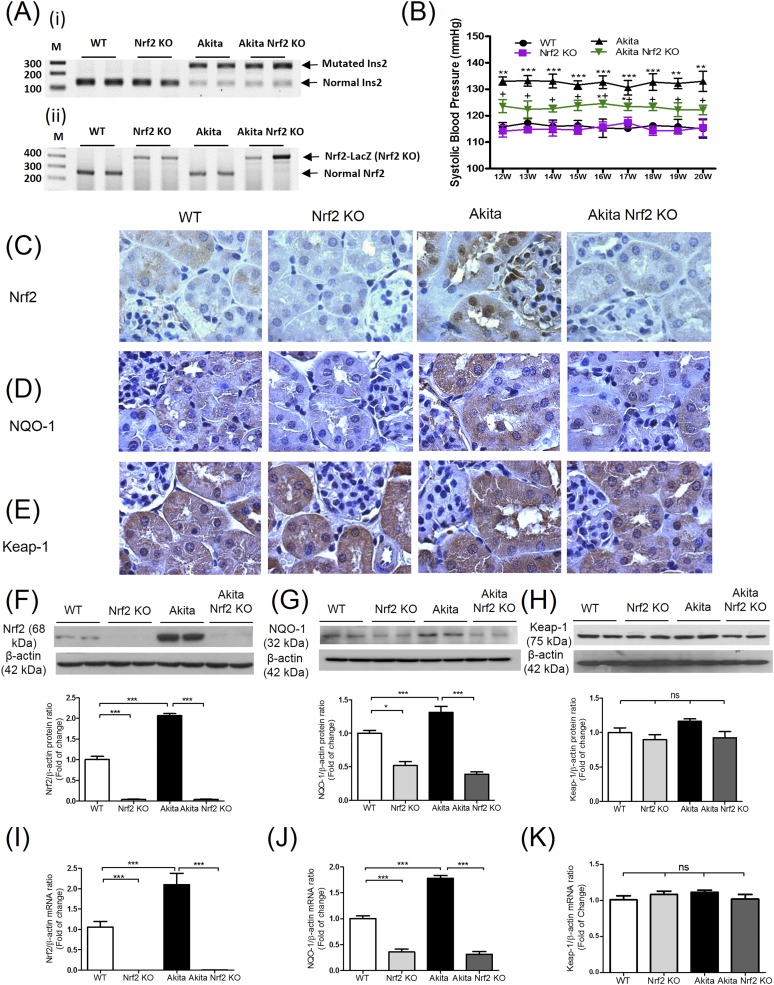
Nrf2 expression in Akita and Akita Nrf2-KO mouse kidneys
We confirmed the presence of mutated Ins2 genes in RPTs isolated from Akita and Akita Nrf2 KO mice but not in WT and Nrf2 KO mice [Fig. 1(Ai)]. The Nrf2 gene was detected in RPTs of WT and Akita mice but not in Nrf2 KO and Akita Nrf2 KO animals [Fig. 1(Aii)]. Average SBP was ∼20 mm Hg higher in Akita mice at age 12 weeks than in WT mice (P < 0.005) and remained significantly elevated for the study’s duration [Fig. 1(B); Table 3]. Genetic deletion of Nrf2 significantly decreased SBP compared with that of Akita mice. Nrf2 immunostaining was more pronounced in the nuclei of RPTCs from Akita mice than in those from WT mice and was barely detectable in Nrf2 KO and Akita Nrf2 KO mice [Fig. 1(C)]. NQO-1 expression was also higher in RPTCs from Akita mice than in those from WT mice and was markedly reduced in Nrf2 KO and Akita Nrf2 KO mice [Fig. 1(D)]. Note: NQO-1 is a member of phase II detoxifying enzymes (28), and Nrf2 binds to the antioxidant RE in the promoter of the NQO-1 gene and stimulates NQO-1 gene transcription (29). Thus, NQO-1 has been implied as a downstream mediator of the Nrf2 pathway (30). In contrast, no differences in Keap1 immunostaining were detected among the groups studied [Fig. 1(E)]. Nrf2, NQO-1, and Keap1 protein expression in RPTs assessed by WB [Fig. 1(F), 1(G), and 1(H), respectively] and their respective mRNA expression assayed with RT-qPCR (Fig. 1(I), 1(J), and 1(K), respectively) were consistent with these changes.
Figure 1.
Generation of Akita Nrf2 KO mice. (A) Genotyping of (panel i) mutated and normal Ins2 gene and (panel ii) Nrf2-LacZ (Nrf2 KO) and normal Nrf2 gene in WT, Nrf2 KO, Akita, and Akita Nrf2 KO mice by specific PCR analysis. (B) Longitudinal changes in mean SBP in male WT (●), Nrf2 KO (■), Akita (▲), and Akita Nrf2 KO (▼) mice. Values are means ± SEM; n = 10 per group. **P < 0.01 and ***P < 0.005 Akita mice compared with WT mice; +P < 0.05 and ++P < 0.01 Akita mice compared with Akita Nrf2 KO mice. (C–K) Immunohistochemical staining for (C) Nrf2, (D) NQO-1, and (E) Keap1 expression in kidney sections (magnification ×600); WB analysis of (F) Nrf2, (G) NQO-1, and (H) Keap1 protein expression and RT-qPCR analysis of (I) Nrf2, (J) NQO-1, and (K) Keap1 mRNA levels in RPTs of WT, Nrf2 KO, Akita, and Akita Nrf2 KO mice. Values are mean ± SEM; n = 6 per group. *P < 0.05; ***P < 0.005. WT (empty bars), Nrf2 KO mice (light gray bars), Akita (solid black bars), and Akita Nrf2 KO mice (dark gray bars). ns, not significant; PCR, polymerase chain reaction; SEM, standard error of the mean.
Table 3.
Physiological and Histological Measurements at Age 20 Weeks
| WT | Nrf2 KO | Akita | Akita Nrf2 KO | |
|---|---|---|---|---|
| Blood glucose, mM (n = 10) | 9.55 ± 0.53 | 11.79 ± 0.46 | 32.11 ± 0.51a | 32.32 ± 0.68a |
| Systolic blood pressure, mm Hg (n = 10) | 111.3 ± 0.71 | 115.9 ± 2.39 | 132.4 ± 2.34a | 121.4 ± 1.57b,c |
| BW, g (n = 10) | 33.08 ± 0.45 | 33.64 ± 0.81 | 23.92 ± 0.58a | 24.13 ± 0.42a |
| KW, mg (n = 10) | 339.5 ± 6.99 | 328.2 ± 9.12 | 540.0 ± 11.55a | 454.2 ± 10.76a,d |
| KW/BW, mg/g (n = 10) | 10.11 ± 0.26 | 10.02 ± 0.35 | 22.45 ± 0.89a | 17.73 ± 0.70a,d |
| TL, mm (n = 10) | 23.52 ± 0.65 | 23.3 ± 0.17 | 21.4 ± 0.27b | 21.91 ± 0.30e |
| KW/TL, mg/mm (n = 10) | 13.46 ± 0.62 | 13.69 ± 0.29 | 25.91 ± 0.84a | 20.17 ± 0.60a,d |
| GFR/BW, mL/min/g (n = 10) | 7.8 ± 0.37 | 9.03 ± 0.47 | 19.2 ± 1.56a | 18.64 ± 1.29a |
| Glomerular tuft volume,e 103 µm3 (n = 6) | 180.4 ± 4.0 | 179.0 ± 4.9 | 291.2 ± 10.28a | 237.9 ± 7.43a,d |
| Tubular luminal area, µm2 (n = 6) | 52.59 ± 2.27 | 51.5 ± 1.86 | 108.59 ± 3.13a | 87.39 ± 2.3a,d |
| RPTC volume,e 103 µm3 (n = 6) | 7.44 ± 0.57 | 7.78 ± 0.29 | 11.64 ± 0.43a | 9.99 ± 0.34a,f |
| ACR, µg/mg (n = 10) | 22.36 ± 1.71 | 25.29 ± 6.09 | 134.1 ± 19.04a | 56.98 ± 15.88c |
| Urinary Ang II/creatinine, ng/mg (n = 10) | 2.57 ± 0.37 | 1.83 ± 0.27 | 23.88 ± 2.88a | 20.08 ± 3.74a |
| Urinary Ang (1-7)/creatinine, ng/mg (n = 10) | 3.45 ± 0.62 | 3.22 ± 0.58 | 0.91 ± 0.11b | 2.58 ± 0.39f |
Abbreviations: ACR, albumin-creatinine ratio; KW, kidney weight; TL, tibial length.
P < 0.001 vs WT.
P < 0.01 vs WT.
P < 0.01 vs Akita.
