Abstract
Objective
To examine county‐level geographic variation in treatment admissions among opioid treatment programs (OTPs) that accept Medicaid in the continental United States.
Data Sources/Study Setting
Data come from the 2012 National Survey of Substance Abuse Treatment Services.
Study Design/Data Collection
We used local measures of spatial autocorrelation (LISA) analysis to identify (1) clusters of counties with higher and lower than average rates of opioid use disorders and (2) clusters of counties with higher and lower than average treatment admissions among OTPs that accept Medicaid, adjusting for county population size.
Principal Findings
Our results reveal several clusters of counties with higher than average rates of opioid use disorder (OUD) and lower than average treatment admissions among OTPs that accept Medicaid. These clusters are highly concentrated in the Southeast region of the country and include Arkansas, Kentucky, Louisiana, Mississippi, and Tennessee.
Conclusions
Medicaid enrollees in areas in the Southeast have the largest gaps between county‐level OUD rates and estimated county‐level capacity for treatment, as measured by county‐level total treatment admissions among OTPs that accept Medicaid. Policy makers should consider strategies to increase the availability of OTPs with the capacity to serve Medicaid enrollees.
Keywords: Medicaid, opioid use disorder, access, opioid treatment programs
Over the past 15 years, overdose deaths involving opioids have reached epidemic proportions (Rudd et al. 2016). Overdose deaths related to opioid analgesics increased more than threefold from 1999 and 2011 (Chen, Hedegaard, and Warner 2014) and overdose deaths related to heroin more than tripled in just 3 years—from 2011 to 2014 (Rudd et al. 2016). In 2014 alone, opioids were involved in over 28,000 deaths. Despite these staggering increases in deaths related to opioid overdose, the number of prescriptions written for opioid analgesics continues to increase (Volkow et al. 2014).
Medicaid enrollees are disproportionately affected by the opioid epidemic (Centers for Medicare & Medicaid Services 2016). Research indicates that Medicaid enrollees are more than twice as likely as non‐Medicaid populations to be prescribed an opioid analgesic and are six times more likely to die from an opioid overdose (Centers for Disease Control and Prevention 2011). A recent study of Medicaid enrollees in 12 states found that approximately 40 percent of enrollees had at least one indicator of potential inappropriate use or prescription of an opioid analgesic—a rate that is substantially higher than that of the privately insured and Medicare populations (Mack et al. 2015).
Medications for treatment of opioid use disorders (OUDs), used in conjunction with psychosocial treatment, are considered the gold standard treatment for OUDs. There are two commonly used medications to treat OUDs. Methadone is the most widely used medication for OUD treatment in the United States and is dispensed only by licensed opioid treatment programs (OTPs). However, there are only about 1,200 OTPs in the country, and they are unable to meet the demand for OUD treatment (Substance Abuse and Mental Health Services Administration 2012). Buprenorphine, used in conjunction with psychosocial treatment, is also recommended in the treatment of OUDs. While buprenorphine can be prescribed in non‐OTP settings, less than 20 percent of non‐OTP specialty treatment programs prescribed the medication in 2012. Thus, OTPs are a critical access point for OUD treatment including both methadone and buprenorphine in the United States.
The expansion of Medicaid under the Affordable Care Act (ACA) has dramatically expanded the number of enrollees who have coverage for OUD treatment (Mark et al. 2014). Medicaid expansion has increased enrollment by approximately 11.2 million (Sommers et al. 2014; The Henry J. Kaiser Family Foundation 2015c). An estimated 15 percent of newly eligible Medicaid enrollees have some type of substance use disorder (SUD), a rate which is roughly 50 percent higher than that of the general population (The Henry J. Kaiser Family Foundation 2015b). The ACA also expands parity legislation which prohibits limits on the provision of OUD treatment services that are more restrictive than those for medical and surgical services. All state Medicaid agencies—including those that have opted out of expansion—must comply with parity requirements in benchmark and managed care plans.
