Abstract
Doxorubicin (DOX) constitutes the major constituent of anti-cancer treatment regimens currently in clinical use. However, the precise mechanisms of DOX’s action are not fully understood. Emerging evidence points to the pleiotropic anticancer activity of DOX, including its contribution to DNA damage, reactive oxygen species (ROS) production, apoptosis, senescence, autophagy, ferroptosis, and pyroptosis induction, as well as its immunomodulatory role. This review aims to collect information on the anticancer mechanisms of DOX as well as its influence on anti-tumor immune response, providing a rationale behind the importance of DOX in modern cancer therapy.
Keywords: adriamycin, apoptosis, DNA damage response (DDR), doxorubicin, immunotherapy
1. Introduction
Drugs used in chemotherapy can be categorized into several groups according to a variety of criteria, including their function and chemical framework. Depending on the mode of action, they can be categorized as alkylating agents, antimetabolites, topoisomerase inhibitors, mitotic spindle inhibitors, and others [1,2,3]. Topoisomerase I inhibitors, such as irinotecan and topotecan, and topoisomerase II inhibitors, such as etoposide, teniposide, and anthracyclines (idarubicin, daunorubicin, and doxorubicin (DOX)), induce DNA strand breaks and hinder the action of topoisomerases that are involved in the DNA replication and process of transcription [3]. DOX has been demonstrated to have significant therapeutic potential and is recognized as one of the most efficient chemotherapy medications that have been approved by the Food and Drug Administration (FDA) for the treatment of various cancers such as breast cancer, carcinomas, sarcomas, and hematological malignancies [4]. Despite the extensive application of anthracyclines, the toxic effects of these drugs are multifaceted, with cardiotoxicity being the most well-known and most comprehensively studied adverse effect, as reviewed by multiple authors [4,5,6,7,8,9,10]. Moreover, damage to other organs [11,12,13], including the brain [12,14,15], liver [16], and kidneys [17,18,19], can also occur. It is already known that the anticancer activity of DOX can be attributed to the capability of the drug to intercalate into DNA, inhibit topoisomerase II, disrupt mitochondria function, and potentiate free-radical generation and oxidative damage. However, the precise mechanisms of action of DOX are complex and still relatively unknown [4,12,20]. There have been many initiatives attempted to lessen the adverse effects of DOX, including the use of substances that possess antioxidant and/or antiapoptotic activity [17,21,22,23,24,25], the creation of efficient delivery systems [12,26,27,28,29,30,31,32], prodrugs [33,34,35,36,37,38], and the development of DOX analogues [39,40,41,42,43], as recently reviewed by Sohali et al. [44]. On the other hand, some of these techniques were not successful in reducing the toxic effects of anthracycline when tested in animal models or in human clinical trials [45,46,47,48,49,50,51]. It is important to make an effort to find more efficient methods of combating DOX toxicity while maintaining or strengthening its therapeutic effects [4].
Despite the side effects induced by DOX it is still widely used in cancer therapy, predominantly in new formulations (mentioned above) or drug combinations [52,53,54,55,56]. In addition to their cytotoxic effect, chemotherapeutic drugs may also boost the infiltration of CD8+ T cells and neutral killer (NK) cells into tumors, as well as the maturation of antigen-presenting cells (APCs), such as tumor macrophages or dendritic cells. Primary cytostatic and cytotoxic medicines function in this way to restore an immune-reactive tumor microenvironment, which ultimately increases the tumor’s susceptibility to immunotherapy. Moreover, many of the medicines that are presently in use have not been investigated in terms of their potential to activate the immune system against tumor cells or for their value in combinations with immune checkpoint inhibitors [57].
Here we review new insights into the DOX mode of action including its contribution to DNA damage, reactive oxygen species (ROS) production, apoptosis, senescence, autophagy, ferroptosis, and pyroptosis induction, as well as the emerging influence of this anthracycline drug on the immune system and antitumor immune response.
2. Mode of Action
2.1. Induction of DNA Damage
2.1.1. Formation of DOX–DNA Adducts and DNA Intercalation
Like other anthracyclines, DOX intercalates DNA through the formation hydrogen bonds with guanines in adjacent GC base pairs [58,59]; however, the exact mechanism of this interaction is not completely understood. One of the postulated mechanisms to explain the effect of DOX on malignant cells is that the intercalation of DOX into DNA untwists the molecule and results in positive supercoiling of the DNA helix [60,61]. There is also evidence that DOX increases the turnover of nucleosomes surrounding promoters of active genes due to its intercalation and induces changes in DNA topology [61,62]. It is possible that the unwinding of DNA that occurs as a result of DOX intercalation provides a significant amount of positive torsional stress that destabilize nucleosomes [63].
Moreover, it has been demonstrated that the formation of DOX–DNA adducts can activate the DNA damage response (DDR) pathway independently of the effect of the drug on topoisomerase II. Importantly, DOX–DNA adducts can be detected at drug doses that are appropriate to clinical practice, which suggests that DOX–DNA adducts can be formed when chemotherapy is applied [64,65,66]. However, the formation of adducts seem not to be the primary action mechanism of DOX [66].
2.1.2. Topoisomerase Trapping
During DNA replication and transcription, topoisomerases play a crucial role in the preservation of the correct DNA structure. Supercoiled DNA emerging during the above-mentioned processes can unwind and efficiently function as a template upon the introduction of single- or double-strand breaks (SSBs or DSBs) by topoisomerase type I and II enzymes, respectively [67]. Topoisomerase II enzyme is possibly the main _target of DOX; however, topoisomerase I inhibition may also play a role in DOX cytotoxicity. Low dosages (<1 µM) of DOX are believed to capture covalently bound topoisomerase II at DNA ds-breaking sites and inhibit DNA relegation [68,69]. Furthermore, the treatment of cancer cells with DOX induces up-regulation of genes of the DDR pathway [61] as a consequence of the induction of SSBs and DSBs in the DNA molecule [70].
Ataxia telangiectasia and Rad3-related (ATR) was discovered in 1996 as the mammalian orthologue of mitotic entry checkpoint protein 1, also known as Mec1. Mec1 is the primary kinase that is responsible for the coordination of DNA damage checkpoints in budding yeast. Structurally, ATR is a phosphoinositide 3-kinase-related protein kinase (PIKK) essential for cell viability due to its major role in the coordination of pathways involved in the replication stress response [71,72,73]. ATR can react to a wide variety of genotoxic stresses, such as those caused by UV radiation, DNA polymerase inhibitors, or topoisomerase poisons. One characteristic that is shared by all of these stressors is the fact that they stop or delay DNA polymerases in replication forks [74]. ATR detects single-stranded DNA (ssDNA) emerging at halted replication forks as a result of minichromosome maintenance (MCM2-7)-complex helicase activity. ATR kinase present in cells as an inactive dimer becomes active upon autophosphorylation reaction in response to DNA damage emergence. Replication protein A/ATR-interacting protein (RPA-ATRIP) complexes are generated on single-stranded DNA and act as a platform for the ATR kinase. Moreover, topoisomerase 2-binding protein 1 (TOPBP1) and the RAD9-RAD1-HUS1 components of the 9-1-1 cell-cycle checkpoint control protein complex are also necessary for the complete activation of the kinase [75,76,77,78,79]. Furthermore, additional factors including the MRE11–RAD50–NBS1 (MRN) complex and RAD9, RAD1, HUS1 interacting nuclear orphan (RHINO) may be involved in the recruitment of TOPBP1 for efficient activation of the ATR kinase [74]. Recent research has shown that Ewing’s tumor-associated antigen 1 (ETAA1) protein also has an ATR-activating domain. In contrast to the embryonically lethal effects of a TOPBP1 impairment in mice, the carriers of ETAA1 mutations are viable [71,72].
SSBs are detected by the poly (ADP-ribose) polymerase 1 (PARP1), which associates with the ends of the strand breaks and creates complexes with tyrosyl-DNA phosphodiesterase 1 (TDP-1), X-ray repair cross-complementing group-1 (XRCC1), and polynucleotide kinase phosphatase (PNKP). The above-mentioned factors are recruited to the sites of SSB for efficient removal of non-canonical DNA ends. For example, TDP1 catalyzes the conversion of 3′-phosphotyrosyl bonds to the 3′-OH ends, while PNKP removes the phosphate groups from the 3′-end and catalyzes the phosphorylation of the 5′-hydroxyl groups of DNA, reconstructing the regular (3′-OH and 5′-P) DNA strand ends [78,80]. Nonetheless, PARP-1 constitutes the central hub protein of the response to single-strand DNA breaks and single-strand break repair (SSBR). PARP-1 is involved in the recognition and signaling of occurring damage and catalyzes an evolutionarily conserved enzymatic reaction that involves attachment of poly (ADP-ribose) polymers (PARs) to arginine, glutamate, aspartate, cysteine, lysine, and serine residues of many adaptor proteins and histones at the sites of DNA damage. This leads to the efficient recruitment of DNA repair factors to the relaxed chromatin [76,78,81,82,83,84], including cellular tumor antigen p53 (TP53), DNA ligase III, XRCC1, DNA-dependent protein kinase catalytic subunit (DNA-PKCS), and KU70/80 [84].
Upon detection of DSBs, cells respond by rapidly and precisely relocating a wide variety of proteins to the area around the lesion. These proteins assemble into massive, overlapping multi-subunit structures called foci. Sequestration of proteins in the DSB’s immediate vicinity may play a role in increasing the damage-induced checkpoint signal and easing the repair of persistent damage [85]. DSBs are detected and processed by the MRN complex. The meiotic recombination 11 homolog 1 (MRE11) complex component works as both a DNA endonuclease and a 3′–5′ dsDNA exonuclease that mediates the resection of aberrant DNA structures such as hairpins, while RAD50 and nibrin (NBS1) stimulate the activity of the nuclease. The MRN concentration at the site of DNA damage serves as a signal for ataxia telangiectasia mutated A-T mutated (ATM) recruitment [85,86,87]. ATM, similar to ATR, exists in cells as an inactive dimer that undergoes monomerization in response to DNA damage. Activated ATM phosphorylates exposed H2AX histone proteins in the vicinity of DSBs, leading to the accumulation of phosphorylation on Ser-139 H2AX (γ-H2AX) histone foci, which serve as an anchorage for the platform protein mediator of DNA damage checkpoint protein 1 (MDC-1). The recruitment of MDC-1 contributes to the further accumulation of ATM at the damage site and amplification of the signal through phosphorylation of H2AX proteins and accumulation of MDC-1 [76,78].
DNA-PKcs constitutes another DDR central hub protein along with ATR and ATM kinases and also belongs to the PIKK family. In contrast to the ATM-mediated pathway, which facilitates DNA repair through the homologous recombination pathway (HR), the detection of DSBs by KU70/80 proteins and formation of the repair complexes with DNA-PKcs favors the repair of occurring breaks by the non-homologous end joining (NHEJ) pathway. Besides its role in the canonical NHEJ pathway, DNA-PKcs participates in replication stress through the phosphorylation of ATR-activating RPA32 protein on Ser-4 and -8 and subsequent activation of the replication checkpoints [88,89] described below.
In the following events, ATR and ATM phosphorylate checkpoint kinases (CHK1 and CHK2), which mediate the downstream events of the DDR. Checkpoint kinases phosphorylate M-phase inducer phosphatases (CDC25A and CDC25C), which control cell-cycle progression through the dephosphorylation of cyclin–cyclin-dependent kinase (CDK) complexes. CDK4 and CDK6 become active following exposure to mitogens and facilitate the cell-cycle entrance by the deactivation of retinoblastoma protein (pRB), which is implicated in transcriptional regulation in mammalian cells. In contrast, complexes composed of CDK1/CDK2/cyclin A are necessary for the progression of the cell cycle into the S phase. CDKs in a phosphorylated state are unable to fulfill their function, which leads to cell-cycle arrest [77,90,91]. Moreover, besides the downstream role of CDKs in DDR, these kinases control the activity of the upstream components and _target RPA, ATRIP, MDC-1, NBS1, ATM, and CHK1 for phosphorylation, as previously reviewed by our group [77]. Moreover, CHK2 phosphorylates TP53, a protein regarded as the guardian of the genome, which controls the expression of proapoptotic genes (including proapoptotic protein BAX) and inhibitors of antiapoptotic proteins (including phorbol-12-myristate-13-acetate-induced protein 1 (NOXA) and isoform 1 of Bcl-2-binding component 3, isoforms 1/2 (PUMA)), contributing to apoptosis induction, or cyclin-dependent kinase inhibitors (including P21), conferring cell-cycle arrest [78,92].