P < 0.001 vs Akita.
P < 0.05 vs WT.
P < 0.05 vs Akita.
Pathophysiological measurements in mice
Table 3 reports the results of physiological measurements in WT, Nrf2 KO, Akita, and Akita Nrf2 KO mice at the age of 20 weeks. As anticipated, BG levels were significantly higher in Akita and Akita Nrf2 KO mice than in WT or Nrf2 KO mice. BG levels were similar in Akita Nrf2 KO and Akita mice. Because of the limited range of detection of the Accu-Check Performa glucose meter (up to 33.3 mmol/L), we cannot exclude the possibility that undetected differences in BG might have existed between the diabetic groups, but these were not sufficient to affect BW, whereas Akita Nrf2 KO mice exhibited significantly lower SBP than Akita mice. Although Nrf2 KO had no detectable effects on BW, it decreased, though never completely normalized, kidney weight (KW)/BW and KW/tibial length ratios, urinary albumin-creatinine ratio, glomerular tuft volume, tubule lumen area, proximal tubular cell volume, and urinary Ang II levels in Akita Nrf2 KO mice compared with Akita mice. Urinary Ang 1-7 levels were normalized in Akita Nrf2 KO mice compared with Akita mice, whereas Nrf2 deficiency did not affect GFR/BW.
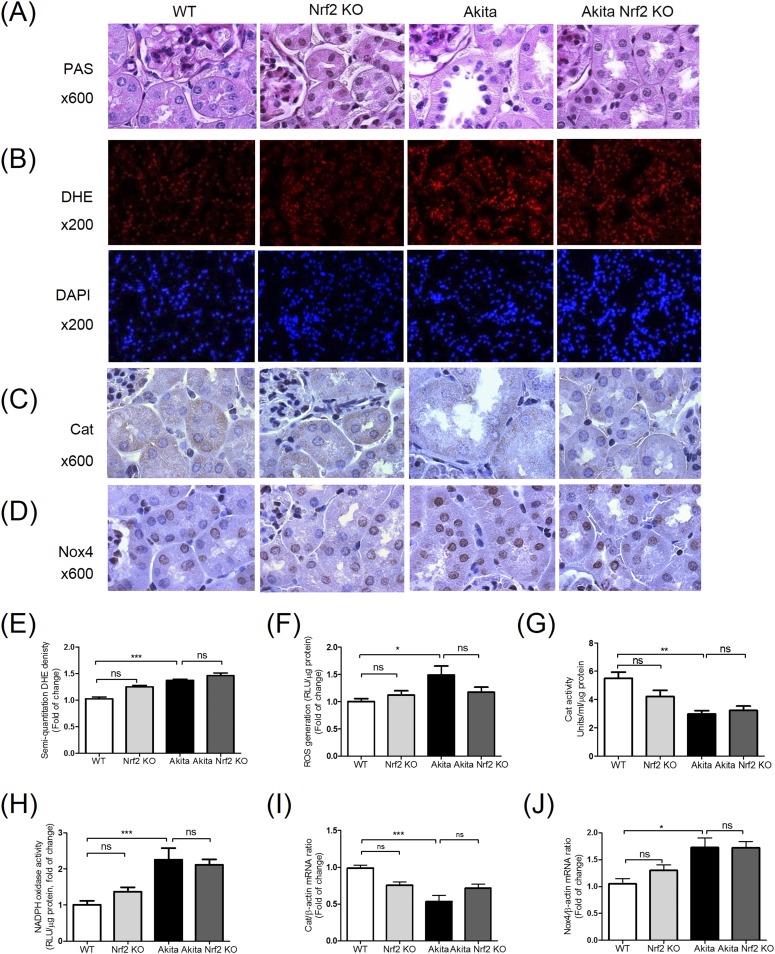
Histology
Confirming earlier observations (5, 6, 15, 17, 26), the kidneys of Akita mice exhibited structural damage. The histological changes included proximal tubule cell atrophy, tubular luminal dilatation with accumulation of cell debris, and increased extracellular matrix proteins in glomeruli and tubules [Fig. 2(A); Table 3]. Nrf2 KO markedly reversed, albeit never completely resolved, these abnormalities.
Figure 2.
Characterization of Akita Nrf2 KO mice. (A) Periodic acid-Schiff (PAS) staining (magnification ×600), (B) DHE (red) and DAPI staining (blue) (magnification ×200), (C) Cat and (D) Nox4 immunostaining in kidney sections (magnification ×600) from male WT, Nrf2 KO, Akita, and Akita Nrf2 KO mouse kidneys at age 20 weeks. Semiquantification of (E) DHE fluorescence, (F) ROS production, (G) Cat activity, (H) nicotinamide adenine dinucleotide phosphate (NADPH) oxidase activity, (I) Cat mRNA, and (J) Nox4 mRNA expression in RPTs of WT controls, Nrf2 KO, Akita, and Akita Nrf2 KO mice. Values are expressed as mean ± SEM; n = 8 per group. *P < 0.05; **P < 0.01; ***P < 0.005. WT (empty bars), Nrf2 KO mice (light gray bars), Akita (solid black bars), and Akita Nrf2 KO mice (dark gray bars). DAPI, 4′,6-diamidino-2-phenylindole; ns, not significant; SEM, standard error of the mean.
We detected significantly stronger staining for DHE [Fig. 2(B)] and DCFDA [Supplemental Fig. 1(A) (630.7KB, pdf) ] in RPTs from Akita mice than in those from WT and Nrf2 KO mice, but the staining did not differ from that in Akita Nrf2 KO mice. These findings were confirmed by semiquantification of DHE [Fig. 2(E)] and assessment of ROS levels in RPTs by the lucigenin assay [Fig. 2(F)].
Immunostaining for Cat [Fig. 2(C)] and nicotinamide adenine dinucleotide phosphate (NADPH) oxidase 4 (Nox4) [Fig. 2(D)] were lower and higher, respectively, in RPTCs from Akita mice than in those from WT or Nrf2 KO mice. Nrf2 deficiency did not affect Cat and Nox4 expression compared with Akita mice. These findings were confirmed by quantification of Cat and NADPH oxidase activity in RPTs [Fig. 2(G) and 2(H), respectively] and by RT-qPCR of mRNAs [Fig. 2(I) and 2(J), respectively] from isolated RPTs. No changes in Nox1 and Nox2 mRNA levels were detected in the different groups [Supplemental Fig. 2(A) and 2(B) (630.7KB, pdf) , respectively].
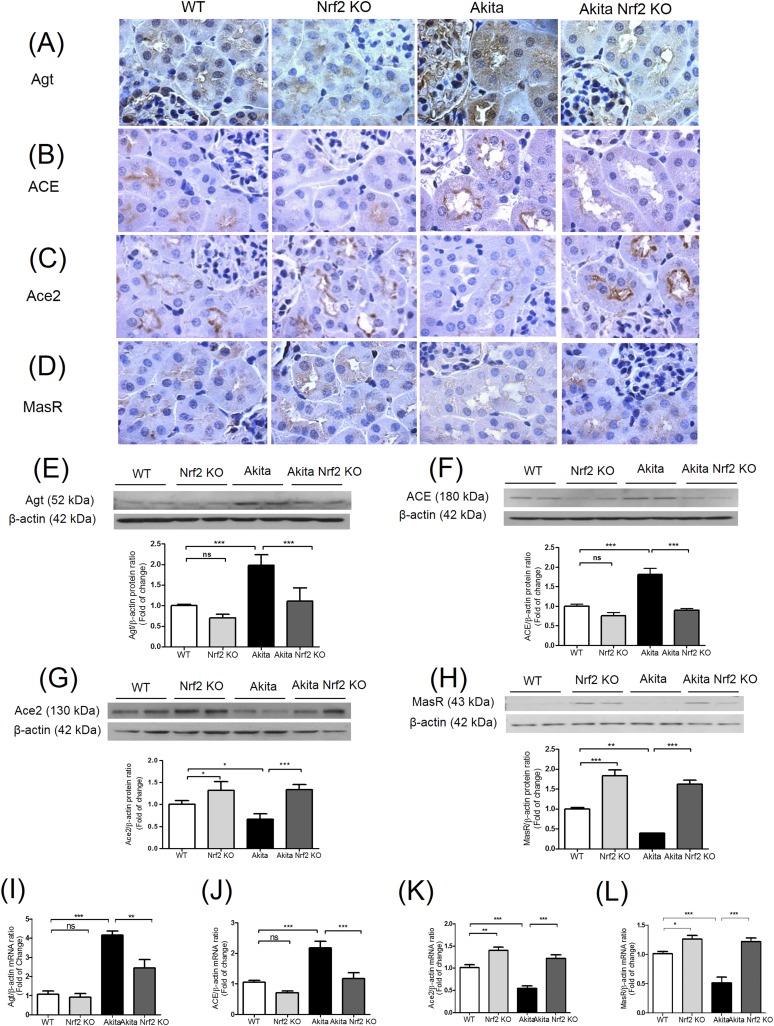
Effects of Nrf2 deletion on Agt, ACE, Ace2, and MasR expression in Akita mice
Immunostaining revealed higher Agt [Fig. 3(A)] and ACE [Fig. 3(B)] expression in RPTCs from Akita mice than in those from WT or Nrf2 KO mice. In contrast, Ace2 [Fig. 3(C)] and MasR [Fig. 3(D)] expression was lower in RPTCs from Akita mice than in those from WT or Nrf2 KO mice. Akita Nrf2-deficient mice exhibited enhanced Ace2 and MasR expression [Fig. 3(C) and 3(D), respectively]. Moreover, Ace2 and MasR expression was higher in RPTCs from Nrf2 KO mice than in those from WT mice [Fig. 3(C) and 3(D), respectively]. These findings were confirmed by WB for Agt, ACE, Ace2, and MasR [Fig. 3(E), 3(F), 3 (G), and 3(H)], respectively) and by RT-qPCR of their respective mRNAs [Fig. 3(I)–3(L)] from isolated RPTs.