There is widespread concern that the nation's OTP system may lack the capacity to meet projected growth in demand for services resulting from the ACA. Medicaid enrollment has increased substantially as ACA insurance expansions went into effect. However, at present, relatively few OTPs accept Medicaid enrollees. Less than two‐thirds accept Medicaid, and in many states, such as Arkansas, Louisiana, and Mississippi, there is not a single OTP that accepts Medicaid insurance (Substance Abuse and Mental Health Services Administration 2012). Complicating this challenge is the fact that many OTPs lack the administrative and technological capacity to become certified providers under Medicaid, a requirement for reimbursement. Inability to bill Medicaid and the absence of staff who meet the program's staff licensure requirements are significant challenges to Medicaid participation for many treatment providers. Research also suggests that generosity of state Medicaid benefits may influence rates of Medicaid acceptance among general health care providers and SUD treatment providers (Sloan, Mitchell, and Cromwell 1978; Hadley 1979; Davidson 1982; Gabel and Rice 1985; Perloff, Kletke, and Neckerman 1986; Mitchell 1991; Baker and Royalty 1998; Berman et al. 2002; Terry‐McElrath, Chriqui, and McBride 2011; Andrews 2014).
As a consequence of low rates of Medicaid acceptance among OTPs, there is a possibility that many newly insured Medicaid enrollees could be turned away by providers from whom they seek help—and fail to receive any treatment for their condition. In a recent survey of public agencies that oversee each state's SUD treatment system, only 30 percent reported devoting any resources to encouraging treatment programs in their state to become Medicaid‐certified (Andrews et al. 2015).
Geographic Variation in Treatment Availability
Prior research examining geographic variation in the availability of SUD treatment—including, but not limited to OUDs—in the United States has revealed important gaps in treatment availability, particularly in the South. A set of studies by McAuliffe and colleagues (McAuliffe et al. 2002, 2003; McAuliffe and Dunn 2004) examined state differences in SUD treatment utilization and need and found that Southern and Southwestern states had the largest SUD treatment gaps (McAuliffe et al. 2003; McAuliffe and Dunn 2004). However, these studies did not focus specifically on treatment availability among Medicaid enrollees or focus specifically on access to OUD treatment. A more recent 2009 study examining county‐level access to SUD treatment facilities that serve Medicaid enrollees found that 40 percent of U.S. counties did not have a single outpatient SUD treatment provider that accepted Medicaid insurance. The authors also found that rural counties in the South and Midwest were more likely to lack access to SUD treatment providers that accepted Medicaid, as were counties with higher percentages of black residents (Cummings et al. 2014). Prior research also reveals wide state‐level variation in potential buprenorphine treatment capacity (Jones et al. 2015) and county‐level access to buprenorphine‐waivered physicians (Rosenblatt et al. 2015).
While prior research demonstrates significant variability in the availability of SUD treatment in general and potential access to buprenorphine‐waivered physicians across the United States, questions remain regarding how availability of OUD treatment in OTPs for Medicaid enrollees may differ across regions of the United States at the county level. While prior studies report on differences in overall SUD treatment capacity by county, they do not account for differences in the number of clients served by treatment programs; nor do they account for treatment need. Perhaps most important, they do not focus specifically on OUD treatment. In light of the opioid epidemic in the United States, policy makers need _targeted information to address the problem most effectively.
To address these gaps in prior literature, we examine geographic variation in OUD treatment need and admissions in OTPs that accept Medicaid enrollees. We improve upon prior research by employing a more nuanced measure of treatment capacity that accounts for total service capacity of OTPs that accept Medicaid as well as county population. Using local measures of spatial autocorrelation (LISA), we identify county‐level geographic clusters of high and low rates for admissions among Medicaid accepting OTPs and OUD treatment need.
Methods
To conduct the study, we used data from the 2012 National Survey of the Substance Abuse Treatment Services (N‐SSATS) (Substance Abuse and Mental Health Services Administration 2012). N‐SSATS is an annual census of SUD treatment facilities in the United States and includes 95 percent of all such facilities. The Inventory of Substance Abuse Treatment Services (I‐SATS) provides the sampling frame for N‐SSATS and includes facilities that are licensed or certified by the state to provide SUD treatment, as well as other private for‐profit providers, small group practices, or hospital‐based programs that provide SUD treatment. In 2012, the N‐SSATS response rate was 93 percent, and the final sample size included 1,151 OTPs from 465 counties across the 48 contiguous states and the District of Columbia. N‐SSATS data were linked to U.S. county population data from the 2010 U.S. Census Bureau, data on state‐level rates of OUD from the 2012 National Survey on Drug Use and Health (NSDUH) restricted file (Jones et al. 2015), and data on 2012 county‐level opioid overdose death rates from the Centers for Disease Control and Prevention (CDC) (Centers for Disease Control and Prevention 2016).