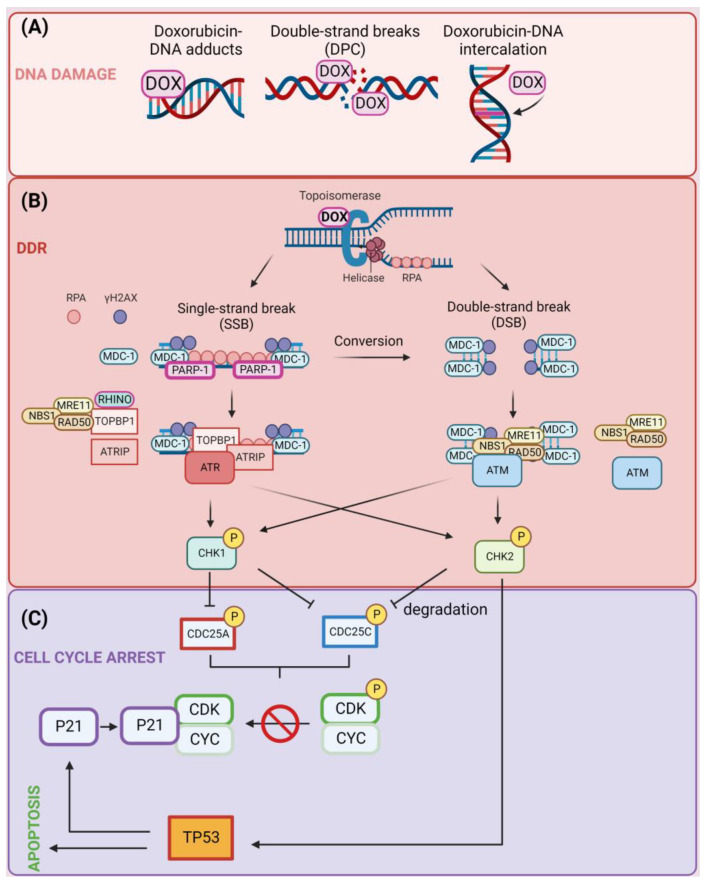
Treatment of cells with DOX induces ATM autophosphorylation on Ser-1981, its activation, and ATM-mediated phosphorylation of multiple _targets, including NBS1, CHK1, and CHK2. Ascorbic acid treatment does not affect DOX-induced TP53 phosphorylation and accumulation, while preincubation of cells with the hydroxyl radical scavenger N-acetylcysteine attenuates DOX-mediated phosphorylation of TP53, H2AX, NBS1, CHK1, and CHK2. This suggests that hydroxyl radicals contribute to DOX-induced activation of ATM-dependent pathways [93]. Moreover, activation of CHK2 in DOX-treated cells may be independent of ATM or ATR activation [94]. In acute lymphoblastic leukemia, DOX treatment results in cell-cycle arrest in the G2/M phase of the cell cycle via activation of the ATR-CHK1 pathway. The combination of ATR-CHK1 inhibition with DOX treatment results in the synergistic cytotoxic activity that is associated with aberrant chromosome segregation and mitotic spindle defects in cells [95]. Furthermore, inhibition of the DDR pathway components including ATM [96], ATR [97], CHK1/2 [98,99,100], DNA-PKcs [101], and PARP-1 [102] sensitizes cancer cells to DOX treatment. DNA damage caused by topoisomerase II inhibition leads to a G1 and G2 cell-cycle arrest and eventual induction of the apoptosis process [103,104,105,106]. The induction of DNA damage (A), DDR (B), and the contribution of these events to apoptosis or cell-cycle arrest (C) are presented in Figure 1.
Figure 1.
(A) Induction of DNA damage following treatment of cells with doxorubicin (DOX). DOX induces DNA damage through three main mechanisms: the formation of DNA adducts, single-strand break (SSB) induction, and double-strand break (DSB) induction, in which DNA strands remain bound to trapped topoisomerase enzymes through DNA–protein crosslinks (DPCs) and intercalation of DOX in the DNA molecule. (B) Activation of DNA damage response (DDR) pathway. Trapping of topoisomerase enzymes by DOX induces the formation of either SSBs or DSBs. SSBs are detected by poly [ADP-ribose] polymerase 1 (PARP-1), and the ssDNA is covered with replication protein A (RPA). This results in the recruitment of a variety of factors including DNA topoisomerase 2-binding protein 1 (TOPBP-1), RAD9, RAD1, HUS1 interacting nuclear orphan (RHINO), ATR-interacting protein (ATRIP), MRE11–RAD50–NBS1 complexes, and serine/threonine-protein kinase ATR that contribute to the formation of γH2AX protein foci at the sites of damage. DSBs are detected by MRN complexes, which recruit a mediator of DNA damage checkpoint protein 1 (MDC-1) and amplification of the foci formation by ataxia telangiectasia mutated (A-T mutated) (ATM) kinase. Consequently, ATR and ATM kinases phosphorylate checkpoint kinases CHK1 and CHK2. (C) Induction of apoptosis or cell-cycle arrest by DOX. The CHK1/2-mediated phosphorylation of CDC25A/C phosphatases leads to their degradation and as a consequence no dephosphorylation of CDK-cyclin complexes that prevent cell-cycle progression. Alternatively, CHK2 phosphorylates and activates cellular tumor antigen p53 (TP53) transcription factor leading to up-regulation of P21, which binds unphosphorylated (active) CDK–cyclin complexes and contributes to cell-cycle arrest. Created with BioRender.com accessed on 1 January 2023.
2.2. Apoptosis–ROS Interplay
Reactive oxygen species (ROS) can be generated in aerobic organisms through the electron transport chain (ETC), the action of catabolic oxidases, and the metabolism of peroxisomes [107]. ROS normally function as cellular messengers in redox signaling events when their concentrations are kept relatively low [108]. Nevertheless, an excessive generation of ROS can contribute to DNA damage through the action of radicals on DNA bases and the sugar–phosphate backbone [109,110]. Unrepaired damage can lead to apoptosis [111,112], cell-cycle arrest [113,114], and senescence [115,116,117,118].
DOX binds directly to cardiolipin on the inner mitochondrial membrane, where it initiates a process of ROS production [119,120,121]. High amounts of ROS cause substantial damage to the mitochondrial structure, which ultimately results in cell apoptosis [122]. In cardiac cells, mitochondria-derived ROS and calcium play an important role in the stimulation of DOX-induced intrinsic and extrinsic forms of apoptosis. This stimulation occurs through the nuclear factor of activated T-lymphocytes (NFAT)-mediated FAS antigen ligand (FASL) up-regulation and down-regulation of FLICE/caspase-8 inhibitory protein (FLIP) [123]. In a study evaluating DOX’s influence on death ligands in induced-pluripotent-stem-cell-derived cardiomyocytes, death receptors including tumor necrosis factor receptor 1 (TNFR1), FAS, and death receptor 5 (DR5) were up-regulated and apoptosis was exacerbated by TNF-related apoptosis-inducing ligand (TRAIL) [124,125]. DOX’s severe cardiotoxicity [126,127] and thrombocytopenia [128] side effects severely restrict its therapeutic utility. DOX induces cardiotoxicity via multiple routes [129,130,131,132], as previously reviewed by multiple authors [7,9,133,134,135]; however, excessive production of ROS and reactive nitrogen species (RNS) constitutes the main mechanism of cardiotoxicity of anthracyclines [136].
The ATM can be also activated by ROS without the involvement of MRN complexes and in the absence of DSBs, as was determined in cells exposed to hydrogen peroxide [137]. The activation of ATM as a consequence of ROS accumulation does not involve the classical DDR response. Some enzymes, such as peroxiredoxin-2 (PRDX2) and thioredoxin-1 (TRX1), can chemically alter cysteine (Cys-2991) residues on ATM when the level of ROS reaches a certain threshold. This leads to the generation of intermolecular disulfide bonds and the activation of ATM dimers. When this disulfide bond formation is prevented (by ATM mutation), the amount of ATM that is activated by ROS is decreased, while the activation route mediated by the MRN complex appears to be unaffected. The notion that ROS are capable of activating ATM independently on MRN complexes is supported by the finding that the activation of ATM by ROS can be impeded by the addition of a reducing agent [137,138,139]. ATM dimers generated in response to ROS exposure still retain their function and can contribute to the phosphorylation of CHK2 and as a consequence activation of the apoptosis pathway [138].
The mechanisms of DOX-induced apoptosis as well as the involvement of ROS in apoptotic signaling were evaluated in osteosarcoma Saos-2 cells. A 48 h treatment of cells with DOX resulted in the accumulation of cells in the pre-G1 phase and induction of DNA laddering, both of which are characteristic features of apoptosis. Additionally, DOX caused an increase in the generation of hydrogen peroxide and superoxide followed by depolarization of the mitochondrial membrane, the release of cytochrome c, and the activation of the caspase-3 enzyme. Furthermore, the DOX treatment caused an increase in the levels of proapoptotic BAX protein and a decrease in the levels of antiapoptotic BCL-2 protein. The fact that catalase was able to inhibit DOX-induced ROS generation, mitochondrial cytochrome c release, procaspase-3 cleavage, and apoptosis in Saos-2 cells provided further evidence that ROS play a role in DOX-induced cancer-cell death. The findings of the above-mentioned research revealed that ROS might function as the signal molecules for DOX-induced cell death, and the mechanism may be functional despite the absence of TP53 [140]. Similar results were obtained in MCF-7 breast cancer cells, where treatment with DOX induced BAX protein expression with concomitant caspase-8 and caspase-3 elevation and down-regulation of BCL-2 protein. Moreover, the treatment with the chemotherapeutic agent increased the generation of hydrogen peroxide with a decrease in nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) expression. In contrast, the increase in superoxide dismutase (SOD2) expression contributed to the diminishment of hydrogen peroxide production with a decrease in NF-κB protein expression in the MDA-MB-231 breast cancer cell line [141]. It is hypothesized that the greater amounts of superoxide that are detected during DOX administration are caused by a decrease in the activity of enzymes that are responsible for the decomposition of superoxide, such as SOD2 and catalases [142]. Treatment of cervical cancer cells (CaSki and SiHa cell lines) with cisplatin and DOX results in different profiles of types of ROS induced following drug administration. Cisplatin treatment results in the generation of hydrogen peroxide, hydroxyl, and peroxyl radicals, while DOX induces the production of superoxides [143]. A similar tendency was observed in HaCaT keratinocytes, where DOX induced superoxide production with no increase in hydrogen peroxide, hydroxyl, or peroxyl radicals. This study also pointed out that the diminished antiapoptotic function of the BCL-2 protein may result from its ubiquitination and proteasomal degradation [144]. Alternatively, down-regulation of GATA binding protein 4 (GATA4) can result in a decrease in antiapoptotic B-cell lymphoma-extra large (BCL-xL) protein [145]. Ehrlich tumor cells treated with DOX experience excessive superoxide anion production in tumor microsomes and nuclei. Rotenone (ETC complex I interferer) was shown to boost the formation of drug-stimulated superoxide by mitochondria. This suggests that the proximal section of the ETC in tumor cells is responsible for the reduction of the DOX quinone. These studies also show that anthracyclines are capable of considerably boosting oxygen radical metabolism in Ehrlich tumor cells and this may contribute to the cytotoxicity and apoptotic properties of agents belonging to this class of compounds [146].
Lipid peroxidation, the oxidative destruction of lipid membranes, has been linked to oxidative stress. This procedure generates about 200 different kinds of aldehydes, many of which are highly reactive. The mutagenic and carcinogenic effects of these aldehydes are due to their capacity to react with DNA or to form pro-mutagenic exocyclic adducts and protein–DNA crosslinks, which can halt both DNA replication and transcription [147,148,149]. Lipid peroxidation was observed following DOX administration [150,151,152]; however, the contribution of lipid peroxidation to DOX cytotoxicity is controversial, as previously reviewed [153].
Another possible mode of action of DOX includes the overproduction of ceramide [154,155], which contribute to ROS generation, DNA damage, and apoptosis [6,129,156,157,158,159]. Ceramides were reported to trigger the release of proapoptotic proteins from the mitochondria through the development of vast protein-permeable channels through which proapoptotic proteins (including cytochrome c, procaspases, apoptosis-inducing factor (AIF), heat shock proteins, the secondary mitochondria-derived activator of caspases (SMAC)/direct inhibitor of apoptosis-binding protein with low pI (DIABLO), and endonuclease G) are released. Mitochondria contain the enzymes necessary for the synthesis and hydrolysis of ceramide. There is also evidence that mitochondrial ceramide levels are increased just before the induction phase of apoptosis [160,161,162]. Khodadust et al. found that a dendrimeric (PIC-G4-DOX) nanoformulation of DOX up-regulates the expression of genes encoding the proapoptotic proteins NOXA, PUMA, and BAX, while down-regulating the expression of survivin, APOLLON, and BCL-2 in the MCF-7 cancer cell line. This formulation also increased the cytotoxic activity of DOX toward the MCF-7 cancer cell line. According to the findings, PIC-G4-DOX has the potential to be effective for _targeted delivery that can impact apoptotic pathways, which ultimately leads to a higher degree of cancer-cell killing. The Polyinosinic:polycytidylic acid [Poly (I:C)] component of the PIC-G4-DOX nanoformulation acts similarly to an RNA virus and triggers the intrinsic apoptosis pathway of cancer cells. Following receptor-mediated endocytosis, the synthetic double-stranded RNA is detected in the cytoplasm by a class of ubiquitous cytoplasmic RNA helicases called retinoic acid inducible gene-I (RIG-I) and melanoma differentiation Ag-5 (MDA-5) initiates an antiviral signaling cascade via the adaptor protein mitochondrial antiviral signaling (MAVS). The activation of TP53 as a result of stress stimuli leads to the activation of BAX, which in turn activates the intrinsic apoptotic pathway. BAX achieves this activation via up-regulating PUMA and NOXA. After being activated, proapoptotic BAX causes the mitochondria to become depolarized, which in turn causes the release of cytochrome c into the cytoplasm. After forming an apoptosome by creating a complex with apoptosis protease activation factor (APAF-1), cytochrome c and pro-caspase 9 lead to caspase 9 activation, which in subsequent events activates effector caspase 3. The activation of the transcription factor nuclear factor kappa B (NF-kB) and interferon regulatory factors (IRFs) such as IRF-3 as a result of MAVS-dependent signaling triggers the production of inflammatory cytokines and chemokines, including type I interferons (IFNs). Activation of RIG-I and subsequent downstream MAVS signaling can induce transcription of the proapoptotic BH3-only proteins NOXA and PUMA independent of TP53. This results in the activation of the intrinsic apoptotic pathway, in which BAX functions to disrupt the integrity of the mitochondrial membrane, which in turn leads to the release of cytochrome c, formation of an apoptosome, caspase 3 activation, and apoptosis. Because of its stability, biocompatibility, increased rate of internalization, and toxicity, PIC-G4-DOX shows promise as potential anticancer agent [163].