Figure 3.
Agt, ACE, Ace2, and MasR expression in mouse kidneys at week 20. Immunohistochemical staining of (A) Agt, (B) ACE, (C) Ace2, and (D) MasR in mouse kidneys. Magnification ×600. WB of (E) Agt, (F) ACE, (G) Ace2, and (H) MasR expression and RT-qPCR analysis of (I) Agt, (J) ACE, (K) Ace2, and (L) MasR mRNA levels in RPTs of WT, Nrf2 KO, Akita, and Akita Nrf2 KO mice. Values are expressed as mean ± SEM; n = 8 per group. *P < 0.05; **P < 0.01; ***P < 0.005. WT (empty bars), Nrf2 KO mice (light gray bars), Akita (solid black bars), and Akita Nrf2 KO mice (dark gray bars). ns, not significant; SEM, standard error of the mean.
Effects of Nrf2 deficiency on tubulointerstitial fibrosis in Akita mice
Masson trichrome staining revealed higher collagenous matrix protein expression [Supplemental Fig. 1(B) (630.7KB, pdf) ] in the tubulointerstitium of Akita mice compared with that of WT or Nrf2 KO mice, with more pronounced attenuation in Akita Nrf2 KO mice. Increased immunostaining of transforming growth factor (TGF)–β1, fibronectin-1 (FN1), and collagen 1 (Col 1) [Supplemental Fig. 1(C), 1(D), and 1(E) (630.7KB, pdf) , respectively] was also detected in the tubulointerstitium of Akita mice compared with that of WT or Nrf2 KO mice. Genetic deletion of Nrf2 in Akita mice markedly attenuated TGF-β1, FN1, and Col 1 expression [Supplemental Fig. 1(C), 1(D), and 1(E) (630.7KB, pdf) , respectively]. Semiquantification of Masson staining [Supplemental Fig. 1(F) (630.7KB, pdf) ] and RT-qPCR of TGF-β1, FN1, and Col I mRNA from isolated RPTs [Supplemental Fig. 1(G), 1(H), and 1(I) (630.7KB, pdf) , respectively] confirmed these findings.
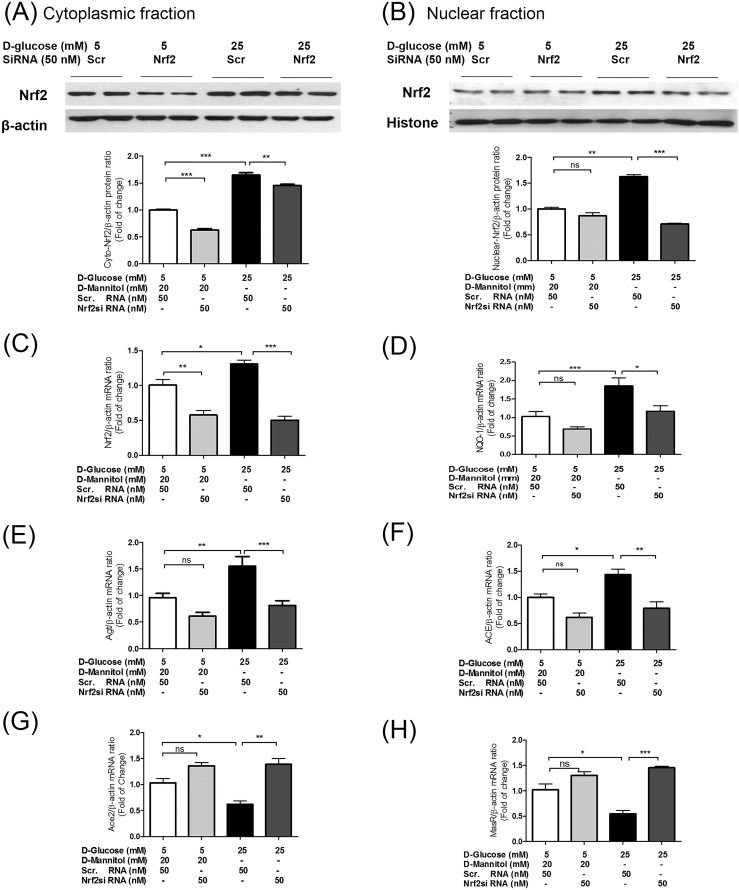
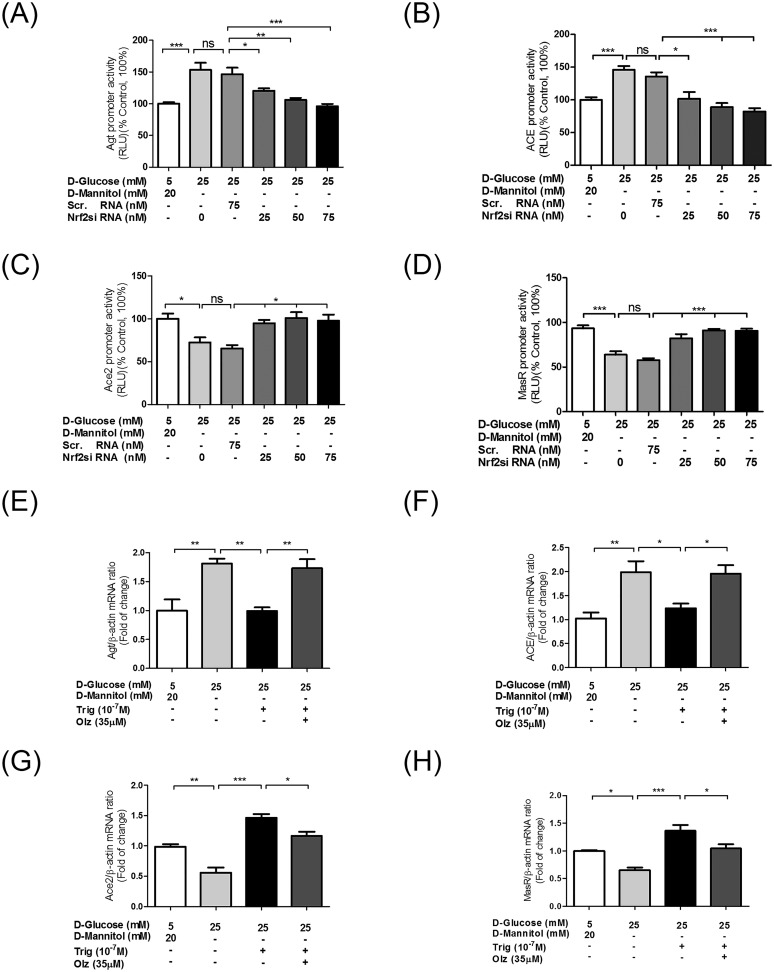
Effects of Nrf2 siRNA on Agt, ACE, Ace2, and MasR gene expression in isolated IRPTCs
Consistent with our previous observations (5, 6), HG enhanced Nrf2 expression in both cytoplasmic [Fig. 4(A)] and nuclear fractions [Fig. 4(B)] of IRPTCs compared with NG. Nrf2 siRNA transfection reduced cytoplasmic Nrf2 in IRPTCs cultured in NG and HG. It had no effect on nuclear Nrf2 in NG but lowered Nrf2 expression in HG in IRPTCs. Transient Nrf2 siRNA transfection also significantly inhibited Nrf2 but not NQO-1 mRNA expression in IRPTCs in NG and prevented HG stimulation of Nrf2 and NQO-1 mRNA expression compared with Scr siRNA [Fig. 4(C) and 4(D), respectively). Furthermore, Nrf2 siRNA transfection prevented increases of Agt and ACE and decreases of Ace2 and MasR in response to HG at the mRNA level [Fig. 4(E), 4(F), 4(G), and 4(H), respectively], as well as their respective promoter activities [Fig. 5(A), 5(B), 5(C), and 5(D), respectively].