We estimate state‐level rates for OUDs taken from the NSDUH restricted file (Jones et al. 2015). To create county‐level estimates from these data, we use a geographic technique called dasymetric mapping, which uses available small‐scale data to weight the disaggregation of data at a larger scale (Eicher and Brewer 2001; Mennis 2015). We use the estimated state OUD rate to estimate the total number of state residents with OUDs.
To disaggregate this figure to the county level, we examine the number of opioid overdose deaths at the county level, available from the CDC's Wonder database (Centers for Disease Control and Prevention 2016). CDC reports county‐level opioid overdose data when the sum of deaths is 10 or more. In counties falling under this threshold, we apply the national median death rate (0.1499 per 1,000) to the county population to create a county‐level estimate. First, we sum county deaths to the state level and then calculate the overdose deaths in each county as a percentage of all deaths within the state. Second, we use this percentage with our variable of interest—state‐level OUD population—to create county‐level estimates, assuming that the overall state pattern of OUDs follows the same geographic distribution as opioid overdose deaths. We then standardize the population of persons with OUDs, calculating a rate per 1,000 residents.
To compare the distribution of the availability of OUD treatment for Medicaid enrollees (rate of admissions to OTPs that accept Medicaid insurance) and OUD treatment need (estimated rate of OUDs), we create county‐level maps for the continental United States (Figures 1 and 2). We then identify clustering of high and low values using LISA (Anselin 1995), calculated through the freely available GeoDa software package (v. 1.4.1) (Chicago, IL, USA). LISA compares the actual geographic distribution of a variable with multiple other permutations of the value distribution, identifying regions where clusters of high or low values were unlikely to happen by chance. Figure 3 shows the results of this analysis. For comparison, we also use LISA analysis to identify clustering of high and low values of the rate of admissions to all OTPs (including those that do not accept Medicaid insurance) (also shown in Figure 3). In addition, we calculated the ratio of OTP admissions to OUD treatment need; however, due to the high number of counties in the United States without an OTP that accepts Medicaid (49 percent of U.S. counties do not have an OTP that accepts Medicaid), this ratio was not meaningful.
Figure 1.
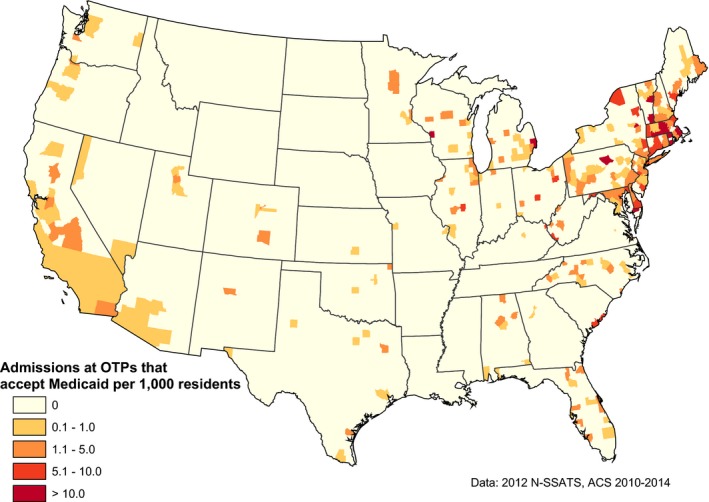
Admissions to OTPs That Accept Medicaid Insurance per 1,000 Residents in the County [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2.
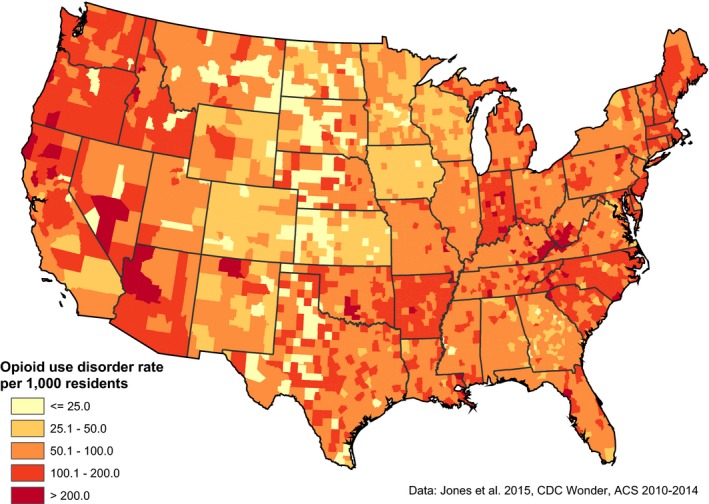
Rate of Opioid Use Disorders per 1,000 Residents, Weighted by County Opioid Overdose Death Rates [Color figure can be viewed at wileyonlinelibrary.com]
Figure 3.