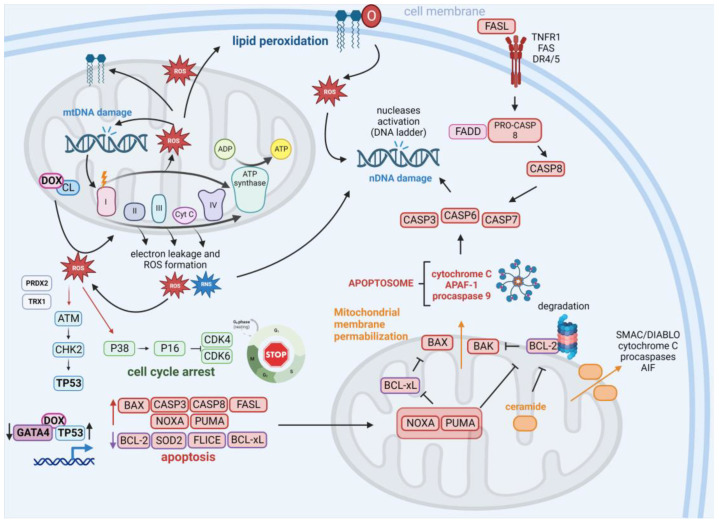
Inconsistency exists on the role of TP53 in DOX-induced apoptosis. While some studies confirm the participation of TP53 in this process, others seem to contradict these finding. Discrepancies in the methodologies utilized for the exploration of TP53’s role in DOX-mediated apoptosis and heterogeneity of the tumors that were evaluated in these studies could be accountable for these conflicting results, as previously reviewed [153]. The contribution of DOX to ROS induction and apoptosis is presented in Figure 2.
Figure 2.
Contribution of DOX to ROS induction and apoptosis. The interaction of DOX with cardiolipin (CL) leads to the elevation of reactive oxygen species (ROS) and reactive nitrogen species (RNS) levels, which contribute to DNA damage of nuclear (nDNA) and mitochondrial DNA (mtDNA). DNA damage and mutations in mtDNA encoding proteins of the electron transport chain (ETC) lead to the production of defective ETC components that increase electron leakage and ROS/RNS generation. Alternatively, ROS trigger lipid peroxidation, enhancing ROS pools in the cells. ROS may trigger the activation of the ATM-CHK2-TP53 signaling independently of DNA damage through ROS-mediated ataxia telangiectasia mutated A-T mutated (ATM) dimer formation through modification of enzyme cysteine residues by peroxiredoxin-2 (PRDX2) and thioredoxin-1 (TRX1). Through the P38 protein, ROS may activate the P16 protein, which works as an inhibitor of cyclin-dependent kinases 4/6 (CDK4/CDK6). DOX increases the expression of cellular tumor antigen p53 (TP53) and down-regulates the expression of GATA binding protein 4 (GATA4), which influences the expression of genes under the control of these transcription factors. Consequently, an increase in multiple proapoptotic proteins (including BAX, caspase 3/8 (CASP3/8), FAS antigen ligand (FASL), phorbol-12-myristate-13-acetate-induced protein 1 (NOXA), and isoform 1 of Bcl-2-binding component 3, isoforms 1/2 (PUMA)) is observed in addition to a decrease in antiapoptotic factors (such as cyclin D1, B-cell lymphoma-extra large (BCL-xL), and FLICE). The observed down-regulation of BCL-xL and apoptosis regulator Bcl-2 (BCL-2) activity can be attributed to the inhibitory activity of NOXA and PUMA and the antiapoptotic protein proteasomal degradation. Alternatively, activation of ceramide signaling together with mitochondrial pore formation (through BAX and BAK proteins) and the loss of mitochondrial integrity confer the release of proapoptotic factors including cytochrome c, apoptotic protease-activating factor 1 (APAF1), and procaspase-9 (leading to apoptosome formation), the secondary mitochondria-derived activator of caspases (SMAC)/direct inhibitor of apoptosis-binding protein with low pI (DIABLO), apoptosis-inducing factor 1, mitochondrial (AIF), and pro-caspases. Apoptosome activity contributes to the activation of effector caspases (CASP3, -6, and -7) that execute the final phase of apoptosis and lead to the activation of nucleases that cleave nDNA (leading to DNA laddering observed following treatment of cells with DOX). DOX also induces the extrinsic apoptosis pathway via up-regulation of FASL, its interaction with the death receptors tumor necrosis factor receptor 1 (TNFR1), FAS, and death receptor 5 (DR5), and activation of CASP8 and effector caspases. Created with BioRender.com accessed on 1 January 2023.
2.3. Senescence Induction
It is well known that cancer cells treated with chemotherapeutics can enter senescence. As a result, therapy-induced senescence (TIS) has emerged as an advantageous method for combating cancer with minimal side effects. Emerging evidence suggests that the senescence of cancer cells can be undesirable due to the propensity of senescent cells to establish a pro-cancerogenic milieu. To deal with senescent cells, researchers have created a new drug class called senolytics, which specifically remove senescent cells [164].
The characteristic features of senescent cells include cell-cycle arrest, expression of senescence-associated β-galactosidase, heterochromatin foci formation, telomere shortening, hyper-methylation of histone H3K9, and secretion of multiple factors including chemokines and inflammatory factors such as MMPs, IL-1, IL-6, and IL-8 (the so-called senescence-associated secretory phenotype; SASP) [165]. This topic was recently reviewed by multiple authors [166,167].
DOX-induced senescence was established as the primary mechanism of therapeutic activity of the drug in the FU-SY-1 synovial sarcoma cell line [168]. Bojko et al. studied the effects of DOX (concentration of 100–200 nM) on different cancer-cell lines (non-small-cell lung cancer (A549), neuroblastoma (SH-SY-5Y), colon (HCT116), and breast cancer (MDA-MB-231 and MCF-7)). Growth arrest, induction of DSBs, up-regulation of P21, and ATM activation (the latter was not activated in HCT116 cells) was shown following drug treatment [164]. This is consistent with the earlier finding on DDR activation and senescence induction in cells treated with DOX [169]. Moreover, NF-κB activation in response to the activity of ATM could contribute to the development of SASP in DOX-treated cells. Furthermore, the induction of senescence in the examined cells was found to be dependent on the cell line used in the experiment [170,171]. As opposed to ATM and DNA-PKsc, ATR kinase activity cannot be entirely replaced by other PIKKs, as demonstrated in previous experiments by the same authors, making it essential for the development of senescence. Furthermore, the authors demonstrated that knocking down the NF-κB component, P65, abolished SASP induction but did not affect other markers of senescence and DDR signaling, demonstrating that SASP is independently controlled by NF-κB activated in other ways than the classical PIKK signaling cascade [169]. Furthermore, the same team evaluated the senescence induction in HCT116 cells treated with low doses of DOX. Increased expression of TP53, P21, and cyclin D1 accompanied by polyploidization through endoreduplication was found following the drug treatment [172].
Intimate cross-talk between senescence, epithelial–mesenchymal transition (EMT), and autophagy exist. Hu et al. observed time-dependent DOX-induced senescence activation in HeLa cells accompanied by elevated expression of IL-6 and IL-8. Due to DOX’s ability to trigger EMT, cancer cells acquire enhanced motility and resistance to chemotherapy (as the expression of pro-inflammatory IL-8 and CDK inhibitory protein p16INK4a were inversely related to that observed for vimentin). This study, therefore, indicated that EMT could suppress senescence induced by DOX [165]. This is consistent with the finding that DOX-induced senescence encourages stemness and tumorigenicity in a hepatocellular carcinoma cell line (HuH-7) [173] or induces autophagy in the myelogenous leukemia cell line (K562) [174].
Multiple other studies have also shown that DOX may also trigger senescence in normal cells, including fibroblasts [175], microglia cells [176], cardiac progenitor cells [177], cardiomyocytes [178,179], mesenchymal stem cells [180], and thymus cells [181]. This should be taken into account when investigating the potential anti-tumor activity of DOX related to senescence induction.
2.4. Other Types of Cell Death
Autophagy is a cellular catabolic degradation response that occurs in response to cell famine or stress. This reaction involves the engulfment, digestion, and recycling of cellular proteins, organelles, and cytoplasm to maintain cellular metabolism. The process of autophagy has a dualistic role in cancer. Catabolism through autophagy is beneficial to cellular survival. However, an imbalance in cell metabolism, which occurs when autophagic cellular consumption surpasses the cellular capacity for synthesis, encourages the death of cells. This can be partially explained by the encouragement of necrotic cell death and an inflammatory response that occurs in tumors that have abnormalities in both autophagy and apoptosis. Loss of the pro-survival role of autophagy is known to promote the development of tumors [182]. Autophagy was found to hamper DOX-induced apoptosis in osteosarcoma [183] and confer the chemoresistance to DOX in MCF-7 cells [184]. The induction of autophagy by rapamycin in the presence of DOX increases cardiac cell viability, decreases apoptosis and ROS production, and refines mitochondrial function in vitro and in vivo [185]. In contrast, inhibition of autophagy escalates the cytotoxicity of DOX in MDA-MB-231 and MCF-7 breast cancer cells [186,187] and prostate cancer cells [188].
Ferroptosis was indicated as another mechanism of DOX-induced cardiotoxicity. DOX causes an increase in the cell’s labile iron pool, which contributes to its cytotoxicity. DOX and its metabolites have the potential to disrupt iron homeostasis through their ability to inactivate iron regulatory proteins 1 and 2 (IRP1 and IRP2). The expression of genes involved in iron metabolism can be altered as a result of the binding of inactive IRPs to iron-response elements (IREs). By inhibition of GPX4 in both the cytosol and the mitochondria, DOX causes lipid peroxidation, which in turn results in ferroptosis. Alternatively, DOX contributes to the activation of nuclear factor erythroid 2-related factor 2 (NRF-2), which elicits ferroptosis. This topic was previously reviewed [189]. In line with these findings, nanoparticles consisting of DOX and exogenous ferritin were developed. The nanoparticles induced ROS formation and ferroptosis of HT-29 cells [190]. Similarly, other formulations including microenvironment-activatable Fe–DOX preloaded amorphous CaCO3 nanoparticles [191] and iron–DOX prodrug-loaded liposomes [192,193] were developed. Induction of ferroptosis, a relatively newly identified mechanism of cell death, can take place as a result of lipid peroxidation that is mediated by the Fenton reaction. The effectiveness of Fenton-reaction-dependent ferroptosis is, however, hindered in tumor cells by low levels of hydrogen peroxide and elevated levels of glutathione [192,194].