Figure 4.
Effect of Nrf2 siRNA on Nrf2, NQO-1, Agt, ACE, Ace2, and MasR gene expression in IRPTCs in NG (normal glucose) and HG (high glucose) media. (A) Effect of Nrf2 siRNA or Scr siRNA on Nrf2 protein expression in cytoplasmic fraction and (B) nuclear fraction of IRPTCs incubated in NG and HG media and quantified by WB. NE-PER Nuclear and Cytoplasmic Extraction Reagents were used for the isolation of cytoplasmic and nuclear fractions from IRPTCs according to the manufacturer’s protocol (Catalog No. 78833; Thermo Scientific; Pierce Biotechnology, Rockford, IL). Effect of Nrf2 siRNA or Scr siRNA on (C) Nrf2, (D) NQO-1, (E) Agt, (F) ACE, (G) Ace2, and (H) MasR mRNA expression in IRPTCs incubated in NG and HG media and quantified by RT-qPCR. Cells were harvested after 24 hours of incubation. mRNA levels in cells incubated in NG medium with Scr RNA are expressed as arbitrary unit 1. The results are reported as percentages of control values (mean ± SEM; n = 3 for three separate experiments done in triplicates. *P < 0.05; **P < 0.01; ***P = 0.005. NG + Scr siRNA (empty bars), NG + Nrf2 siRNA (light gray bars), HG + Scr siRNA (solid black bars), and HG + Nrf2 siRNA (dark gray bars). ns, not significant; SEM, standard error of the mean.
Figure 5.
Effect of Nrf2 siRNA and trigonelline on Agt, ACE, Ace2, and MasR promoter activity and mRNA in IRPTCs in HG medium. Dose-dependent effect of Nrf2 siRNA and Scr siRNA on (A) Agt, (B) ACE, (C) Ace2, and (D) MasR promoter activity in stably transfected IRPTCs incubated in HG medium and quantified by luciferase activity assay. Effect of trigonelline (Trig) ± oltipraz (Olz) on (E) Agt, (F) ACE, (G) Ace2, and (H) MasR mRNA expression in IRPTCs incubated in HG medium and quantified by RT-qPCR. Cells were harvested after 24 hours of incubation. Promoter activity and mRNA levels in cells incubated in NG medium are expressed as 100% control and arbitrary unit 1, respectively. The results are reported as percentages or fold of change of control values (mean ± SEM; n = 3 for three separate experiments done in triplicates). *P < 0.05; **P < 0.01; ***P < 0.005. ns, not significant; SEM, standard error of the mean.
To confirm the impact of Nrf2 on Agt, ACE, Ace2, and MasR expression in IRPTCs, we studied the effects of the Nrf2 inhibitor alkaloid trigonelline ± the Nrf2 activator oltipraz. Trigonelline treatment prevented HG stimulation of Agt and ACE and suppression of Ace2 and MasR mRNA expression in IRPTCs, and these actions were abrogated by oltipraz [Fig. 5(E), 5(F), 5(G), and 5(H), respectively].
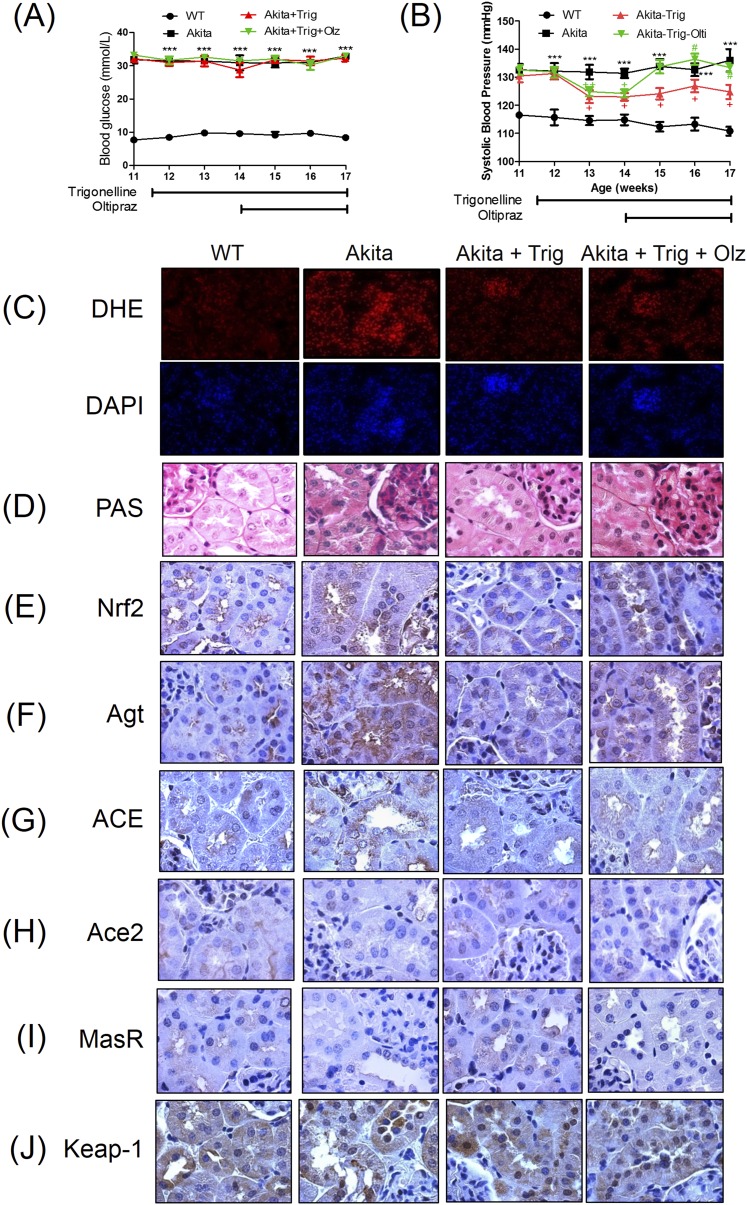
Effect of trigonelline and oltipraz on expression of intrarenal RAS in Akita mice
Trigonelline administration did not affect BG [Fig. 6(A)], whereas it significantly lowered SBP in Akita mice [Fig. 6(B); Table 4]. This was reversed by oltipraz treatment. Trigonelline significantly decreased the KW/BW and KW/tibial length ratios but not urinary albumin-creatinine ratio and Ang II/creatinine levels (Table 4). These actions were also reversed by oltipraz. Interestingly, trigonelline treatment completely normalized urinary Ang 1-7/creatinine levels in Akita mice compared with non-Akita mice, without affecting GFR/BW.
Figure 6.
Effect of trigonelline on Nrf2, Agt, ACE, Ace2, and MasR expression in Akita mice in vivo. Longitudinal changes in mean (A) BG and (B) SBP in male WT (●), Akita (■), Akita + trigonelline (Trig) (▲), and Akita + Trig + Oltipraz (Olz) (▼) mice. Values are mean ± SEM; n = 9 per group. ***P < 0.005 Akita mice compared with WT mice; +P < 0.05 Akita mice compared with Akita + Trig mice; #P < 0.05 Akita + Trig mice compared with Akita + Trig + Olz mice. (C) DHE (red) and DAPI staining (blue) (magnification ×200) and (D) PAS staining and immunohistochemical staining for (E) Nrf2, (F) Agt, (G) ACE, (H) Ace2, (I) MasR, and (J) Keap1 in the kidneys of WT and Akita ± Trig and Olz mice. Magnification ×600. SEM, standard error of the mean.
Table 4.