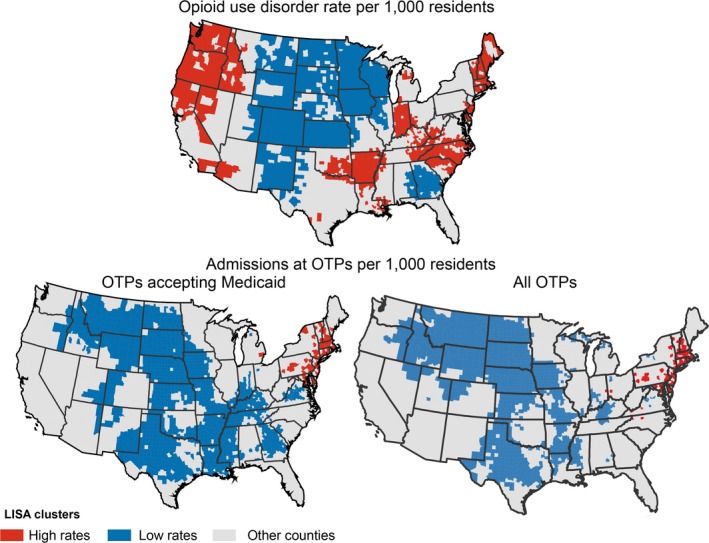
The LISA Clusters: Rate of Opioid Use Disorders per 1,000 Residents in County, Rate of Admissions to OTPs That Accept Medicaid Insurance per 1,000 Residents in County, and Rate of Admissions to All OTPs per 1,000 Residents in the County [Color figure can be viewed at wileyonlinelibrary.com]
Results
Of the 1,151 of OTPs included in the analysis, 744 accepted Medicaid (64.6 percent). Population‐adjusted county OTP treatment admissions were distributed disproportionately across the United States. The overall distribution of OTP treatment capacity is shown in Figure 1 as rate per 1,000 residents. Most counties have no access to OUD treatment in OTPs for Medicaid enrollees, with the most notable gaps in coverage found in the Great Plains—Idaho, Montana, North and South Dakota, Nebraska, and Wyoming—and portions of the Southeast—Arkansas, Louisiana, Mississippi, and Tennessee. The highest rates of OUD treatment are found in New England and southern California, as well as counties surrounding Chicago and Detroit.
Geographic variation in the OUD rate, shown in Figure 2, follows a somewhat different pattern, with four clusters of high values located in sections of New England, Appalachia into Indiana, northwestern Arkansas and Oklahoma, and sections of western states including Arizona, Washington, Oregon, California, and Idaho. The lowest OUD rates are found in the Great Plains and upper Midwest: states such as Iowa, Kansas, Minnesota, North and South Dakota, and Wisconsin. These maps show the value of a county‐level approach, as several states, such as Kentucky and West Virginia, show strong internal variation rates, and high values often straddle state boundaries.
Figure 3 shows the distribution of LISA clusters by county for rates of OUDs (top map), total admissions among OTPs that accept Medicaid (bottom left map), and total admissions among all OTPs (bottom right map). Clusters of high values for OUDs (top map), shown in red (mean = 128.60, range = 83.33–487.60), were found in several areas outlined above—the Pacific Northwest, Arkansas and its neighbors, Appalachia, and sections of New England. Much of the north central United States is part of a cluster of low values, shown in blue (mean = 43.75, range = 0.00–83.02), as well as parts of Texas and the Southeast.
In contrast, clusters of high values for admissions to OTPs that accept Medicaid (bottom left map), shown in red (mean = 4.74, range = 0.28–54.59), are found only in coastal New England. Much of the central United States is part of a cluster of low values, shown in blue (mean = 0.0005, range 0.00–0.24); this band stretches from Montana and Idaho down through Texas and Georgia. Several areas with high OUD rates correspond to low treatment capacity among OTPs that accept Medicaid, particularly in the South, including a large majority of Arkansas and sections of Kentucky, Louisiana, Mississippi, and Tennessee. Only in sections of New England do we find counties with significant clustering of high values for both OUD rate and high treatment capacity among OTPs that accept Medicaid. Correlation using Spearman's rho found a positive association of 0.05, a small although significant figure. We attribute this to shared low values in the Great Plains and some overlap of high values in New England.