Pyroptosis is an inflammatory form of programmed cell death with a dualistic role in cancer. On the one hand, pyroptosis, in its role as an inflammatory cell-death process, creates an environment that is favorable for the growth of tumors. On the other, an over-activation of pyroptosis can limit the growth of tumor cells [195,196]. Caspase-1, -4, -5, and -11 are involved in the execution of pyroptosis. When caspase-1 is activated, the preforms of IL-1β, IL-18, and gasdermin D (GSDMD) are processed into active forms. In contrast to caspase-1, which is triggered by pyroptotic sensors such as the NLR family pyrin domain containing 3 (NLRP3) inflammasome, caspase-4, -5, and -11 are activated when they directly attach to lipopolysaccharides. In the past, it has been noted that NLRP3 is significant with regard to the cardiotoxicity of DOX, as discussed earlier [189,197]. Moreover, DOX caused a significant decrease in mouse muscular function, which was connected with a considerable increase in the NLRP3 inflammasome and the initiation marker toll-like receptor 4 (TLR4). When compared to the controls, there was a considerable rise in the pyroptosis activator known as apoptosis-associated speck-like protein containing a caspase recruitment domain (ASCO), which was accompanied by overexpression of certain pyroptosis markers (caspase-1, IL-1, and IL-18) [198]. When breast cancer cells were treated with DOX, the cell viability was decreased in a dose-dependent manner. Additionally, pyroptosis morphology was elicited in MDA-MB-231 and T47D cells. GSDME seems to be a crucial regulator of DOX-induced pyroptosis. In addition to this, DOX treatments caused an increase in the amount of ROS, activation of the C-Jun N-terminal kinase (JNK) signaling pathway, and activation of caspase-3 [199]. Pyroptosis was triggered by DOX at concentrations ranging from 0.5 to 5 µmol/L in melanoma cell lines SK-MEL-5, SK-MEL-28, and A-375 that had high levels of deafness, autosomal dominant 5, isoform CRA a (DFNA5) expression, but not in the human breast cancer cell line MCF-7, which had low levels of DFNA5 expression. On the other hand, treatment with DOX prompted melanoma cells to begin the process of autophagy and the use of an autophagy inhibitor triggered the pyroptosis of cells. In DOX-treated human melanoma cells, eukaryotic elongation factor-2 kinase (eEF-2K) directs the cross-talk between pyroptosis and autophagy. The absence of eEF-2K results in the inhibition of autophagy and enhancement of pyroptosis, which contributes to the modification of the sensitivity of melanoma cells to DOX. This finding suggests that _targeting eEF-2K may enhance the antitumor activity of DOX [200].
3. DOX and Tumor–Immune Microenvironment
Through many mechanisms involving coordination between innate and adaptive immune responses, the body can recognize cancer cells and eradicate them. The role of T cells in this process is crucial. When stimulated, these cells contribute to an immune response that _targets cancer cells. For T cells to become engaged, a specific peptide epitope of the antigen must be presented on the major histocompatibility complex (MHC) of an APC, and then form a complex with the T-cell receptor on T cells. T-cell activation requires a second signal produced by the binding of co-stimulatory molecules [201]. The process is complex and involves tumor-cell recognition, recruitment of APCs, antigen uptake and its processing, APC maturation, antigen presentation to T lymphocytes, production of stimulatory factors including interferons (IFNs, including IFNγ), and engagement of cytotoxic CD8+ T lymphocytes [202]. Moreover, the coinhibitory receptor PD-1 can be constitutively expressed or activated in myeloid, lymphoid, normal epithelial cells, and cancer. Programmed death ligand 1 (PD-L1) represents the main ligand of the PD-1 receptor. The PD-1/PD-L1 association is crucial in the establishment of immunological tolerance under normal conditions, where it serves to suppress excessive immune cell activity that could otherwise cause tissue damage and autoimmune response. Cancer cells, however, utilize PD-L1 to avoid detection by the immune response [203].
Conventional chemotherapy’s impact on the immune system is becoming increasingly recognized. This is because most studies evaluating the efficacy of such drugs against cancer cells are conducted in vitro or on immune-compromised animals and do not include immunological follow-ups [204]. DOX not only exhibits direct cytotoxic effects on cancer cells, but also utilizes the immune system to kill cancer cells by triggering CD8+ T-cell responses [205]. Moreover, pre-treatment with DOX in cancer patients may be an effective strategy to boost anti-cancer immune responses by increasing antigen-specific CD4+ Th1 immune responses [206,207]. The incubation of cancer cells with DNA-damaging agents, including the topoisomerase inhibitors camptothecin [208], DOX [209,210,211], and irinotecan [212] or the alkylating agents carboplatin [213,214], cisplatin [215,216,217,218,219], and oxaliplatin [220], leads to up-regulation of PD-L1. In response to drugs that cause DSBs, including etoposide or ionizing radiation, the ATM/ATR/CHK1 pathway is activated, which causes PD-L1 expression to increase. In addition, PD-L1 expression levels return to normal in cells that escape death after being exposed to ionizing radiation, suggesting that the up-regulation of this immune checkpoint protein in response to DNA damage is only temporary [221]. In addition, DSBs activate the interferon regulatory factor 1 (IRF1) and signal transducer and activator of transcription 1/3 (STAT1/3) transcription factors. Notably, IRF1 is necessary for PD-L1 overexpression, which shows that the DSB-dependent up-regulation of PD-L1 is regulated through the traditional JAK1/2-STAT1/2/3-IRF1 pathway [221,222,223,224,225].
DOX treatment induces the up-regulation of immune-related genes of the PD-1/PD-L1 and T-cell cytotoxicity pathways. This is accompanied by the induction of the tyrosine-protein kinase JAK (JAK-STAT) pathway and tumor necrosis factor α (TNF-α) signaling in triple-negative breast cancer patients [210] and can lead to up-regulation of PD-L1 in cancer cells [209]. PD-1/PD-L1 axis blockage together with DOX treatment may help to overcome resistance to DOX treatment and provide clinical benefits for patients [210,226]. It is possible that the up-regulation of PD-L1 in cancer cells could increase the availability of epitopes to which anti-PD-L1 small-molecule compounds and antibodies could bind. This could be one of the explanations for the observed enhanced therapeutic efficacy of the combined treatment of DOX and ant-PD-L1 antibodies [227,228]. In contrast, PD-L1 up-regulation can also confer chemiresistance in malignant cells through the up-regulation of multidrug resistance 1/P-glycoprotein (MDR1/P-GP) in breast cancer cells [229]. Therefore PD-1/PD-L1 inhibition could help to overcome the resistance mechanism to commonly used chemotherapeutic agents [230].
However, the difficulty lies in combining chemotherapeutic medications with anti-PD-L1 compounds to increase the effectiveness of the combined treatment beyond that of the individual treatments and reduce the negative effects of the therapies. A combination of the chemotherapeutic agent with the anti-PD-L1 agent should be chosen not only for its capacity to effectively kill cancer cells and inhibit their growth but also based on its predisposition to modulate the activity of immune-active cells and to preserve the activity of the administered immunotherapy [231]. For instance, PD-L1 expression is increased in bone marrow stromal cells or osteosarcoma cell lines and clinical tissue samples obtained following DOX treatment. DOX prevents CD8+ T-lymphocyte proliferation and also increases the rate of immune-cell apoptosis. The use of an antibody against PD-L1 can revert these diminishing effects on the anti-tumor immune response and lead to elevated tumor-cell apoptosis [211,232]. Pembrolizumab and atezolizumab are examples of two anti-PD-L1 monoclonal antibodies that are frequently paired with DOX to treat a variety of malignancies including triple-negative breast cancer (TNBC). A recent clinical investigation showed a significant elevation of immune-related genes involved in the PD-1/PD-L1 pathway and T-cell cytotoxicity pathways in TNBC patients treated with DOX and cisplatin [210].
Over the years, numerous systems and strategies have been tested for their effectiveness in directing drugs toward tumors. Multiple systems have been developed, including liposomes, polymers, micelles, nanoparticles, and antibody conjugates [233]. The accumulation of antitumor drugs in tumors is enhanced, and the solubility, stability, and bioavailability problems often associated with these agents are avoided through the nanoformulation of drugs into liposomes [234]. The introduction of the liposomal drug-delivery method has had a profound impact on the pharmaceutical industry. Liposomes are synthetic vehicles that can be made using cholesterol and natural, non-toxic phospholipids to generate a spherical vesicle. Liposomes constitute a promising technology for drug delivery because of their size and hydrophobic and hydrophilic properties, which hallow the encapsulation of drugs, low toxicity, and biocompatibility. Passive drug loading occurs when the drug is contained in the liposome during preparation, while active drug loading occurs after the formation of the liposome [235,236].
In 1995, the FDA approved the first liposomal DOX, called Doxil® (injectable DOX hydrochloride liposomes), for the treatment of ovarian cancer, Kaposi’s sarcoma, and myeloid melanoma [236]. The PEGylation of liposomes significantly contributed to the advancement of Doxil in clinical trials. PEGylation refers to the covalent attachment of polyethylene glycol (PEG) to a given molecule. It provides several benefits in drug development: it prolongs the retention time of liposomes in the body and shields them from degradation by intracellular enzymes or other mechanisms active inside the cell [237,238]. Pre-formulation and post-formulation techniques are distinguished as types of liposomal surface modification. Before formulation, phospholipids (often PEGylated) undergo covalent-bond formation with ligands. After conventional lipids are combined with ligand-anchored lipids, the active drug is loaded into the liposomes remotely. Through the addition of transferrin to the distal ends of liposomal PEG chains, Eavarone et al. designed liposomes containing DOX selectively _targeting glioma C6 cells expressing transferrin receptor. This formulation exceeded the uptake efficiency of non-PEG, PEG, and albumin-coupled PEG liposome drug-delivery systems [239]. _targeted liposomal formulations constitute the next generation of liposomal drug-delivery systems and have been created to increase the selectivity of liposomes for cancerous tissues. Considering their great specificity for their _target antigens, antibodies and antibody fragments are the most popular _targeting moieties for liposomes. Interest in antibody-modified liposomes for the _targeted delivery of anticancer drugs is high [240]. Effective treatment of B-cell cancers may involve the monoclonal-antibody-mediated delivery of liposomal anticancer medicines to surface antigens expressed on malignant B cells [241]. Liposomal agents _targeting the internalizing epitopes (such as CD19) are hypothesized to be more effective than those _targeting non-internalizing epitopes (e.g., _targeted against CD20). When comparing DOX-loaded anti-CD20 _targeted liposomes and non_targeted liposomes, DOX-loaded anti-CD19 _targeted liposomes dramatically increased survival times after a single i.v. dosage. It has been thereby empirically established that internalizing epitopes are more beneficial to _target therapeutically than their non-internalizing counterparts [242,243]. Studies on CD22 suggest a multifaceted function for this transmembrane glycoprotein in controlling B-cell survival and proliferation [244]. Through the conjugation of HB22.7 anti-CD22 monoclonal antibody with PEGylated liposomal DOX, an immunoliposomal formulation with increased efficacy and without increased toxicity was generated [245,246].
The FDA’s green light for Doxil® led the way for more liposomal formulations to be used in clinical settings. In addition to Doxil®, another licensed liposomal formulation is Myocet®, which provides the same benefits as Doxil® without displaying hand–foot syndrome (palmar–plantar erythrodysesthesia syndrome), a prominent side effect of pegylated liposomal DOX formulations [247,248,249,250,251]. The generic DOX hydrochloride liposomal injectable Lipodox® has been approved for use in patients [252,253,254]. Studies on other DOX liposomal preparations including Caelyx® [255,256], Thermodox® [257,258], Nudoxa® [259,260], 2B3-101 [261,262,263], and C225-ILS-Dox [264] with unique anticancer efficiencies, tissue distributions, and toxicity profiles have also been conducted. This topic was extensively reviewed by other authors [153,265,266]
Some of the formulations were tested for their beneficial effect on the tumor-directed immune response. For example, chimeric polypeptide DOX nanoparticle formulation boosted the infiltration of leukocytes into the tumor, reducing tumor-cell growth and inhibiting the metastatic potential of 4T1 mammary carcinoma cells of BALB/c mice compared with conventional DOX. These findings demonstrate that a nanoparticle drug is distinct from the free drug in its ability to activate antitumor immunity depending on CD8+ T-cell stimulation and IFN-γ production [267]. In addition, the number of immunosuppressive tumor-associated macrophages (TAMs) in the tumor bed is reduced by DOX treatment. STAT1-deficient mice, on the other hand, show decreased T-cell activation and reduced T-cell infiltration of the tumor in response to drug treatment and show resistance to lapatinib and/or DOX’s effects on tumor growth. Additionally, STAT1 deficiency leads to decreased production of C-X-C motif chemokine receptors (CXCL9, CXCL10, and CXCL11) in the tumor epithelium, all of which work as T-cell chemotactic factors, suggesting STAT is an important contributor to DOX’s effects on the antitumor immune response [268]. Increased numbers of CD8+ T lymphocytes and suppression of metastasis are observed in dendritic-cell infusion and DOX treatment of mice with metastatic tumors. DOX-treated mice exhibit higher levels of calreticulin (CRT). CRT is a protein that resides in the endoplasmic reticulum (ER), and it plays an important role in the regulation of calcium homeostasis as well as glycoprotein folding in the ER. Additionally, the protein has been found on the cell surface of necrotic and apoptotic cells, where it is thought to play a part in immunogenic cell death as well as other extracellular functions. Following an exposition on the apoptotic cell, CRT interacts with the CD91 receptor on DCs, playing an important role in cancer-cell recognition by the immune system [269,270]. Additionally, high mobility group box protein B1 (HMGB1) expression is also increased following the treatment of cells with DOX [271]. HMGB1 is a nuclear molecule that is typically secreted from necrotic cells. It is believed that HMGB1 is involved in the structural organization of DNA. After being released into the extracellular space, HMGB1 acts as a mediator of the inflammatory response. This could enhance the anti-tumor immune response. Apoptotic cells, on the other hand, typically do not release HMGB1 and are “immunologically silent”, in contrast to necrotic cells [271,272]. Upon the administration of DOX, metastatic human melanoma SK-MEL-24 and human colon cancer LS174T cells undergo senescence; however, the less-metastatic cell lines SK-MEL-28 and DLD-1 prefer apoptosis following drug treatment. The expression of HMGB1 was found to be persistent in senescent B16-F10, SK-MEL-24, and LS174T cells that had been treated with DOX. This led to a rise in P21 levels. Furthermore, HMGB1 depletion caused a shift from senescence to apoptosis in B16-F10 cells, and HMGB1 overexpression managed to trigger the transition from apoptosis to senescence simultaneously with increased P21 expression in B16 cells after treatment with DOX. According to these findings, selective induction of tumor suppression might be possible through the use of HMGB1 regulation of malignancies that have distinct metastatic capability [273]. HMGB1, which is released by cancer cells, serves as a ligand for the TLR-4 receptor on DCs. Sera IFNγ levels are highest after treatment with DCs and DOX, which contributes to the induction of immunological cell death [270,273].