Physiological and Histological Measurements at Age 17 Weeks
| WT | Akita | Akita + Trig | Akita + Trig + Olz | |
|---|---|---|---|---|
| Blood glucose, mM (n = 9) | 8.87 ± 0.44 | 32.86 ± 0.19a | 31.72 ± 1.11a | 32.69 ± 0.39a |
| Systolic blood pressure, mm Hg (n = 9) | 111.0 ± 0.50 | 136.0 ± 1.43a | 124.1 ± 0.84a,b | 133.4 ± 0.52a,c |
| BW, g (n = 9) | 32,75 ± 0.60 | 22.65 ± 0.84a | 22.88 ± 0.54a | 21.14 ± 0.40a |
| KW, mg (n = 9) | 364.3 ± 9.83 | 549.8 ± 9.15a | 514.7 ± 9.43a | 528.3 ± 4.77a |
| TL, mm (n = 9) | 22.56 ± 0.46 | 21.87 ± 0.41 | 21.32 ± 0.52 | 20.95 ± 0.28 |
| KW/BW, mg/g (n = 9) | 11.12 ± 0.40 | 24.24 ± 0.89a | 21,51 ± 0.42a,d | 24.92 ± 0.64a,e |
| KW/TL, mg/mm (n = 9) | 16.19 ± 0.34 | 26.04 ± 0.68a | 23.01 ± 0.82a,f | 25.95 ± 0.51a,e |
| GFR/BW, mL/min/g (n = 9) | 9.92 ± 0.80 | 22 ± 1.96a | 21.15 ± 1.12a | 20.25 ± 0.58a |
| ACR, µg/mg (n = 9) | 22.22 ± 1.64 | 105.10 ± 19.87g | 82.19 ± 20.79 | 123.0 ± 32.91h |
| Urinary Ang II/creatinine, ng/mg (n = 9) | 1.27 ± 0.15 | 25.92 ± 1.93a | 16.79 ± 1.87g | 23.84 ± 3.03a |
| Urinary Ang (1–7)/creatinine, ng/mg (n = 9) | 2.61 ± 0.55 | 0.83 ± 0.15h | 2.65 ± 0.39f | 2.4 ± 0.33d |
Abbreviations: ACR, albumin-creatinine ratio; KW, kidney weight; TL, tibial length.
P < 0.001 vs WT.
P < 0.001 vs Akita.
P < 0.001 vs Akita + Trig.
P < 0.05 vs Akita.
P < 0.01 vs Akita + Trig.
P < 0.01 vs Akita.
P < 0.01 vs WT.
P < 0.05 vs WT.
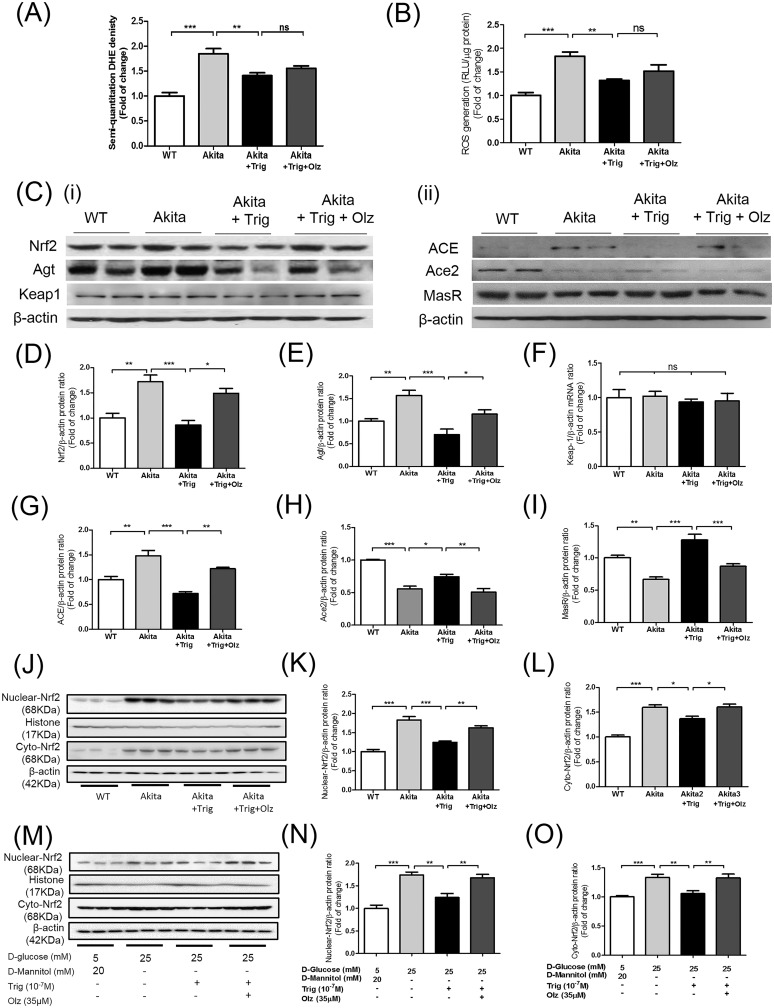
To test the antioxidant capacity of trigonelline, we examined the effect of trigonelline on oxidative stress in kidneys of Akita mice. Treatment of Akita mice with trigonelline markedly attenuated DHE staining [Fig. 6(C); semiquantification of DHE staining is shown in Fig. 7(A)] and reduced ROS levels in RPTs assessed by the lucigenin assay [Fig. 7(B)]. Furthermore, trigonelline prevented HG-induced ROS generation in IRPTCs in a concentration-dependent manner [Supplemental Fig. 3(A) (630.7KB, pdf) ]. Thus, trigonelline possesses an intrinsic antioxidant property to lower ROS generation in diabetic RPTCs.
Figure 7.
Effect of trigonelline (Trig) on oxidative stress and RPT Nrf2, Agt, ACE, Ace2, and MasR expression in mice in vivo. (A) Semiquantification of DHE fluorescence, (B) ROS production, (C) WB of (panel i) Nrf2, Agt, and Keap1 expression and (panel ii) ACE, Ace2, and MasR expression in RPTs of WT and Akita mice ± Trig and oltipraz (Olz). WB quantification of (D) Nrf2, (E) Agt, (F) Keap1, (G) ACE, (H) Ace2, and (I) MasR expression in RPTs of WT and Akita mice ± trigonelline and oltipraz. (J) WB of Nrf2 protein expression and quantitation in (K) nuclear fraction and (L) cytosolic fraction in RPTs of WT and Akita mice ± Trig and oltipraz, respectively. (M) WB of Nrf2 protein expression and quantitation in (N) nuclear fraction and (O) cytosolic fraction of IRPTCs incubated in NG, HG, and HG ± Trig and Olz, respectively. Values are expressed as mean ± SEM (n = 6 per group). *P < 0.05; **P < 0.01; ***P < 0.005. WT (empty bars), Akita mice (light gray bars), Akita mice treated with Trig (solid black bars), and Akita mice treated with Trig and Olz (dark gray bars). ns, not significant; SEM, standard error of the mean.
Trigonelline also markedly attenuated renal damage, including glomerulosclerosis, tubule lumen dilatation, and accumulation of cell debris as assessed with periodic acid-Schiff staining [Fig. 6(D)], and these changes were reversed by oltipraz. Consistently, RPTCs of Akita mice exhibited higher immunostaining for Nrf2 [Fig. 6(E)], Agt [Fig. 6(F)], and ACE [Fig. 6(G)] than RPTCs of WT mice. In contrast, lower immunostaining of Ace2 [Fig. 6(H)] and MasR [Fig. 6(I)] was observed in Akita mice. Trigonelline reduced Nrf2, Agt, and ACE expression [Fig. 6(E), 6(F), and 6(G), respectively] and increased Ace2 and MasR expression [Fig. 6(H) and 6(I), respectively] to levels comparable to those detected in WT mice, and these effects were reversed by oltipraz. Trigonelline did not affect Keap1 expression in Akita mice [Fig. 6(J)]. WB of Nrf2, Agt, Keap1 [Fig. 7(Ci), 7(D), 7(E), and 7(F), respectively], ACE, Ace2, and MasR [Fig. 7(Cii), 7(G), 7(H), and 7(I), respectively], and RT-qPCR of Nrf2, Agt, Keap1, ACE, Ace2, and MasR mRNA expression [Supplemental Fig. 2(C), 2(D), 2(E), 2(F), 2(G), and 2(H) (630.7KB, pdf) , respectively] confirmed these findings. Furthermore, trigonelline treatment prevented Nrf2 nuclear translocation and decreased cytosolic Nrf2 expression in RPTs of Akita mice [Fig. 7(J)–7(L)] and in IRPTCs cultured in HG [Fig. 7(M)–7(O)]. These effects were reversed by oltipraz.
Discussion
Our results document that selective genetic deletion of Nrf2 or pharmacological blockade of Nrf2 with trigonelline in Akita mice effectively upregulated RPTC Ace2/MasR and suppressed Agt/ACE expression, resulting in attenuation of systemic hypertension and kidney injury. Consistently in cultured IRPTCs, Nrf2 siRNA transfection or trigonelline treatment prevented HG-induced upregulation of Agt/ACE and downregulation of Ace2/MasR gene expression. The effects of trigonelline were reversed by oltipraz both in vitro and in vivo. These data identify a mechanism underlying Nrf2 activation by oxidative stress (secondary to hyperglycemia) that stimulates intrarenal RAS gene expression and activation, leading to the development of hypertension and nephropathy in diabetes.