Figure 3 also shows clusters of high and low values for the rate of admissions per 1,000 residents for all OTPs (bottom left map). When comparing these results to OTPs that accept Medicaid (bottom right map), there are no longer clusters of low values in many sections of the South (particularly Georgia and Tennessee) and the four corners area of the Southwest.
Discussion
The results of this study indicate significant county‐level variation in total OUD treatment admissions for Medicaid enrollees across the United States and that these differences are not linked to any discernible pattern of variation in rates of OUDs. This finding is aligned with prior studies that highlight important disparities in SUD treatment availability, particularly in southern portions of the country (McAuliffe et al. 2003; McAuliffe and Dunn 2004; Cummings et al. 2014). In particular, we identified several areas of the South—including portions of Arkansas, Kentucky, Louisiana, Mississippi, and Tennessee—as areas where high OUD rates correspond to low treatment admissions for OUDs among OTPs that accept Medicaid. LISA analysis including all OTPs lends support to our finding that access to OTPs that accept Medicaid is particularly problematic in the South.
Three possible factors may influence lower OUD treatment availability for Medicaid enrollees in the Southeast. First, counties in these states are significantly less likely to have any OTPs. Second, the South has the highest concentration of for‐profit SUD treatment providers in the country—over 60 percent of which refuse treatment to Medicaid enrollees (Substance Abuse and Mental Health Services Administration 2012). Third, state Medicaid coverage for SUD treatment has traditionally been less generous in Southern states (Substance Abuse and Mental Health Services Administration 2012; Grogan et al. 2016). A broad base of research has documented lower rates of Medicaid acceptance in states with less generous coverage for health care services, including SUD treatment (Sloan, Mitchell, and Cromwell 1978; Hadley 1979; Davidson 1982; Gabel and Rice 1985; Perloff, Kletke, and Neckerman 1986; Mitchell 1991; Baker and Royalty 1998; Berman et al. 2002; Terry‐McElrath, Chriqui, and McBride 2011; Andrews 2014). However, even in southern states where methadone is not covered by Medicaid, buprenorphine and many additional services offered by OTPs are covered (e.g., assessment, counseling, case management) (Grogan et al. 2016). Assessing the causal factors underlying low OUD treatment admissions in the Southeast remains a topic for future research.
Our results suggest that Arkansas, the only state in Deep South that has expanded Medicaid, and Louisiana, which recently opted to expand Medicaid, may need to increase infrastructure to provide opioid treatment services to both preexpansion and newly enrolled Medicaid beneficiaries. As the traditional Medicaid plan in Arkansas provides limited coverage of SUD treatment (The Henry J. Kaiser Family Foundation 2015a), many providers may not have experience with Medicaid and may lack Medicaid reimbursement‐eligible staff. In Louisiana, the estimated percentage of the Medicaid expansion population with an SUD is 18.8 percent—well above the national average (The Henry J. Kaiser Family Foundation 2015b). It will be important to closely monitor how Medicaid enrollees are faring in accessing OUD treatment in these states.
Our findings also have implications for racial disparities in access to OUD treatment in U.S. states located in the South, which have among the highest percentages of black residents in the nation. Black Americans are also more likely to be enrolled in Medicaid than members of other racial and ethnic groups. Consequently, Black Americans may be more likely to be adversely affected by lower OUD treatment admissions in the Southeast. This finding adds to literature examining contextual factors that can explain racial disparities in access to SUD treatment (McAuliffe et al. 2003; McAuliffe and Dunn 2004; Guerrero and Kao 2013; Cummings et al. 2014). Our findings also suggest that the industrial organization of the SUD treatment system—and specifically, the extent of penetration of for‐profit treatment programs within each state's system—may contribute to these challenges.
Our results also indicate areas of high OUD treatment need and low treatment capacity for Medicaid enrollees in large sections of Oklahoma, Indiana, Idaho, and a small section of Oregon's eastern boarder. While Idaho and Oklahoma have opted not to expand Medicaid, both Indiana and Oregon have expanded Medicaid. Thus, both traditional Medicaid enrollees in these states and newly eligible Medicaid enrollees in Indiana and Oregon may face challenges when seeking treatment in OTPs.
We identified only one area of the country with geographic clusters of high rates for both OUDs and high opioid treatment capacity for Medicaid enrollees—New England. Specifically, rates of OUDs and OUD treatment admissions were high in parts of Connecticut, Massachusetts, New Hampshire, New Jersey, Vermont, Rhode Island, and the entire state of Delaware. In this region of the country, OTPs are much more likely to be nonprofit, to accept Medicaid, and to serve a large number of clients annually (Substance Abuse and Mental Health Services Administration 2012).