Yang et al. generated DOX prodrug nanoparticles (CAP-NPs) via conjugation of the cathepsin B-cleavable peptide with DOX that allowed the release of the DOX only in cancer cells over-expressing cathepsin B. Moreover, when compared with the treatment of conventional free DOX with anti-PD-L1 antibodies, the combinatorial therapy of CAP-NPs with the same immune-checkpoint inhibitor demonstrated a significantly higher rate of complete tumor regression (50%) than the latter. During this time, CAP-NP-treated mice experienced significantly fewer adverse effects that were associated with DOX treatment and PD-1/PD-L1 blockage [34,274]. It has been also demonstrated that PD-L1-directed liposomes encompassing DOX are a reasonable combination that is capable of improving the activity of the immune system by blocking PD-L1 and through discriminate internalization of DOX in cancer cells. This combination has been effective in providing a dual benefit that is achieved by both the chemo- and immune-therapeutic strategies [275].
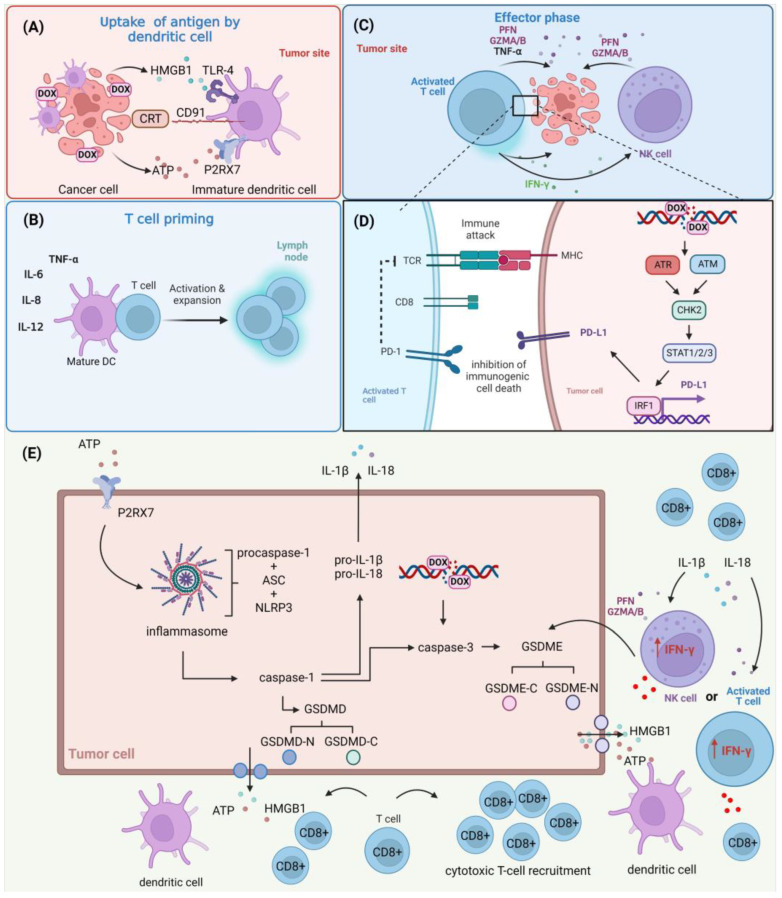
Unlike apoptotic cells, which remain immunologically quiet, pyroptotic cells rapidly leak their cellular contents, such as cell antigens, proinflammatory cytokines, and damage-associated molecular patterns (DAMPs), which can then affect the tumor immune microenvironment, activate host antitumor immunity, and ultimately result in tumor regression. Furthermore, APCs adopt a “hyperactive” state characterized by increased motility and promotion of higher cytotoxic T-lymphocyte responses after being activated by pyroptosis-induced signals [276]. The influence of DOX on the anti-tumor immune response is shown in Figure 3.
Figure 3.
The role of DOX in the anti-tumor immune response. (A) DOX induces the apoptotic cell death of cancer cells, contributing to the exposition or release of ATP, calreticulin (CRT), and high mobility group box protein B1 (HMGB1) of cancer cells and promoting their recognition by dendritic cells (DCs) through respective receptors (P2X purinoceptor 7 (P2RX7), CD91, and toll-like receptor 4 (TLR-4)) present on their cellular surface. (B) These events allow the maturation of DCs and the release of immune-stimulating factors such as interleukins (ILs) and tumor-necrosis factor α (TNF-α). These events promote the activation and expansion of T cells. (C) Activated T cells and natural killer (NK) cells recruited to the tumor microenvironment release perforins (PFNs), granzyme A/B (GZMA/B), and interferon γ (IFN-γ), leading to cancer-cell death. (D) DOX induces double-strand break (DSB) formation, contributing to the activation of the ATR/ATM/CHK2 pathway and promoting STAT1/2/3/IRF1-mediated programmed cell death 1 ligand 1 (PD-L1) up-regulation. This confers to the inhibition of immunogenic cell death. (E) ATP released by dying cancer cells activates P2RX7 expressed on surrounding tumor cells, contributing to the formation of the inflammasome (consisting of adapter protein apoptosis-associated speck-like protein containing a CARD (ASC), NACHT, LRR, and PYD domains-containing protein 3 (NLRP3) and procaspase-1) and activation of caspase-1, which converts pro-IL-1β and pro-IL-18 to active forms (IL-1β, IL-18), activates effector caspase-3, and cleaves gasdermin-D/E (GSDMD/E) to the C-terminal moiety (GSDMD/E-C) and promotes the release of the N-terminal moiety (GSDMD/E-N) that forms pores, triggering pyroptosis. This contributes to the release of a multitude of intracellular factors including ATP, HMGB1, IL-1β, and IL-8 to the extracellular space. Alternatively, the cleavage of GSDMD/E can be triggered by GZNMA/B and PFNs released by NK cells and activated T cells recruited to the tumor microenvironment. Created with BioRender.com accessed on 1 January 2023.
4. Conclusions
Because of its efficacy in battling a wide spectrum of malignancies, DOX is commonly employed in chemotherapeutic regimens. Despite its widespread clinical use, the mechanisms of action of DOX are still being debated. Although the precise mechanisms of action of DOX remain unknown, it is established that this anticancer agent intercalates into DNA, inhibits topoisomerase enzymes, disrupts the proper functioning of mitochondria, and increases free-radical production and oxidative damage [4]. Besides triggering the mitochondrial apoptosis pathway, DOX also induces senescence, autophagy, pyroptosis, ferroptosis, or necrosis of cancer cells depending on the dose of the drug and the cellular context.
DOX not only has direct cytotoxic effects on cancer cells, but also contributes to the elimination of cancer cells via the activation of immune CD8+ T-cell responses. An understanding of the interplay between the DOX-treated cells and the tumor microenvironment seems crucial for the development of combinatorial regimens including immune checkpoint inhibitors such as PD-L1 antibodies and DOX [231].
DOX exerts its effect on normal cells, leading to the development of life-threatening side effects including myelosuppression, nephrotoxicity, and cardiotoxicity [153,189]. Attempts should be made to find more effective ways to manage DOX toxicity. As a result, DOX must be loaded into a special vehicle and delivered to specific tumor sites, minimizing toxicity while maximizing the therapeutic benefits. Therefore, numerous investigations have been conducted on DOX nanoformulations such as liposomes, polymer micelles, dendrimers, and nanogels [277]. Although several DOX nanoformulations have been shown to increase the therapeutic output in comparison to standard preparations, they still face obstacles such as suboptimal diffusion and permeation properties, sophisticated release patterns, immunogenic responses, and undesirable interactions with serum proteins that force their in-depth in vitro and in vivo investigations [4,278].
Abbreviations
| AIF | apoptosis-inducing factor |
| APAF1 | apoptotic protease-activating factor 1 |
| APC | antigen-presenting cell |
| ASC | adapter protein apoptosis-associated speck-like protein containing a CARD |
| ASCO | apoptosis-associated speck-like protein containing a caspase recruitment domain |
| ATM | ataxia telangiectasia mutated (A-T mutated) |
| ATR | ataxia telangiectasia and Rad3-related |
| ATRIP | ATR-interacting protein |
| BCL-2 | apoptosis regulator BCL2 |
| BCL-xL | B-cell lymphoma-extra large |
| CDC25A/C | M-phase inducer phosphatases |
| CDK | cyclin-dependent kinase |
| CHK1/2 | checkpoint kinases |
| CL | Cardiolipin |
| CRT | Calreticulin |
| CXCL | C-X-C motif chemokine receptors |
| DAMPs | damage-associated molecular patterns |
| DDR | DNA damage response |
| DFNA5 | deafness, autosomal dominant 5, isoform CRA |
| DIABLO | direct inhibitor of apoptosis-binding protein with low |
| DNA-PKcs | DNA-dependent protein kinase catalytic subunit |
| DOX | Doxorubicin |
| DPC | DNA–protein crosslink |
| DR5 | death receptor 5 |
| DSBs | double-strand breaks |
| eEF-2K | eukaryotic elongation factor-2 kinase |
| EMT | epithelial–mesenchymal transition |
| ER | Endoplasmic reticulum |
| ETAA1 | Ewing’s tumor-associated antigen 1 |
| ETC | electron transport chain |
| FASL | FAS antigen ligand |
| FDA | Food and Drug Administration |
| FLIP | FLICE/caspase-8 inhibitory protein |
| GATA4 | GATA Binding Protein 4 |
| GPX4 | glutathione peroxidase |
| GSDMD/E | gasdermin-D/E |
| GZMA/B | granzyme A/B |
| HMGB1 | high mobility group box protein B1 |
| HR | homologous recombination |
| IFNs | Interferons |
| ILs | Interleukins |
| IREs | iron-response elements |
| IRF1 | interferon regulatory factor 1 |
| IRP1/2 | iron regulatory proteins 1/2 |
| JAK | tyrosine-protein kinase JAK |
| JNK | C-Jun N-terminal kinase |
| MAVS | adaptor protein mitochondrial antiviral signaling |
| MCM2/7 | minichromosome maintenance helicase complex |
| MDA-5 | melanoma differentiation Ag-5 |
| MDC-1 | mediator of DNA damage checkpoint protein 1 |
| MDR1 | multidrug resistance 1 |
| MHC | major histocompatibility complex |
| MRE11 | meiotic recombination 11 homolog 1 |
| MRN | MRE11–RAD50–NBS1 complex |
| mtDNA | mitochondrial DNA |
| NBS1 | Nibrin |
| nDNA | nuclear DNA |
| NFAT | nuclear factor of activated T-lymphocytes |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NHEJ | non-homologous end joining |
| NK | natural killer cell |
| NLRP3 | NACHT, LRR, and PYD domains-containing protein 3 |
| NOXA | phorbol-12-myristate-13-acetate-induced protein 1 |
| NRF2 | nuclear factor erythroid 2-related factor 2 |
| P2RX7 | P2X purinoceptor |
| PARP-1 | poly(ADP-ribose) polymerase 1 |
| PARs | poly(ADP-ribose) polymers |
| PD-L1 | programmed death ligand 1 |
| PEG | polyethylene glycol |
| PFNs | Perforins |
| PG-P | P-glycoprotein |
| PIKKs | phosphoinositide 3-kinase-related protein kinases |
| PNKP | polynucleotide kinase phosphatase |
| pRB | retinoblastoma protein |
| PRDX2 | peroxiredoxin-2 |
| PUMA | isoform 1 of Bcl-2-binding component 3, isoforms 1/2 |
| RHINO | RAD9, RAD1, HUS1 interacting nuclear orphan |
| RIG-1 | retinoic acid inducible gene-I |
| RNS | reactive nitrogen species |
| ROS | reactive oxygen species |
| RPA | replication protein A |
| SASP | senescence-associated secretory phenotype |
| SOD2 | superoxide dismutase 2 |
| SMAC | secondary mitochondria-derived activator of caspases |
| SSBR | single-strand break repair |
| SSBs | single-strand breaks |
| ssDNA | single-stranded DNA |
| STAT1/2/3 | signal transducer and activator of transcription 1/2/3 |
| TAMs | tumor-associated macrophages |
| TPD-1 | tyrosyl-DNA phosphodiesterase 1 |
| TIS | therapy-induced senescence |
| TLR4 | Toll-like receptor 4 |
| TNFR1 | tumor necrosis factor receptor 1 |
| TNF-α | tumor necrosis factor α |
| TOPB1 | topoisomerase 2-binding protein 1 |
| TP53 | cellular tumor antigen p53 |
| TRAIL | TNF-related apoptosis inducing ligand |
| TRX1 | thioredoxin-1 |
| XRCC1 | X-ray repair cross-complementing group-1 |
Author Contributions
