Using meta-analysis to explore clinical determinants for death of COVID-19 patients has been a problem due to insufficient sample size and overlapped cases [1]. In the study, we re-analyzed the largest confirmed case series reported publicly by the Chinese center for disease control and prevention (44,672 laboratory confirmed cases updated through February 11, 2020, [2]), to explore the clinical risk factors associated with death.
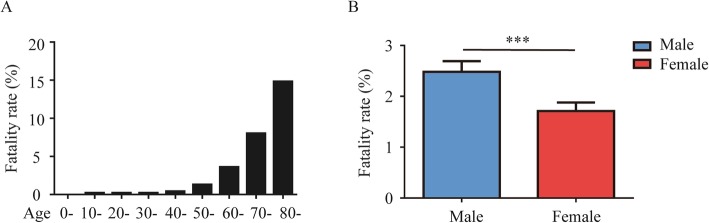
The basic characteristics between survivors and non-survivors with COVID-19 were presented in Table 1. Among a total of 44,672 patients with laboratory confirmation of SARS-CoV-2 infection, 1023 (2.3%) patients were dead as of February 11, 2020, the last day of follow-up. The fatality rate was increasing with ages and even up to 14.8% in patients aged above 80 years old (see Fig. 1a). The prevalence of COVID-19 between men and women was pretty close (51.4% vs. 48.6%), which is different from previous report (58.1% vs. 41.9%) [3]. Notably, the fatality rate of male patients was significantly higher than that of female patients (RR = 1.67, 95%CI = 1.47–1.89, p < 0.001) (see Fig. 1b). Furthermore, cardiovascular disease (RR = 6.75, 95%CI = 5.40–8.43, p < 0.001), hypertension (HR = 4.48, 95%CI = 3.69–5.45, p < 0.001), diabetes (RR = 4.43, 95%CI = 3.49–5.61, p < 0.001), respiratory disease (RR = 3.43, 95%CI = 2.42–4.87, p < 0.001), and cancers (RR = 2.926, 95%CI = 1.34–6.41, p = 0.006) were the risk factors for fatality of patients with COVID-19.
Table 1.
Characteristics between survivors and non-survivors with COVID-19
| Characteristics | Total (n = 44,672) | Non-survivors (n = 1023) | Survivors (n = 43,649) | Fatality (%) | RR (95%CI) | p |
|---|---|---|---|---|---|---|
| Age, n (%) | ||||||
| 0– | 416 (0.9%) | 0 | 416 (0.9%) | 0 | ||
| 10– | 549 (1.2%) | 1 (0.1%) | 548 (1.3%) | 0.2 | ||
| 20– | 3619 (8.1%) | 7 (0.7%) | 3612 (8.3%) | 0.2 | ||
| 30– | 7600 (17.0%) | 18 (1.8%) | 7582 (17.4%) | 0.2 | ||
| 40– | 8571 (19.2%) | 38 (3.7%) | 8533 (19.5%) | 0.4 | ||
| 50– | 10,008 (22.4%) | 130 (12.7%) | 9878 (22.6%) | 1.3 | ||
| 60– | 8583 (19.2%) | 309 (30.2%) | 8274 (19.0%) | 3.6 | ||
| 70– | 3918 (8.8%) | 312 (30.5%) | 3606 (8.3%) | 8.0 | ||
| ≥ 80 | 1408 (3.2%) | 208 (20.3%) | 1200 (2.7%) | 14.8 | ||
| Severity*, n (%) | ||||||
| Mild/moderate | 36,160 (80.9%) | 0 | 36,160 (82.8%) | 0 | ||
| Severe | 6168 (13.8%) | 0 | 6168 (14.1%) | 0 | ||
| Critical | 2087 (4.7%) | 1023 (100%) | 1064 (2.4%) | 49.0 | ||
| Gender, n (%) | ||||||
| Male | 22,981 (51.4%) | 653 (63.8%) | 22,328 (51.2%) | 2.8 | 1.67 (1.47–1.89) | < 0.001 |
| Female | 21,691 (48.6%) | 370 (36.2%) | 21,321 (48.8%) | 1.7 | ||
| Comorbidity#, n (%) | ||||||
| Hypertension | 2683 (12.8%) | 161 (39.7%) | 2522 (12.3%) | 6.0 | 4.48 (3.69–5.45) | < 0.001 |
| Diabetes | 1102 (5.3%) | 80 (19.7%) | 1022 (5.0%) | 7.3 | 4.47 (3.49–5.61) | < 0.001 |
| Cardiovascular disease | 873 (4.2%) | 92 (22.7%) | 781 (3.8%) | 10.5 | 6.75 (5.40–8.43) | < 0.001 |
| Respiratory disease | 511 (2.4%) | 32 (7.9%) | 479 (2.3%) | 6.3 | 3.43 (2.42–4.87) | < 0.001 |
| Cancer | 107 (0.5%) | 6 (1.5%) | 101 (0.5%) | 5.6 | 2.93 (1.34–6.41) | 0.006 |
*Missing data (n = 257 in survivors group)
#Missing data (n = 617 in the non-survivors group, n = 23,073 in the survivors group)
Fig. 1.
Fatality rate distribution of age (a) and gender (b). ***p < 0.001
In summary, we found that there was no difference in the prevalence of COVID-19 between men and women, but male patients had a nearly 1.7-fold higher risk of death than female patients. Moreover, we concluded that patients with comorbidities had a significantly high death risk. Admittedly, due to the unavailability of individual patient data, we could not exclude the influence of age on the conclusion because old patients were more likely to have the underlying comorbidities. We would like to provide a reminder to the physicians that more intensive surveillance or treatment should be considered for male patients and those with comorbidities. Further and larger studies are needed to validate the findings.
Acknowledgements
None.
Authors’ contributions
GD and FZ conceptualized the idea and designed the study. MY and XC revised the manuscript. The authors read and approved the final manuscript.
Funding
This work was supported by the grants from the National Natural Science Foundation of China (No. 81620108024).
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bauchner H, Golub RM, Zylke J. Editorial concern-possible reporting of the same patients with COVID-19 in different reports. JAMA. 2020. 10.1001/jama.2020.3980. [DOI] [PubMed]
- 2.Novel Coronavirus Pneumonia Emergency Response Epidemiology T The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. [Google Scholar]
- 3.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.