Limitations
This study has several limitations. First, our data were measured at the county level, limiting our ability to examine within‐county variation in availability of OUD treatment for Medicaid enrollees. Second, we relied on estimates of the actual number of clients served in OTPs. Treatment admissions may change from year to year, and we were unable to account for any such changes. Related to this issue, we are unable to account for local factors that may influence admissions. For example, we could not account for differences in propensity for help‐seeking among people with OUDs in different counties. Third, we only measured OUD treatment admissions in OTPs. Consequently, we cannot account for OUD treatment in other settings, such as non‐OTP specialty treatment programs and primary care and mental health centers that do not have programs specific to OUD treatment. Fourth, we were unable to account for buprenorphine‐waivered physicians in the state or county in our analyses. Data on acceptance of Medicaid insurance by buprenorphine‐waivered physicians are not currently available. However, only 2.2 percent of physicians in the United States have obtained a waiver to prescribe buprenorphine; a majority of counties in the United States do not have any buprenorphine‐waivered physicians (Rosenblatt et al. 2015); and a small percentage of persons with SUDs receive care in office‐based settings (Substance Abuse and Mental Health Services Administration 2014).
Conclusions
The findings of this study highlight significant county‐level variation in OUD rates and OUD treatment admissions in OTPs that accept Medicaid in the United States. Several geographic areas of the United States may face challenges in meeting current and future demand for OUD treatment among Medicaid enrollees. While most of the states with the lowest OUD treatment admissions among OTPs that accept Medicaid are located in states that have not elected to expand Medicaid, this is likely to change in the years ahead. It is likely that more states will elect to expand Medicaid under the ACA option over the next several years—including states in the South, which have been particularly vocal in resisting ACA‐driven policy change.
Research suggests several promising strategies for increasing the availability of OUD treatment for Medicaid enrollees. First, several states have relatively few or no OTPs (e.g., Idaho, Mississippi, Oklahoma). For these states, the first step is simply to establish OTPs. Second, it will be critical to identify and address barriers to obtaining Medicaid certification among OTPs. This may include technical assistance to support OTPs in developing technology to submit insurance reimbursement claims and create electronic health record systems as well as training to improve licensure and credentialing up to the standards of state Medicaid agencies. Third, public agencies might consider offering incentives to nonspecialty SUD treatment providers, such as mental health and primary care providers already certified by Medicaid, to offer OUD treatment, particularly buprenorphine and naltrexone, which can be prescribed in non‐OTP settings. Increasing the availability of OUD treatment in these settings has the potential to simultaneously increase treatment access and promote service integration. Finally, prior research demonstrates that SUD treatment providers in states with more generous coverage for SUD are more likely to accept Medicaid enrollees (Sloan, Mitchell, and Cromwell 1978; Hadley 1979; Davidson 1982; Gabel and Rice 1985; Perloff, Kletke, and Neckerman 1986; Mitchell 1991; Baker and Royalty 1998; Berman et al. 2002; Terry‐McElrath, Chriqui, and McBride 2011; Andrews 2014). Thus, improvements in state Medicaid coverage for OUD treatment spurred by the ACA and parity legislation may serve as incentives to some OTPs to accept Medicaid enrollees.
In the face of a growing opioid epidemic, federal policy makers are calling for increased access to medications for the treatment of OUDs (i.e., methadone, buprenorphine, naltrexone) as part of a comprehensive strategy to combat the opioid epidemic. This call is particularly salient for state Medicaid programs as the Medicaid population is disproportionately impacted by the opioid epidemic. While all state Medicaid programs now cover buprenorphine and almost all states cover injectable naltrexone, 19 state Medicaid programs do not cover methadone under their fee‐for‐service plan (Grogan et al. 2016). These states include Arkansas, Idaho, Indiana, Kentucky, Oklahoma, and Tennessee, which are all characterized by low OTP treatment capacity for Medicaid enrollees and high OUD rates. In fact, a recent study found that a significantly higher percentage of clients in treatment for OUDs received opioid agonist therapy in states with Medicaid coverage of methadone (Saloner, Stoller, and Barry 2016). Medicaid enrollees in states without Medicaid coverage of methadone are likely forced to pay out‐of‐pocket for the medication or are simply unable to access methadone. Thus, increasing Medicaid coverage of methadone is critical. Other promising strategies include encouraging more OTPs that accept Medicaid insurance to prescribe buprenorphine and naltrexone and/or increase their existing capacity to treat patients with methadone, particularly in areas with great need.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors acknowledge Kevin C. Remington for his contribution to data analysis. The authors acknowledge the University of Georgia and University of South Carolina for their support.