Conceptualization, M.K., A.G., D.K., Ż.K.-K., S.M. and I.C.; Supervision, M.K., S.M. and R.K.; Visualization, M.K., D.K. and Ż.K.-K.; Writing—original draft, M.K., A.G. and I.C.; Writing—review and editing, M.K., A.G., D.K., S.M. and R.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Mohseni M., Samadi N., Ghanbari P., Yousefi B., Tabasinezhad M., Sharifi S., Nazemiyeh H. Co-Treatment by Docetaxel and Vinblastine Breaks down P-Glycoprotein Mediated Chemo-Resistance. Iran. J. Basic Med. Sci. 2016;19:300–309. [PMC free article] [PubMed] [Google Scholar]
- 2.Dallavalle S., Dobričić V., Lazzarato L., Gazzano E., Machuqueiro M., Pajeva I., Tsakovska I., Zidar N., Fruttero R. Improvement of Conventional Anti-Cancer Drugs as New Tools against Multidrug Resistant Tumors. Drug Resist. Updat. 2020;50:100682. doi: 10.1016/j.drup.2020.100682. [DOI] [PubMed] [Google Scholar]
- 3.Bukowski K., Kciuk M., Kontek R. Mechanisms of Multidrug Resistance in Cancer Chemotherapy. Int. J. Mol. Sci. 2020;21:3233. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carvalho C., Santos R.X., Cardoso S., Correia S., Oliveira P.J., Santos M.S., Moreira P.I. Doxorubicin: The Good, the Bad and the Ugly Effect. Curr. Med. Chem. 2009;16:3267–3285. doi: 10.2174/092986709788803312. [DOI] [PubMed] [Google Scholar]
- 5.Rawat P.S., Jaiswal A., Khurana A., Bhatti J.S., Navik U. Doxorubicin-Induced Cardiotoxicity: An Update on the Molecular Mechanism and Novel Therapeutic Strategies for Effective Management. Biomed. Pharmacother. 2021;139:111708. doi: 10.1016/j.biopha.2021.111708. [DOI] [PubMed] [Google Scholar]
- 6.Thorn C.F., Oshiro C., Marsh S., Hernandez-Boussard T., McLeod H., Klein T.E., Altman R.B. Doxorubicin Pathways: Pharmacodynamics and Adverse Effects. Pharm. Genom. 2011;21:440–446. doi: 10.1097/FPC.0b013e32833ffb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi Y., Moon M., Dawood S., McManus B., Liu P.P. Mechanisms and Management of Doxorubicin Cardiotoxicity. Herz. 2011;36:296–305. doi: 10.1007/s00059-011-3470-3. [DOI] [PubMed] [Google Scholar]
- 8.Wenningmann N., Knapp M., Ande A., Vaidya T.R., Ait-Oudhia S. Insights into Doxorubicin-Induced Cardiotoxicity: Molecular Mechanisms, Preventive Strategies, and Early Monitoring. Mol. Pharmacol. 2019;96:219–232. doi: 10.1124/mol.119.115725. [DOI] [PubMed] [Google Scholar]
- 9.Sheibani M., Azizi Y., Shayan M., Nezamoleslami S., Eslami F., Farjoo M.H., Dehpour A.R. Doxorubicin-Induced Cardiotoxicity: An Overview on Pre-Clinical Therapeutic Approaches. Cardiovasc. Toxicol. 2022;22:292–310. doi: 10.1007/s12012-022-09721-1. [DOI] [PubMed] [Google Scholar]
- 10.Kalyanaraman B. Teaching the Basics of the Mechanism of Doxorubicin-Induced Cardiotoxicity: Have We Been Barking up the Wrong Tree? Redox Biol. 2020;29:101394. doi: 10.1016/j.redox.2019.101394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pugazhendhi A., Edison T.N.J.I., Velmurugan B.K., Jacob J.A., Karuppusamy I. Toxicity of Doxorubicin (Dox) to Different Experimental Organ Systems. Life Sci. 2018;200:26–30. doi: 10.1016/j.lfs.2018.03.023. [DOI] [PubMed] [Google Scholar]
- 12.Tacar O., Sriamornsak P., Dass C.R. Doxorubicin: An Update on Anticancer Molecular Action, Toxicity and Novel Drug Delivery Systems. J. Pharm. Pharmacol. 2013;65:157–170. doi: 10.1111/j.2042-7158.2012.01567.x. [DOI] [PubMed] [Google Scholar]
- 13.Mohan U.P., Pichiah P.B.T., Iqbal S.T.A., Arunachalam S. Mechanisms of Doxorubicin-Mediated Reproductive Toxicity—A Review. Reprod. Toxicol. 2021;102:80–89. doi: 10.1016/j.reprotox.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 14.Alhowail A.H., Bloemer J., Majrashi M., Pinky P.D., Bhattacharya S., Yongli Z., Bhattacharya D., Eggert M., Woodie L., Buabeid M.A., et al. Doxorubicin-Induced Neurotoxicity Is Associated with Acute Alterations in Synaptic Plasticity, Apoptosis, and Lipid Peroxidation. Toxicol. Mech. Methods. 2019;29:457–466. doi: 10.1080/15376516.2019.1600086. [DOI] [PubMed] [Google Scholar]
- 15.Tangpong J., Miriyala S., Noel T., Sinthupibulyakit C., Jungsuwadee P., St Clair D.K. Doxorubicin-Induced Central Nervous System Toxicity and Protection by Xanthone Derivative of Garcinia Mangostana. Neuroscience. 2011;175:292–299. doi: 10.1016/j.neuroscience.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prasanna P.L., Renu K., Valsala Gopalakrishnan A. New Molecular and Biochemical Insights of Doxorubicin-Induced Hepatotoxicity. Life Sci. 2020;250:117599. doi: 10.1016/j.lfs.2020.117599. [DOI] [PubMed] [Google Scholar]
- 17.Ayla S., Seckin I., Tanriverdi G., Cengiz M., Eser M., Soner B.C., Oktem G. Doxorubicin Induced Nephrotoxicity: Protective Effect of Nicotinamide. Int. J. Cell Biol. 2011;2011:390238. doi: 10.1155/2011/390238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Manil L., Couvreur P., Mahieu P. Acute Renal Toxicity of Doxorubicin (Adriamycin)-Loaded Cyanoacrylate Nanoparticles. Pharm. Res. 1995;12:85–87. doi: 10.1023/A:1016290704772. [DOI] [PubMed] [Google Scholar]
- 19.Lahoti T.S., Patel D., Thekkemadom V., Beckett R., Ray S.D. Doxorubicin-Induced in Vivo Nephrotoxicity Involves Oxidative Stress-Mediated Multiple pro- and Anti-Apoptotic Signaling Pathways. Curr. Neurovasc. Res. 2012;9:282–295. doi: 10.2174/156720212803530636. [DOI] [PubMed] [Google Scholar]
- 20.van der Zanden S.Y., Qiao X., Neefjes J. New Insights into the Activities and Toxicities of the Old Anticancer Drug Doxorubicin. FEBS J. 2021;288:6095–6111. doi: 10.1111/febs.15583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varela-López A., Battino M., Navarro-Hortal M.D., Giampieri F., Forbes-Hernández T.Y., Romero-Márquez J.M., Collado R., Quiles J.L. An Update on the Mechanisms Related to Cell Death and Toxicity of Doxorubicin and the Protective Role of Nutrients. Food Chem. Toxicol. 2019;134:110834. doi: 10.1016/j.fct.2019.110834. [DOI] [PubMed] [Google Scholar]
- 22.Moustafa I., Viljoen M., Perumal-Pillay V.A., Oosthuizen F. Critical Appraisal of Clinical Guidelines for Prevention and Management of Doxorubicin-Induced Cardiotoxicity. J. Oncol. Pharm. Pract. 2022:147660. doi: 10.1177/10781552221147660. [DOI] [PubMed] [Google Scholar]
- 23.Benzer F., Kandemir F.M., Kucukler S., Comaklı S., Caglayan C. Chemoprotective Effects of Curcumin on Doxorubicin-Induced Nephrotoxicity in Wistar Rats: By Modulating Inflammatory Cytokines, Apoptosis, Oxidative Stress and Oxidative DNA Damage. Arch. Physiol. Biochem. 2018;124:448–457. doi: 10.1080/13813455.2017.1422766. [DOI] [PubMed] [Google Scholar]
- 24.Rashid S., Ali N., Nafees S., Ahmad S.T., Arjumand W., Hasan S.K., Sultana S. Alleviation of Doxorubicin-Induced Nephrotoxicity and Hepatotoxicity by Chrysin in Wistar Rats. Toxicol. Mech. Methods. 2013;23:337–345. doi: 10.3109/15376516.2012.759306. [DOI] [PubMed] [Google Scholar]
- 25.Ibrahim Fouad G., Ahmed K.A. Neuroprotective Potential of Berberine Against Doxorubicin-Induced Toxicity in Rat’s Brain. Neurochem. Res. 2021;46:3247–3263. doi: 10.1007/s11064-021-03428-5. [DOI] [PubMed] [Google Scholar]
- 26.Shafei A., El-Bakly W., Sobhy A., Wagdy O., Reda A., Aboelenin O., Marzouk A., El Habak K., Mostafa R., Ali M.A., et al. A Review on the Efficacy and Toxicity of Different Doxorubicin Nanoparticles for _targeted Therapy in Metastatic Breast Cancer. Biomed. Pharmacother. 2017;95:1209–1218. doi: 10.1016/j.biopha.2017.09.059. [DOI] [PubMed] [Google Scholar]
- 27.Prados J., Melguizo C., Ortiz R., Vélez C., Alvarez P.J., Arias J.L., Ruíz M.A., Gallardo V., Aranega A. Doxorubicin-Loaded Nanoparticles: New Advances in Breast Cancer Therapy. Anticancer Agents Med. Chem. 2012;12:1058–1070. doi: 10.2174/187152012803529646. [DOI] [PubMed] [Google Scholar]
- 28.Zhao N., Woodle M.C., Mixson A.J. Advances in Delivery Systems for Doxorubicin. J. Nanomed. Nanotechnol. 2018;9:519. doi: 10.4172/2157-7439.1000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kanwal U., Irfan Bukhari N., Ovais M., Abass N., Hussain K., Raza A. Advances in Nano-Delivery Systems for Doxorubicin: An Updated Insight. J. Drug _target. 2018;26:296–310. doi: 10.1080/1061186X.2017.1380655. [DOI] [PubMed] [Google Scholar]
- 30.Ansari L., Shiehzadeh F., Taherzadeh Z., Nikoofal-Sahlabadi S., Momtazi-Borojeni A.A., Sahebkar A., Eslami S. The Most Prevalent Side Effects of Pegylated Liposomal Doxorubicin Monotherapy in Women with Metastatic Breast Cancer: A Systematic Review of Clinical Trials. Cancer Gene Ther. 2017;24:189–193. doi: 10.1038/cgt.2017.9. [DOI] [PubMed] [Google Scholar]
- 31.Miguel R.D.A., Hirata A.S., Jimenez P.C., Lopes L.B., Costa-Lotufo L.V. Beyond Formulation: Contributions of Nanotechnology for Translation of Anticancer Natural Products into New Drugs. Pharmaceutics. 2022;14:1722. doi: 10.3390/pharmaceutics14081722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mukhtar M., Bilal M., Rahdar A., Barani M., Arshad R., Behl T., Brisc C., Banica F., Bungau S. Nanomaterials for Diagnosis and Treatment of Brain Cancer: Recent Updates. Chemosensors. 2020;8:117. doi: 10.3390/chemosensors8040117. [DOI] [Google Scholar]
- 33.Skarbek C., Serra S., Maslah H., Rascol E., Labruère R. Arylboronate Prodrugs of Doxorubicin as Promising Chemotherapy for Pancreatic Cancer. Bioorg. Chem. 2019;91:103158. doi: 10.1016/j.bioorg.2019.103158. [DOI] [PubMed] [Google Scholar]
- 34.Zhong Y.-J., Shao L.-H., Li Y. Cathepsin B-Cleavable Doxorubicin Prodrugs for _targeted Cancer Therapy (Review) Int. J. Oncol. 2013;42:373–383. doi: 10.3892/ijo.2012.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garsky V.M., Lumma P.K., Feng D.M., Wai J., Ramjit H.G., Sardana M.K., Oliff A., Jones R.E., DeFeo-Jones D., Freidinger R.M. The Synthesis of a Prodrug of Doxorubicin Designed to Provide Reduced Systemic Toxicity and Greater _target Efficacy. J. Med. Chem. 2001;44:4216–4224. doi: 10.1021/jm0101996. [DOI] [PubMed] [Google Scholar]
- 36.DeFeo-Jones D., Garsky V.M., Wong B.K., Feng D.M., Bolyar T., Haskell K., Kiefer D.M., Leander K., McAvoy E., Lumma P., et al. A Peptide-Doxorubicin “prodrug” Activated by Prostate-Specific Antigen Selectively Kills Prostate Tumor Cells Positive for Prostate-Specific Antigen in Vivo. Nat. Med. 2000;6:1248–1252. doi: 10.1038/81351. [DOI] [PubMed] [Google Scholar]
- 37.Albright C.F., Graciani N., Han W., Yue E., Stein R., Lai Z., Diamond M., Dowling R., Grimminger L., Zhang S.-Y., et al. Matrix Metalloproteinase-Activated Doxorubicin Prodrugs Inhibit HT1080 Xenograft Growth Better than Doxorubicin with Less Toxicity. Mol. Cancer Ther. 2005;4:751–760. doi: 10.1158/1535-7163.MCT-05-0006. [DOI] [PubMed] [Google Scholar]