Akita mice, an autosomal dominant model of spontaneous type 1 diabetes with a mutated Ins2 gene, have decreased numbers of pancreatic islet β-cells and have developed hyperglycemia as early as 3 to 4 weeks of age (31). By age 13 to 30 weeks, male Akita mice manifest impaired renal function and increased oxidative stress markers in their RPTs (32, 33). Akita mice represent a useful model to study the early to moderately advanced renal morphological changes in patients with type 1 diabetes.
In the current study, we found that Nrf2 and NQO-1 expression was increased in RPTs of 20-week-old Akita mice compared with those of WT mice. This was associated with marked increases in ROS generation, NADPH oxidase activity, and Nox4 mRNA expression, whereas Cat activity and Cat mRNA expression were lower in RPTCs of Akita mice than in those of WT mice. These changes were similar to those detected in Akita Nrf2 KO mice, indicating that hyperglycemia-induced oxidative stress and higher Nox4 activity with suppressed Cat activity may contribute to renal injury in Akita mice.
We do not presently understand why increased Nrf2 expression and activity (reflected by heightened NQO-1 expression) cannot attenuate oxidative stress (as evidenced by augmented DHE and DCFDA staining and ROS generation) in Akita mice. Our data, including our previous reports (5, 6) and studies in diabetic rats by other groups (34, 35), document reduced Cat activity in diabetic mice. Thus, one possibility is that hyperglycemia results in decreased Sirtuin-1 and Foxo3α expression and consequently lowers Cat expression, thereby enhancing ROS generation in diabetic kidneys (36, 37). Another possible explanation is that hyperglycemia enhances nuclear factor κB (NF-κB) activation to compete for Nrf2 stimulation of transcription of antioxidant genes including Cat. The latter possibility is supported by the findings that the phosphorylated NF-κB p65 subunit and Nrf2 both bind to the same domain of CREB-binding protein, a coactivator of Nrf2 (38). The phospho-NF-κB p65 subunit could then attenuate the transcription of antioxidant RE-dependent genes by depriving CREB-binding protein from Nrf2 through a competitive mechanism (38).
The mechanisms leading to SBP elevation in Akita mice are incompletely understood. The possibility that downregulation of Ace2 and MasR gene expression and upregulation of Agt and ACE gene expression, yielding higher Ang II/Ang 1-7 ratios that facilitate the development of hypertension, has received considerable attention (39–41). Indeed, our data disclosed significantly higher RPTC Agt and ACE expression and urinary Ang II levels with lower RPTC Ace2 and MasR expression and urinary Ang 1-7 levels in Akita mice than in WT mice. These observations are consistent with our earlier findings of markedly elevated ACE and depressed Ace2 expression in the kidneys of Akita Agt-Tg mice (21), suggesting that upregulation of Ace2/MasR expression to increase Ang 1-7 level is important to downregulate Agt/ACE expression and prevent systemic hypertension in Akita mice (26). These findings are consistent with clinical reports of heightened intrarenal RAS and urinary Ang II expression with lower Ace2 expression in patients with hypertensive diabetic (42–46).
The exact mechanism(s) by which Nrf2 deficiency leads to downregulation of renal Agt/ACE and upregulation of Ace2/MasR gene expression in diabetes remain(s) unclear. One possibility is that hyperglycemia/ROS augments Nrf2 activation by promoting its dissociation from Keap1 and translocation into the nucleus. Nrf2 then binds to Nrf2-binding sites in the Agt/ACE gene promoter regions and promotes Agt/ACE gene expression. Previously, we showed that Nrf2 binded to Nrf2-binding sites in the Agt gene promoter (5). Thus, Nrf2 deletion in Akita mice should diminish Agt gene expression. Consistently, Nrf2 siRNA transfection diminished HG stimulation of Agt/ACE gene promoter activity and upregulation of the Ace2/MasR gene promoter in IRPTCs. These observations could be explained by the presence of Nrf2-REs in the Agt gene promoter (5) and of potential putative Nrf2-REs in ACE, Ace2, and MasR gene promoters. Indeed, studies are ongoing in our laboratory to identify these putative Nrf2-REs.
How might oxidative stress lead to interstitial fibrosis in Akita mice? One possibility is that augmented Agt/ACE expression with Ang II elevation via ROS generation stimulates TGF-β1 and subsequently enhances the expression of extracellular matrix proteins and profibrotic genes in RPTCs, resulting in interstitial fibrosis (47). Indeed, neutralizing TGF-β1 with antibody was reported to alleviate fibrosis and tubule cell apoptosis in animal models of diabetes (48). We also detected higher TGF-β1, FN1, and Col I protein and mRNA expressions in the RPTs of Akita mice than in those of WT controls. These increases were mitigated in Akita Nrf2 KO mice, linking Nrf2 with intrarenal RAS activation and upregulation of TGF-β1 expression in RPTs and consequently to interstitial fibrosis in Akita mice. Thus, our findings support the notion that Nrf2 activation aggravates tubulointerstitial fibrosis with nephropathy progression in diabetes.
At present, our data do not dealineate whether kidney damage in Akita mice is due to hyperglycemia or hypertension per se. We previously reported that dual RAS blockade normalized Ace2 expression and prevented hypertension and tubular apoptosis in Akita angiotensinogen-Tg mice without affecting hyperglycemia (21), suggesting that the hypertension induced by intrarenal RAS activation plays a predominant role in diabetic nephropathy progression. Furthermore, our recent observation that insulin treatment normalized hyperglycemia and hypertension, inhibited Nrf2 gene expression, and prevented Nrf2 stimulation of Agt gene expression in RPTs of Akita mice (6) indicates that hyperglycemia can evoke intrarenal RAS gene expression and subsequently hypertension development in diabetes. Thus, these studies point to the importance of hyperglycemia-induced intrarenal RAS activation via Nrf2 expression in the development of hypertension in Akita mice. Clearly, more studies are needed to define the contribution of hypertension and hyperglycemia to kidney damage in diabetes.
The exact mode of the mechanism by which trigonelline decreases Nrf2 protein levels in the RPTs of Akita mice is unknown. However, we found that trigonelline decreased oxidative stress (DHE staining) in the kidneys of Akita mice and inhibited Nrf2 promoter activity, Nrf2 mRNA expression, and Nrf2 nuclear translocation in IRPTCs in HG. These data indicate that trigonelline inhibits Nrf2 protein expression via inhibition of Nrf2 gene transcription by lowering oxidative stress in diabetic RPTCs. These data are consistent with our previous report that overexpression of catalase in RPTCs inhibited Nrf2 expression in Akita mice (5). Furthermore, lowering Nrf2 nuclear translocation by trigonelline may prevent positive autofeedback of Nrf2 on Nrf2 gene transcription (49). Clearly, more studies are needed to elucidate the underlying mechanism of trigonelline action on Nrf2 expression.
In summary, our findings document that selective Nrf2 KO upregulated renal Ace2/MasR gene expression with downregulation of Agt/ACE gene expression and prevented systemic hypertension and renal injury in diabetes. Our results imply an important role for oxidative stress‒induced Nrf2 expression and activation in the development of hypertension and renal injury in diabetes by altering local intrarenal RAS expression.
Acknowledgments
Editorial assistance was provided by the Centre Hospitalier de l’Université de Montréal Research Support Office and Ovid Da Silva.
Financial Support: The present investigation was supported by grants from the Canadian Institutes of Health Research [CIHR, MOP-84363, MOP-93650, and MOP-16088 (to J.S.D.C.); MOP-86450 (to S.-L.Z.); MOP-494266 (to J.W.S.); and MOP-97742 (to J.G.F.)], the Canadian Diabetes Association [NOD_OG-3-14-4472-JC (to J.S.D.C.)], and the National Institutes of Health [HL-48455 (to J.R.I.)].
Author Contributions: S.Z. researched the data and contributed to the discussion. A.G. researched the data. C.-S.L. researched the data. I.C. researched the data. J.W.S. contributed to the discussion and reviewed the manuscript. J.G.F. contributed to the discussion and reviewed/edited the manuscript. J.R.I. contributed to the discussion and reviewed/edited the manuscript. S.-L.Z. researched the data, contributed to the discussion and edited the manuscript. J.S.D.C. contributed to the discussion and wrote, reviewed, and edited the manuscript.