Disclosures: None.
Disclaimer: None.
References
- Andrews, C. M. 2014. “The Relationship Between State Medicaid Coverage to Medicaid Acceptance among Substance Abuse Providers in the United States.” Journal of Behavioral Health Services & Research 41 (4). [DOI] [PubMed] [Google Scholar]
- Andrews, C. , Abraham A., Grogan C. M., Pollack H. A., Bersamira C., Humphreys K., and Friedmann P.. 2015. “Despite Resources from the ACA, Most States Do Little to Help Addiction Treatment Programs Implement Health Care Reform.” Health Affairs (Millwood) 34 (5): 828–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anselin, L. 1995. “Local Indicators of Spatial Association‐LISA.” Geographical Analysis 27 (2): 93–115. [Google Scholar]
- Baker, L. , and Royalty A. B.. 1998. “Medicaid Policy, Physician Behavior, and Health Care for the Low‐Income Population.” Journal of Human Resources 35 (3): 480–502. [Google Scholar]
- Berman, S. , Dolins J., Tang S. F., and Yudkowsky B.. 2002. “Factors That Influence the Willingness of Private Primary Care Pediatricians to Accept More Medicaid Patients.” Pediatrics 110 (2 Pt 1): 239–48. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2011. Policy Impact: Prescription Painkiller Overdoses. Atlanta, GA: National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. [Google Scholar]
- Centers for Disease Control and Prevention . 2016. “WONDER Online Databases” [accessed on May 1, 2016]. Available at http://wonder.cdc.gov
- Centers for Medicare & Medicaid Services . 2016. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. CMCS Informational Bulletin. Baltimore, MD: Centers for Medicare & Medicaid Services. [Google Scholar]
- Chen, L. , Hedegaard H., and Warner M.. 2014. “Drug‐Poisoning Deaths Involving Opioid Analgesics: United States, 1999–2011.” National Center for Health Statistics Data Brief No. 166. Hyattsville, MD. [PubMed] [Google Scholar]
- Cummings, J. R. , Wen H., Ko M., and Druss B. G.. 2014. “Race/Ethnicity and Geographic Access to Medicaid Substance Use Disorder Treatment Facilities in the United States.” Journal of the American Medical Association Psychiatry 71 (2): 190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson, S. M. 1982. “Physician Participation in Medicaid: Background and Issues.” Journal of Health Politics, Policy and Law 6 (4): 703–17. [DOI] [PubMed] [Google Scholar]
- Eicher, C. L. , and Brewer C. A.. 2001. “Dasymetric Mapping and Areal Interpolation: Implementation and Evaluation.” Cartography and Geographic Information Science 28 (2): 125–38. [Google Scholar]
- Gabel, J. R. , and Rice T. H.. 1985. “Reducing Public Expenditures for Physician Services: The Price of Paying Less.” Journal of Health Politics, Policy and Law 9 (4): 595–609. [DOI] [PubMed] [Google Scholar]
- Grogan, C. M. , Andrews C. A., Abraham A. J., Humphreys K., Pollack H. A., Smith B., and Friedmann P. D.. 2016. “Survey Highlights Differences in Medicaid Coverage for Substance Use Treatment and Opioid Use Disorder Medications.” Health Affairs 35 (12): 2289–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero, E. G. , and Kao D.. 2013. “Racial/Ethnic Minority and low‐Income Hotspots and Their Geographic Proximity to Integrated Care Providers.” Substance Abuse Treatment, Prevention, and Policy 8: 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley, J. 1979. “Physician Participation in Medicaid: Evidence from California.” Health Services Research 14 (4): 266–80. [PMC free article] [PubMed] [Google Scholar]
- The Henry J. Kaiser Family Foundation . 2015a. “A Look at the Private Option in Arkansas.” Issue Brief. J. Guyer, N. Shine, M. Musumeci, and R. Rudowitz: The Henry J. Kaiser Family Foundation.
- The Henry J. Kaiser Family Foundation . 2015b. “Many People with Substance Abuse Problems May Find Few to Treat Them.” C. Vestal: Kaiser Health News.