- 38.Bao Y., Yin M., Hu X., Zhuang X., Sun Y., Guo Y., Tan S., Zhang Z. A Safe, Simple and Efficient Doxorubicin Prodrug Hybrid Micelle for Overcoming Tumor Multidrug Resistance and _targeting Delivery. J. Control. Release. 2016;235:182–194. doi: 10.1016/j.jconrel.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 39.Farquhar D., Newman R.A., Zuckerman J.E., Andersson B.S. Doxorubicin Analogues Incorporating Chemically Reactive Substituents. J. Med. Chem. 1991;34:561–564. doi: 10.1021/jm00106a013. [DOI] [PubMed] [Google Scholar]
- 40.Weiss R.B. The Anthracyclines: Will We Ever Find a Better Doxorubicin? Semin. Oncol. 1992;19:670–686. [PubMed] [Google Scholar]
- 41.Brown J.R., Imam S.H. Recent Studies on Doxorubicin and Its Analogues. Prog. Med. Chem. 1984;21:169–236. doi: 10.1016/s0079-6468(08)70410-7. [DOI] [PubMed] [Google Scholar]
- 42.Giuliani F.C., Kaplan N.O. New Doxorubicin Analogs Active against Doxorubicin-Resistant Colon Tumor Xenografts in the Nude Mouse. Cancer Res. 1980;40:4682–4687. [PubMed] [Google Scholar]
- 43.Lang D.K., Kaur R., Arora R., Saini B., Arora S. Nitrogen-Containing Heterocycles as Anticancer Agents: An Overview. Anticancer Agents Med. Chem. 2020;20:2150–2168. doi: 10.2174/1871520620666200705214917. [DOI] [PubMed] [Google Scholar]
- 44.Sohail M., Sun Z., Li Y., Gu X., Xu H. Research Progress in Strategies to Improve the Efficacy and Safety of Doxorubicin for Cancer Chemotherapy. Expert Rev. Anticancer Ther. 2021;21:1385–1398. doi: 10.1080/14737140.2021.1991316. [DOI] [PubMed] [Google Scholar]
- 45.Zujewski J.A., Eng-Wong J., O’Shaughnessy J., Venzon D., Chow C., Danforth D., Kohler D.R., Cusack G., Riseberg D., Cowan K.H. A Pilot Study of Dose Intense Doxorubicin and Cyclophosphamide Followed by Infusional Paclitaxel in High-Risk Primary Breast Cancer. Breast Cancer Res. Treat. 2003;81:41–51. doi: 10.1023/A:1025421416674. [DOI] [PubMed] [Google Scholar]
- 46.Liu X., Jiang S., Wang H., Wu X., Yan W., Chen Y., Xu Y., Wang C., Yao W., Wang J., et al. Pegylated Liposomal Doxorubicin Combined with Ifosfamide for Treating Advanced or Metastatic Soft-Tissue Sarcoma: A Prospective, Single-Arm Phase II Study. Clin. Cancer Res. 2022;28:5280–5289. doi: 10.1158/1078-0432.CCR-22-1785. [DOI] [PubMed] [Google Scholar]
- 47.Pautier P., Italiano A., Piperno-Neumann S., Chevreau C., Penel N., Firmin N., Boudou-Rouquette P., Bertucci F., Balleyguier C., Lebrun-Ly V., et al. Doxorubicin Alone versus Doxorubicin with Trabectedin Followed by Trabectedin Alone as First-Line Therapy for Metastatic or Unresectable Leiomyosarcoma (LMS-04): A Randomised, Multicentre, Open-Label Phase 3 Trial. Lancet Oncol. 2022;23:1044–1054. doi: 10.1016/S1470-2045(22)00380-1. [DOI] [PubMed] [Google Scholar]
- 48.Picardi M., Giordano C., Pugliese N., Esposito M., Fatigati M., Muriano F., Rascato M.G., Pepa R.D., D’Ambrosio A., Vigliar E., et al. Liposomal Doxorubicin Supercharge-Containing Front-Line Treatment in Patients with Advanced-Stage Diffuse Large B-Cell Lymphoma or Classical Hodgkin Lymphoma: Preliminary Results of a Single-Centre Phase II Study. Br. J. Haematol. 2022;198:847–860. doi: 10.1111/bjh.18348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Prakash S.S., Nagarkar R.V., Puligundla K.C., Lokesh K.N., Boya R.R., Patel A.B., Goyal L., Thoke A., Patel J.G., Mehta A.O., et al. Bioequivalence of a Hybrid Pegylated Liposomal Doxorubicin Hydrochloride Injection and Caelyx®: A Single-Dose, Randomized, Multicenter, Open-Label, Two-Period Crossover Study in Patients with Advanced Ovarian Cancer. Eur. J. Pharm. Sci. 2022;176:106248. doi: 10.1016/j.ejps.2022.106248. [DOI] [PubMed] [Google Scholar]
- 50.Wang T., Tang J., Yang H., Yin R., Zhang J., Zhou Q., Liu Z., Cao L., Li L., Huang Y., et al. Effect of Apatinib Plus Pegylated Liposomal Doxorubicin vs Pegylated Liposomal Doxorubicin Alone on Platinum-Resistant Recurrent Ovarian Cancer: The APPROVE Randomized Clinical Trial. JAMA Oncol. 2022;8:1169–1176. doi: 10.1001/jamaoncol.2022.2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee Y.J., Seol A., Lee M., Kim J.-W., Kim H.S., Kim K., Suh D.H., Kim S., Kim S.W., Lee J.-Y. A Phase II Trial to Evaluate the Efficacy of Bortezomib and Liposomal Doxorubicin in Patients With BRCA Wild-Type Platinum-Resistant Recurrent Ovarian Cancer (KGOG 3044/EBLIN) In Vivo. 2022;36:1949–1958. doi: 10.21873/invivo.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elfadadny A., Ragab R.F., Hamada R., Al Jaouni S.K., Fu J., Mousa S.A., El-Far A.H. Natural Bioactive Compounds-Doxorubicin Combinations _targeting Topoisomerase II-Alpha: Anticancer Efficacy and Safety. Toxicol. Appl. Pharmacol. 2023;461:116405. doi: 10.1016/j.taap.2023.116405. [DOI] [PubMed] [Google Scholar]
- 53.Qiu C., Wu Y., Shi Q., Guo Q., Zhang J., Meng Y., Wang C., Xia F., Wang J., Xu C. Advanced Strategies for Nucleic Acids and Small-Molecular Drugs in Combined Anticancer Therapy. Int. J. Biol. Sci. 2023;19:789–810. doi: 10.7150/ijbs.79328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.de Padua T.C., Marandino L., Raggi D., Hallanger-Johnson J., Kutikov A., Spiess P.E., Necchi A. A Systematic Review of Published Clinical Trials in the Systemic Treatment of Adrenocortical Carcinoma: An Initiative Led on Behalf of the Global Society of Rare Genitourinary Tumors. Clin. Genitourin. Cancer. 2023;21:1–7. doi: 10.1016/j.clgc.2022.10.011. [DOI] [PubMed] [Google Scholar]
- 55.Chen Y., Xu H., Shan N., Qu H. Pegylated Liposomal Doxorubicin (PLD)-Containing Regimen as a Novel Treatment of Monomorphic Epithelial Intestinal T-Cell Lymphoma (MEITL): A Case Report and Review of Literature. Medicine. 2022;101:e31326. doi: 10.1097/MD.0000000000031326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Younes M., Mardirossian R., Rizk L., Fazlian T., Khairallah J.P., Sleiman C., Naim H.Y., Rizk S. The Synergistic Effects of Curcumin and Chemotherapeutic Drugs in Inhibiting Metastatic, Invasive and Proliferative Pathways. Plants. 2022;11:2137. doi: 10.3390/plants11162137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kciuk M., Kołat D., Kałuzińska-Kołat Ż., Gawrysiak M., Drozda R., Celik I., Kontek R. PD-1/PD-L1 and DNA Damage Response in Cancer. Cells. 2023;12:530. doi: 10.3390/cells12040530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Howerton S.B., Nagpal A., Williams L.D. Surprising Roles of Electrostatic Interactions in DNA-Ligand Complexes. Biopolymers. 2003;69:87–99. doi: 10.1002/bip.10319. [DOI] [PubMed] [Google Scholar]
- 59.Lipscomb L.A., Peek M.E., Zhou F.X., Bertrand J.A., VanDerveer D., Williams L.D. Water Ring Structure at DNA Interfaces: Hydration and Dynamics of DNA-Anthracycline Complexes. Biochemistry. 1994;33:3649–3659. doi: 10.1021/bi00178a023. [DOI] [PubMed] [Google Scholar]
- 60.Zlatanova J., Victor J.-M. How Are Nucleosomes Disrupted during Transcription Elongation? HFSP J. 2009;3:373–378. doi: 10.2976/1.3249971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yang F., Kemp C.J., Henikoff S. Doxorubicin Enhances Nucleosome Turnover around Promoters. Curr. Biol. 2013;23:782–787. doi: 10.1016/j.cub.2013.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Salerno D., Brogioli D., Cassina V., Turchi D., Beretta G.L., Seruggia D., Ziano R., Zunino F., Mantegazza F. Magnetic Tweezers Measurements of the Nanomechanical Properties of DNA in the Presence of Drugs. Nucleic Acids Res. 2010;38:7089–7099. doi: 10.1093/nar/gkq597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yang F., Teves S.S., Kemp C.J., Henikoff S. Doxorubicin, DNA Torsion, and Chromatin Dynamics. Biochim. Biophys. Acta. 2014;1845:84–89. doi: 10.1016/j.bbcan.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Swift L.P., Rephaeli A., Nudelman A., Phillips D.R., Cutts S.M. Doxorubicin-DNA Adducts Induce a Non-Topoisomerase II-Mediated Form of Cell Death. Cancer Res. 2006;66:4863–4871. doi: 10.1158/0008-5472.CAN-05-3410. [DOI] [PubMed] [Google Scholar]
- 65.Forrest R.A., Swift L.P., Rephaeli A., Nudelman A., Kimura K.-I., Phillips D.R., Cutts S.M. Activation of DNA Damage Response Pathways as a Consequence of Anthracycline-DNA Adduct Formation. Biochem. Pharmacol. 2012;83:1602–1612. doi: 10.1016/j.bcp.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 66.Coldwell K.E., Cutts S.M., Ognibene T.J., Henderson P.T., Phillips D.R. Detection of Adriamycin-DNA Adducts by Accelerator Mass Spectrometry at Clinically Relevant Adriamycin Concentrations. Nucleic Acids Res. 2008;36:e100. doi: 10.1093/nar/gkn439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kciuk M., Marciniak B., Kontek R. Irinotecan—Still an Important Player in Cancer Chemotherapy: A Comprehensive Overview. Int. J. Mol. Sci. 2020;21:4919. doi: 10.3390/ijms21144919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pommier Y., Leo E., Zhang H., Marchand C. DNA Topoisomerases and Their Poisoning by Anticancer and Antibacterial Drugs. Chem. Biol. 2010;17:421–433. doi: 10.1016/j.chembiol.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ross W.E., Glaubiger D.L., Kohn K.W. Protein-Associated DNA Breaks in Cells Treated with Adriamycin or Ellipticine. Biochim. Biophys. Acta. 1978;519:23–30. doi: 10.1016/0005-2787(78)90059-X. [DOI] [PubMed] [Google Scholar]
- 70.Tewey K.M., Rowe T.C., Yang L., Halligan B.D., Liu L.F. Adriamycin-Induced DNA Damage Mediated by Mammalian DNA Topoisomerase II. Science. 1984;226:466–468. doi: 10.1126/science.6093249. [DOI] [PubMed] [Google Scholar]
- 71.Fokas E., Prevo R., Hammond E.M., Brunner T.B., McKenna W.G., Muschel R.J. _targeting ATR in DNA Damage Response and Cancer Therapeutics. Cancer Treat. Rev. 2014;40:109–117. doi: 10.1016/j.ctrv.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 72.Lecona E., Fernandez-Capetillo O. _targeting ATR in Cancer. Nat. Rev. Cancer. 2018;18:586–595. doi: 10.1038/s41568-018-0034-3. [DOI] [PubMed] [Google Scholar]