Acknowledgments
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- ACE
- angiotensin-converting enzyme
- Ace2
- angiotensin-converting enzyme-2
- Agt
- angiotensinogen
- Ang 1-7
- angiotensin 1-7
- Ang II
- angiotensin II
- BG
- blood glucose
- BM
- bardoxolone methyl
- BW
- body weight
- Cat
- catalase
- Col 1
- collagen 1
- DCFDA
- 5-(6)-carboxy-2′,7′-dichlorodihydrofluorescein diacetate
- DHE
- dihydroethidium
- DMEM
- Dulbecco’s modified Eagle medium
- FN1
- fibronectin-1
- GFR
- glomerular filtration rate
- HG
- high glucose
- Ins2
- insulin 2
- IRPTC
- immortalized renal proximal tubular cell
- Keap1
- Kelch-like ECH-associated protein 1
- KO
- knockout
- KW
- kidney weight
- MasR
- angiotensin 1-7 receptor
- mRNA
- messenger RNA
- NADPH
- nicotinamide adenine dinucleotide phosphate
- NF-κB
- nuclear factor
- NG
- normal glucose
- Nox4
- nicotinamide adenine dinucleotide phosphate oxidase 4
- NQO-1
- NAD(P)H quinone oxidoreductase 1
- Nrf2
- nuclear factor erythroid 2–related factor 2
- RAS
- renin-angiotensin system
- RE
- response element
- ROS
- reactive oxygen species
- RPT
- renal proximal tubule
- RPTC
- renal proximal tubule cell
- RT-qPCR
- real-time quantitative polymerase chain reaction
- SBP
- systolic blood pressure
- Scr
- scrambled
- siRNA
- small interfering RNA
- T2D
- type 2 diabetes
- Tg
- transgenic
- TGF
- transforming growth factor
- WB
- Western blotting
- WT
- wild-type.
References
- 1.Venugopal R, Jaiswal AK. Nrf1 and Nrf2 positively and c-Fos and Fra1 negatively regulate the human antioxidant response element-mediated expression of NAD(P)H:quinone oxidoreductase1 gene. Proc Natl Acad Sci USA. 1996;93(25):14960–14965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Motohashi H, Yamamoto M. Nrf2-Keap1 defines a physiologically important stress response mechanism. Trends Mol Med. 2004;10(11):549–557. [DOI] [PubMed] [Google Scholar]
- 3.Surh YJ, Kundu JK, Na HK. Nrf2 as a master redox switch in turning on the cellular signaling involved in the induction of cytoprotective genes by some chemopreventive phytochemicals. Planta Med. 2008;74(13):1526–1539. [DOI] [PubMed] [Google Scholar]
- 4.Chan K, Lu R, Chang JC, Kan YW. NRF2, a member of the NFE2 family of transcription factors, is not essential for murine erythropoiesis, growth, and development. Proc Natl Acad Sci USA. 1996;93(24):13943–13948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdo S, Shi Y, Otoukesh A, Ghosh A, Lo CS, Chenier I, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Catalase overexpression prevents nuclear factor erythroid 2-related factor 2 stimulation of renal angiotensinogen gene expression, hypertension, and kidney injury in diabetic mice. Diabetes. 2014;63(10):3483–3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghosh A, Abdo S, Zhao S, Wu CH, Shi Y, Lo CS, Chenier I, Alquier T, Filep JG, Ingelfinger JR, Zhang SL, Chan JSD. Insulin inhibits Nrf2 gene expression via heterogeneous nuclear ribonucleoprotein F/K in diabetic mice. Endocrinology. 2017;158(4):903–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saha PK, Reddy VT, Konopleva M, Andreeff M, Chan L. The triterpenoid 2-cyano-3,12-dioxooleana-1,9-dien-28-oic-acid methyl ester has potent anti-diabetic effects in diet-induced diabetic mice and Lepr(db/db) mice. J Biol Chem. 2010;285(52):40581–40592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chin M, Lee CY, Chuang JC, Bumeister R, Wigley WC, Sonis ST, Ward KW, Meyer C. Bardoxolone methyl analogs RTA 405 and dh404 are well tolerated and exhibit efficacy in rodent models of Type 2 diabetes and obesity. Am J Physiol Renal Physiol. 2013;304(12):F1438–F1446. [DOI] [PubMed] [Google Scholar]
- 9.Zoja C, Corna D, Nava V, Locatelli M, Abbate M, Gaspari F, Carrara F, Sangalli F, Remuzzi G, Benigni A. Analogs of bardoxolone methyl worsen diabetic nephropathy in rats with additional adverse effects. Am J Physiol Renal Physiol. 2013;304(6):F808–F819. [DOI] [PubMed] [Google Scholar]
- 10.Tan SM, Sharma A, Stefanovic N, Yuen DY, Karagiannis TC, Meyer C, Ward KW, Cooper ME, de Haan JB. Derivative of bardoxolone methyl, dh404, in an inverse dose-dependent manner lessens diabetes-associated atherosclerosis and improves diabetic kidney disease. Diabetes. 2014;63(9):3091–3103. [DOI] [PubMed] [Google Scholar]
- 11.Pergola PE, Raskin P, Toto RD, Meyer CJ, Huff JW, Grossman EB, Krauth M, Ruiz S, Audhya P, Christ-Schmidt H, Wittes J, Warnock DG; BEAM Study Investigators . Bardoxolone methyl and kidney function in CKD with type 2 diabetes. N Engl J Med. 2011;365(4):327–336. [DOI] [PubMed] [Google Scholar]
- 12.de Zeeuw D, Akizawa T, Audhya P, Bakris GL, Chin M, Christ-Schmidt H, Goldsberry A, Houser M, Krauth M, Lambers Heerspink HJ, McMurray JJ, Meyer CJ, Parving HH, Remuzzi G, Toto RD, Vaziri ND, Wanner C, Wittes J, Wrolstad D, Chertow GM; BEACON Trial Investigators . Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med. 2013;369(26):2492–2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brezniceanu ML, Liu F, Wei CC, Tran S, Sachetelli S, Zhang SL, Guo DF, Filep JG, Ingelfinger JR, Chan JS. Catalase overexpression attenuates angiotensinogen expression and apoptosis in diabetic mice. Kidney Int. 2007;71(9):912–923. [DOI] [PubMed] [Google Scholar]
- 14.Brezniceanu ML, Liu F, Wei CC, Chénier I, Godin N, Zhang SL, Filep JG, Ingelfinger JR, Chan JS. Attenuation of interstitial fibrosis and tubular apoptosis in db/db transgenic mice overexpressing catalase in renal proximal tubular cells. Diabetes. 2008;57(2):451–459. [DOI] [PubMed] [Google Scholar]
- 15.Shi Y, Lo CS, Chenier I, Maachi H, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Overexpression of catalase prevents hypertension and tubulointerstitial fibrosis and normalization of renal angiotensin-converting enzyme-2 expression in Akita mice. Am J Physiol Renal Physiol. 2013;304(11):F1335–F1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang L, Lei C, Zhang et al. Synergistic effect of dexamethasone and isoproterenol on the expression of angiotensinogen in immortalized rat proximal tubular cells. Kidney Int. 1998;53:287–295. [DOI] [PubMed] [Google Scholar]
- 17.Abdo S, Lo CS, Chenier I, Shamsuyarova A, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Heterogeneous nuclear ribonucleoproteins F and K mediate insulin inhibition of renal angiotensinogen gene expression and prevention of hypertension and kidney injury in diabetic mice. Diabetologia. 2013;56(7):1649–1660. [DOI] [PubMed] [Google Scholar]
- 18.Lo CS, Shi Y, Chang SY, Abdo S, Chenier I, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Overexpression of heterogeneous nuclear ribonucleoprotein F stimulates renal Ace-2 gene expression and prevents TGF-β1-induced kidney injury in a mouse model of diabetes. Diabetologia. 2015;58(10):2443–2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sachetelli S, Liu Q, Zhang SL, Liu F, Hsieh TJ, Brezniceanu ML, Guo DF, Filep JG, Ingelfinger JR, Sigmund CD, Hamet P, Chan JS. RAS blockade decreases blood pressure and proteinuria in transgenic mice overexpressing rat angiotensinogen gene in the kidney. Kidney Int. 2006;69(6):1016–1023. [DOI] [PubMed] [Google Scholar]