- The Henry J. Kaiser Family Foundation . 2015c. “Recent Trends in Medicaid and CHIP Enrollment as of January 2015: Early Findings from the CMS Performance Indicator Project.” S. Artiga, R. Rudowitz, A. Gates, and L. Snyder: The Henry J. Kaiser Family Foundation.
- Jones, C. M. , Campopiano M., Baldwin G., and McCance‐Katz E.. 2015. “National and State Treatment Need and Capacity for Opioid Agonist Medication‐Assisted Treatment.” American Journal of Public Health 105 (8): e55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack, K. A. , Zhang K., Paulozzi L., and Jones C.. 2015. “Prescription Practices Involving Opioid Analgesics among Americans with Medicaid, 2010.” Journal of Health Care for the Poor and Underserved 26 (1): 182–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark, T. L. , Levit K. R., Yee T., and Chow C. M.. 2014. “Spending on Mental and Substance Use Disorders Projected to Grow More Slowly Than All Health Spending through 2020.” Health Affairs (Millwood) 33 (8): 1407–15. [DOI] [PubMed] [Google Scholar]
- McAuliffe, W. E. , and Dunn R.. 2004. “Substance Abuse Treatment Needs and Access in the USA: Interstate Variations.” Addiction 99 (8): 999–1014. [DOI] [PubMed] [Google Scholar]
- McAuliffe, W. E. , Woodworth R., Zhang C. H., and Dunn R. P.. 2002. “Identifying Substance Abuse Treatment Gaps in Substate Areas.” Journal of Substance Abuse Treatment 23 (3): 199–208. [DOI] [PubMed] [Google Scholar]
- McAuliffe, W. E. , LaBrie R., Woodworth R., Zhang C., and Dunn R. P.. 2003. “State Substance Abuse Treatment Gaps.” American Journal on Addictions 12 (2): 101–21. [PubMed] [Google Scholar]
- Mennis, J. 2015. “Dasymetric Spatiotemporal Interpolation.” Professional Geographer 124: 1–11. [Google Scholar]
- Mitchell, J. B. 1991. “Physician Participation in Medicaid Revisited.” Medical Care 29 (7): 645–53. [DOI] [PubMed] [Google Scholar]
- Perloff, J. D. , Kletke P. R., and Neckerman K. M.. 1986. “Recent Trends in Pediatrician Participation in Medicaid.” Medical Care 24 (8): 749–60. [DOI] [PubMed] [Google Scholar]
- Rosenblatt, R. A. , Andrilla C. H., Catlin M., and Larson E. H.. 2015. “Geographic and Specialty Distribution of US Physicians Trained to Treat Opioid Use Disorder.” Annals of Family Medicine 13 (1): 23–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd, R. A. , Aleshire N., Zibbell J. E., and Gladden R. M.. 2016. “Increases in Drug and Opioid Overdose Deaths — United States, 2000–2014.” MMWR. Morbidity and Mortality Weekly Report 64 (50–51): 1378–82. [DOI] [PubMed] [Google Scholar]
- Saloner, B. , Stoller K. B., and Barry C. L.. 2016. “Medicaid Coverage for Methadone Maintenance and Use of Opioid Agonist Therapy in Specialty Addiction Treatment.” Psychiatric Services (Washington, DC) 67 (6): 676–9. [DOI] [PubMed] [Google Scholar]
- Sloan, F. , Mitchell J., and Cromwell J.. 1978. “Physician Participation in State Medicaid Programs.” Journal of Human Resources 13 (Suppl): 211–45. [PubMed] [Google Scholar]
- Sommers, B. D. , Musco T., Finegold K., Gunja M. Z., Burke A., and McDowell A. M.. 2014. “Health Reform and Changes in Health Insurance Coverage in 2014.” New England Journal of Medicine 371 (9): 867–74. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2012. National Survey of Substance Abuse Treatment Services. Bethesda, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2014. National Survey on Drug Use and Health. Bethesda, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Terry‐McElrath, Y. M. , Chriqui J. F., and McBride D. C.. 2011. “Factors Related to Medicaid Payment Acceptance at Outpatient Substance Abuse Treatment Programs.” Health Services Research 46 (2): 632–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow, N. D. , Frieden T. R., Hyde P. S., and Cha S. S.. 2014. “Medication‐Assisted Therapies—Tackling the Opioid‐Overdose Epidemic.” New England Journal of Medicine 370 (22): 2063–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