- 20.Liu F, Brezniceanu ML, Wei CC, Chénier I, Sachetelli S, Zhang SL, Filep JG, Ingelfinger JR, Chan JS. Overexpression of angiotensinogen increases tubular apoptosis in diabetes. J Am Soc Nephrol. 2008;19(2):269–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lo CS, Liu F, Shi Y, Maachi H, Chenier I, Godin N, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Dual RAS blockade normalizes angiotensin-converting enzyme-2 expression and prevents hypertension and tubular apoptosis in Akita angiotensinogen-transgenic mice. Am J Physiol Renal Physiol. 2012;302(7):F840–F852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu F, Wei CC, Wu SJ, Chenier I, Zhang SL, Filep JG, Ingelfinger JR, Chan JS. Apocynin attenuates tubular apoptosis and tubulointerstitial fibrosis in transgenic mice independent of hypertension. Kidney Int. 2009;75(2):156–166. [DOI] [PubMed] [Google Scholar]
- 23.Godin N, Liu F, Lau GJ, Brezniceanu ML, Chénier I, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Catalase overexpression prevents hypertension and tubular apoptosis in angiotensinogen transgenic mice. Kidney Int. 2010;77(12):1086–1097. [DOI] [PubMed] [Google Scholar]
- 24.Aleksunes LM, Reisman SA, Yeager RL, Goedken MJ, Klaassen CD. Nuclear factor erythroid 2-related factor 2 deletion impairs glucose tolerance and exacerbates hyperglycemia in type 1 diabetic mice. J Pharmacol Exp Ther. 2010;333(1):140–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arlt A, Sebens S, Krebs S, Geismann C, Grossmann M, Kruse ML, Schreiber S, Schäfer H. Inhibition of the Nrf2 transcription factor by the alkaloid trigonelline renders pancreatic cancer cells more susceptible to apoptosis through decreased proteasomal gene expression and proteasome activity. Oncogene. 2013;32(40):4825–4835. [DOI] [PubMed] [Google Scholar]
- 26.Shi Y, Lo CS, Padda R, Abdo S, Chenier I, Filep JG, Ingelfinger JR, Zhang SL, Chan JS. Angiotensin-(1-7) prevents systemic hypertension, attenuates oxidative stress and tubulointerstitial fibrosis, and normalizes renal angiotensin-converting enzyme 2 and Mas receptor expression in diabetic mice. Clin Sci (Lond). 2015;128:649–663. [DOI] [PubMed] [Google Scholar]
- 27.Ingelfinger JR, Jung F, Diamant D, Haveran L, Lee E, Brem A, Tang SS. Rat proximal tubule cell line transformed with origin-defective SV40 DNA: autocrine ANG II feedback. Am J Physiol. 1999;276(2 Pt 2):F218–F227. [DOI] [PubMed] [Google Scholar]
- 28.Itoh K, Chiba T, Takahashi S, Ishii T, Igarashi K, Katoh Y, Oyake T, Hayashi N, Satoh K, Hatayama I, Yamamoto M, Nabeshima Y. An Nrf2/small Maf heterodimer mediates the induction of phase II detoxifying enzyme genes through antioxidant response elements. Biochem Biophys Res Commun. 1997;236(2):313–322. [DOI] [PubMed] [Google Scholar]
- 29.Xie T, Belinsky M, Xu Y, Jaiswal AK. ARE- and TRE-mediated regulation of gene expression: response to xenobiotics and antioxidants. J Biol Chem. 1995;270(12):6894–6900. [DOI] [PubMed] [Google Scholar]
- 30.Yagishita Y, Fukutomi T, Sugawara A, Kawamura H, Takahashi T, Pi J, Uruno A, Yamamoto M. Nrf2 protects pancreatic β-cells from oxidative and nitrosative stress in diabetic model mice. Diabetes. 2014;63(2):605–618. [DOI] [PubMed] [Google Scholar]
- 31.Yoshioka M, Kayo T, Ikeda T, Koizumi A. A novel locus, Mody4, distal to D7Mit189 on chromosome 7 determines early-onset NIDDM in nonobese C57BL/6 (Akita) mutant mice. Diabetes. 1997;46(5):887–894. [DOI] [PubMed] [Google Scholar]
- 32.Haseyama T, Fujita T, Hirasawa F, Tsukada M, Wakui H, Komatsuda A, Ohtani H, Miura AB, Imai H, Koizumi A. Complications of IgA nephropathy in a non-insulin-dependent diabetes model, the Akita mouse. Tohoku J Exp Med. 2002;198(4):233–244. [DOI] [PubMed] [Google Scholar]
- 33.Ueno Y, Horio F, Uchida K, Naito M, Nomura H, Kato Y, Tsuda T, Toyokuni S, Osawa T. Increase in oxidative stress in kidneys of diabetic Akita mice. Biosci Biotechnol Biochem. 2002;66(4):869–872. [DOI] [PubMed] [Google Scholar]
- 34.Celik S, Akkaya H. Total antioxidant capacity, catalase and superoxide dismutase on rats before and after diabetes. J Anim Vet Adv. 2009;8(8):1503–1508. [Google Scholar]
- 35.Takemoto K, Tanaka M, Iwata H, Nishihara R, Ishihara K, Wang DH, Ogino K, Taniuchi K, Masuoka N. Low catalase activity in blood is associated with the diabetes caused by alloxan. Clin Chim Acta. 2009;407(1-2):43–46. [DOI] [PubMed] [Google Scholar]
- 36.Hasegawa K, Wakino S, Yoshioka K, Tatematsu S, Hara Y, Minakuchi H, Washida N, Tokuyama H, Hayashi K, Itoh H. Sirt1 protects against oxidative stress-induced renal tubular cell apoptosis by the bidirectional regulation of catalase expression. Biochem Biophys Res Commun. 2008;372(1):51–56. [DOI] [PubMed] [Google Scholar]
- 37.Lo CS, Shi Y, Chenier I, Ghosh A, Wu CH, Cailhier JF, Ethier J, Lattouf JB, Filep JG, Ingelfinger JR, Zhang SL, Chan JSD. Heterogeneous Nuclear Ribonucleoprotein F Stimulates Sirtuin-1 Gene Expression and attenuates nephropathy progression in diabetic mice. Diabetes. 2017;66(7):1964–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liu GH, Qu J, Shen X. NF-kappaB/p65 antagonizes Nrf2-ARE pathway by depriving CBP from Nrf2 and facilitating recruitment of HDAC3 to MafK. Biochim Biophys Acta. 2008;1783(5):713–727. [DOI] [PubMed] [Google Scholar]
- 39.Batlle D, Wysocki J, Soler MJ, Ranganath K. Angiotensin-converting enzyme 2: enhancing the degradation of angiotensin II as a potential therapy for diabetic nephropathy. Kidney Int. 2012;81(6):520–528. [DOI] [PubMed] [Google Scholar]
- 40.Ingelfinger JR. Angiotensin-converting enzyme 2: implications for blood pressure and kidney disease. Curr Opin Nephrol Hypertens. 2009;18(1):79–84. [DOI] [PubMed] [Google Scholar]
- 41.Santos RA, Ferreira AJ. Angiotensin-(1-7) and the renin-angiotensin system. Curr Opin Nephrol Hypertens. 2007;16(2):122–128. [DOI] [PubMed] [Google Scholar]
- 42.Kobori H, Urushihara M, Xu JH, Berenson GS, Navar LG. Urinary angiotensinogen is correlated with blood pressure in men (Bogalusa Heart Study). J Hypertens. 2010;28(7):1422–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lai KN, Leung JC, Lai KB, To WY, Yeung VT, Lai FM. Gene expression of the renin-angiotensin system in human kidney. J Hypertens. 1998;16(1):91–102. [DOI] [PubMed] [Google Scholar]
- 44.Navar LG, Harrison-Bernard LM, Nishiyama A, Kobori H. Regulation of intrarenal angiotensin II in hypertension. Hypertension. 2002;39(2):316–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Navar LG, Prieto MC, Satou R, Kobori H. Intrarenal angiotensin II and its contribution to the genesis of chronic hypertension. Curr Opin Pharmacol. 2011;11(2):180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saito T, Urushihara M, Kotani Y, Kagami S, Kobori H. Increased urinary angiotensinogen is precedent to increased urinary albumin in patients with type 1 diabetes. Am J Med Sci. 2009;338(6):478–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dai C, Yang J, Liu Y. Transforming growth factor-beta1 potentiates renal tubular epithelial cell death by a mechanism independent of Smad signaling. J Biol Chem. 2003;278(14):12537–12545. [DOI] [PubMed] [Google Scholar]
- 48.Ziyadeh FN, Hoffman BB, Han DC, Iglesias-De La Cruz MC, Hong SW, Isono M, Chen S, McGowan TA, Sharma K. Long-term prevention of renal insufficiency, excess matrix gene expression, and glomerular mesangial matrix expansion by treatment with monoclonal antitransforming growth factor-beta antibody in db/db diabetic mice. Proc Natl Acad Sci USA. 2000;97(14):8015–8020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kwak MK, Itoh K, Yamamoto M, Kensler TW. Enhanced expression of the transcription factor Nrf2 by cancer chemopreventive agents: role of antioxidant response element-like sequences in the nrf2 promoter. Mol Cell Biol. 2002;22(9):2883–2892. [DOI] [PMC free article] [PubMed] [Google Scholar]