- 73.Maréchal A., Zou L. DNA Damage Sensing by the ATM and ATR Kinases. Cold Spring Harb. Perspect. Biol. 2013;5:a012716. doi: 10.1101/cshperspect.a012716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saldivar J.C., Cortez D., Cimprich K.A. The Essential Kinase ATR: Ensuring Faithful Duplication of a Challenging Genome. Nat. Rev. Mol. Cell Biol. 2017;18:622–636. doi: 10.1038/nrm.2017.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ma A., Dai X. The Relationship between DNA Single-Stranded Damage Response and Double-Stranded Damage Response. Cell Cycle. 2018;17:73–79. doi: 10.1080/15384101.2017.1403681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kciuk M., Gielecińska A., Kołat D., Kałuzińska Ż., Kontek R. Cancer-Associated Transcription Factors in DNA Damage Response. Biochim. Biophys. Acta Rev. Cancer. 2022;1877:188757. doi: 10.1016/j.bbcan.2022.188757. [DOI] [PubMed] [Google Scholar]
- 77.Kciuk M., Gielecińska A., Mujwar S., Mojzych M., Kontek R. Cyclin-Dependent Kinases in DNA Damage Response. Biochim. Biophys. Acta Rev. Cancer. 2022;1877:188716. doi: 10.1016/j.bbcan.2022.188716. [DOI] [PubMed] [Google Scholar]
- 78.Kciuk M., Marciniak B., Mojzych M., Kontek R. Focus on UV-Induced DNA Damage and Repair—Disease Relevance and Protective Strategies. Int. J. Mol. Sci. 2020;21:7264. doi: 10.3390/ijms21197264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cimprich K.A., Cortez D. ATR: An Essential Regulator of Genome Integrity. Nat. Rev. Mol. Cell Biol. 2008;9:616–627. doi: 10.1038/nrm2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mei C., Lei L., Tan L.-M., Xu X.-J., He B.-M., Luo C., Yin J.-Y., Li X., Zhang W., Zhou H.-H., et al. The Role of Single Strand Break Repair Pathways in Cellular Responses to Camptothecin Induced DNA Damage. Biomed. Pharmacother. 2020;125:109875. doi: 10.1016/j.biopha.2020.109875. [DOI] [PubMed] [Google Scholar]
- 81.Abbotts R., Wilson D.M. Coordination of DNA Single Strand Break Repair. Free Radic. Biol. Med. 2017;107:228–244. doi: 10.1016/j.freeradbiomed.2016.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fortini P., Dogliotti E. Base Damage and Single-Strand Break Repair: Mechanisms and Functional Significance of Short- and Long-Patch Repair Subpathways. DNA Repair. 2007;6:398–409. doi: 10.1016/j.dnarep.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 83.Caldecott K.W. Mammalian Single-Strand Break Repair: Mechanisms and Links with Chromatin. DNA Repair. 2007;6:443–453. doi: 10.1016/j.dnarep.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 84.Spiegel J.O., Van Houten B., Durrant J.D. PARP1: Structural Insights and Pharmacological _targets for Inhibition. DNA Repair. 2021;103:103125. doi: 10.1016/j.dnarep.2021.103125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.van den Bosch M., Bree R.T., Lowndes N.F. The MRN Complex: Coordinating and Mediating the Response to Broken Chromosomes. EMBO Rep. 2003;4:844–849. doi: 10.1038/sj.embor.embor925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Qiu S., Huang J. MRN Complex Is an Essential Effector of DNA Damage Repair. J. Zhejiang Univ. Sci. B. 2021;22:31–37. doi: 10.1631/jzus.B2000289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lamarche B.J., Orazio N.I., Weitzman M.D. The MRN Complex in Double-Strand Break Repair and Telomere Maintenance. FEBS Lett. 2010;584:3682–3695. doi: 10.1016/j.febslet.2010.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yue X., Bai C., Xie D., Ma T., Zhou P.-K. DNA-PKcs: A Multi-Faceted Player in DNA Damage Response. Front. Genet. 2020;11:607428. doi: 10.3389/fgene.2020.607428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dylgjeri E., Knudsen K.E. DNA-PKcs: A _targetable Protumorigenic Protein Kinase. Cancer Res. 2022;82:523–533. doi: 10.1158/0008-5472.CAN-21-1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Amani J., Gorjizadeh N., Younesi S., Najafi M., Ashrafi A.M., Irian S., Gorjizadeh N., Azizian K. Cyclin-Dependent Kinase Inhibitors (CDKIs) and the DNA Damage Response: The Link between Signaling Pathways and Cancer. DNA Repair. 2021;102:103103. doi: 10.1016/j.dnarep.2021.103103. [DOI] [PubMed] [Google Scholar]
- 91.Kciuk M., Gielecińska A., Mujwar S., Mojzych M., Kontek R. Cyclin-Dependent Kinase Synthetic Lethality Partners in DNA Damage Response. Int. J. Mol. Sci. 2022;23:3555. doi: 10.3390/ijms23073555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lim S., Kaldis P. Cdks, Cyclins and CKIs: Roles beyond Cell Cycle Regulation. Development. 2013;140:3079–3093. doi: 10.1242/dev.091744. [DOI] [PubMed] [Google Scholar]
- 93.Kurz E.U., Douglas P., Lees-Miller S.P. Doxorubicin Activates ATM-Dependent Phosphorylation of Multiple Downstream _targets in Part through the Generation of Reactive Oxygen Species. J. Biol. Chem. 2004;279:53272–53281. doi: 10.1074/jbc.M406879200. [DOI] [PubMed] [Google Scholar]
- 94.Théard D., Coisy M., Ducommun B., Concannon P., Darbon J.M. Etoposide and Adriamycin but Not Genistein Can Activate the Checkpoint Kinase Chk2 Independently of ATM/ATR. Biochem. Biophys. Res. Commun. 2001;289:1199–1204. doi: 10.1006/bbrc.2001.6095. [DOI] [PubMed] [Google Scholar]
- 95.Ghelli Luserna Di Rorà A., Ghetti M., Ledda L., Ferrari A., Bocconcelli M., Padella A., Napolitano R., Fontana M.C., Liverani C., Imbrogno E., et al. Exploring the ATR-CHK1 Pathway in the Response of Doxorubicin-Induced DNA Damages in Acute Lymphoblastic Leukemia Cells. Cell Biol. Toxicol. :2021. doi: 10.1007/s10565-021-09640-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Batey M.A., Zhao Y., Kyle S., Richardson C., Slade A., Martin N.M.B., Lau A., Newell D.R., Curtin N.J. Preclinical Evaluation of a Novel ATM Inhibitor, KU59403, in Vitro and in Vivo in P53 Functional and Dysfunctional Models of Human Cancer. Mol. Cancer Ther. 2013;12:959–967. doi: 10.1158/1535-7163.MCT-12-0707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cui J., Dean D., Hornicek F.J., Pollock R.E., Hoffman R.M., Duan Z. ATR Inhibition Sensitizes Liposarcoma to Doxorubicin by Increasing DNA Damage. Am. J. Cancer Res. 2022;12:1577–1592. [PMC free article] [PubMed] [Google Scholar]
- 98.Baranski Z., Booij T.H., Cleton-Jansen A.-M., Price L.S., van de Water B., Bovée J.V.M.G., Hogendoorn P.C.W., Danen E.H.J. Aven-Mediated Checkpoint Kinase Control Regulates Proliferation and Resistance to Chemotherapy in Conventional Osteosarcoma. J. Pathol. 2015;236:348–359. doi: 10.1002/path.4528. [DOI] [PubMed] [Google Scholar]
- 99.Chung S.W., Kim G.C., Kweon S., Lee H., Choi J.U., Mahmud F., Chang H.W., Kim J.W., Son W.-C., Kim S.Y., et al. Metronomic Oral Doxorubicin in Combination of Chk1 Inhibitor MK-8776 for P53-Deficient Breast Cancer Treatment. Biomaterials. 2018;182:35–43. doi: 10.1016/j.biomaterials.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 100.Weng M.-T., Tung T.-H., Lee J.-H., Wei S.-C., Lin H.-L., Huang Y.-J., Wong J.-M., Luo J., Sheu J.-C. Enhancer of Rudimentary Homolog Regulates DNA Damage Response in Hepatocellular Carcinoma. Sci. Rep. 2015;5:9357. doi: 10.1038/srep09357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Davidson D., Grenier J., Martinez-Marignac V., Amrein L., Shawi M., Tokars M., Aloyz R., Panasci L. Effects of the Novel DNA Dependent Protein Kinase Inhibitor, IC486241, on the DNA Damage Response to Doxorubicin and Cisplatin in Breast Cancer Cells. Investig. New Drugs. 2012;30:1736–1742. doi: 10.1007/s10637-011-9678-5. [DOI] [PubMed] [Google Scholar]
- 102.Park H.J., Bae J.S., Kim K.M., Moon Y.J., Park S.-H., Ha S.H., Hussein U.K., Zhang Z., Park H.S., Park B.-H., et al. The PARP Inhibitor Olaparib Potentiates the Effect of the DNA Damaging Agent Doxorubicin in Osteosarcoma. J. Exp. Clin. Cancer Res. 2018;37:107. doi: 10.1186/s13046-018-0772-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kim H.-S., Lee Y.-S., Kim D.-K. Doxorubicin Exerts Cytotoxic Effects through Cell Cycle Arrest and Fas-Mediated Cell Death. Pharmacology. 2009;84:300–309. doi: 10.1159/000245937. [DOI] [PubMed] [Google Scholar]
- 104.Bar-On O., Shapira M., Hershko D.D. Differential Effects of Doxorubicin Treatment on Cell Cycle Arrest and Skp2 Expression in Breast Cancer Cells. Anticancer Drugs. 2007;18:1113–1121. doi: 10.1097/CAD.0b013e3282ef4571. [DOI] [PubMed] [Google Scholar]
- 105.Ling Y.H., el-Naggar A.K., Priebe W., Perez-Soler R. Cell Cycle-Dependent Cytotoxicity, G2/M Phase Arrest, and Disruption of P34cdc2/Cyclin B1 Activity Induced by Doxorubicin in Synchronized P388 Cells. Mol. Pharmacol. 1996;49:832–841. [PubMed] [Google Scholar]
- 106.Lüpertz R., Wätjen W., Kahl R., Chovolou Y. Dose- and Time-Dependent Effects of Doxorubicin on Cytotoxicity, Cell Cycle and Apoptotic Cell Death in Human Colon Cancer Cells. Toxicology. 2010;271:115–121. doi: 10.1016/j.tox.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 107.Sarniak A., Lipińska J., Tytman K., Lipińska S. Endogenous Mechanisms of Reactive Oxygen Species (ROS) Generation. Postep. Hig. Med. Dosw. (Online) 2016;70:1150–1165. doi: 10.5604/17322693.1224259. [DOI] [PubMed] [Google Scholar]
- 108.Zorov D.B., Juhaszova M., Sollott S.J. Mitochondrial Reactive Oxygen Species (ROS) and ROS-Induced ROS Release. Physiol. Rev. 2014;94:909–950. doi: 10.1152/physrev.00026.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cadet J., Douki T., Ravanat J.-L. Oxidatively Generated Base Damage to Cellular DNA. Free Radic. Biol. Med. 2010;49:9–21. doi: 10.1016/j.freeradbiomed.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 110.Cadet J., Davies K.J.A. Oxidative DNA Damage & Repair: An Introduction. Free Radic. Biol. Med. 2017;107:2–12. doi: 10.1016/j.freeradbiomed.2017.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Simon H.U., Haj-Yehia A., Levi-Schaffer F. Role of Reactive Oxygen Species (ROS) in Apoptosis Induction. Apoptosis. 2000;5:415–418. doi: 10.1023/A:1009616228304. [DOI] [PubMed] [Google Scholar]
- 112.Redza-Dutordoir M., Averill-Bates D.A. Activation of Apoptosis Signalling Pathways by Reactive Oxygen Species. Biochim. Biophys. Acta. 2016;1863:2977–2992. doi: 10.1016/j.bbamcr.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 113.Kuczler M.D., Olseen A.M., Pienta K.J., Amend S.R. ROS-Induced Cell Cycle Arrest as a Mechanism of Resistance in Polyaneuploid Cancer Cells (PACCs) Prog. Biophys. Mol. Biol. 2021;165:3–7. doi: 10.1016/j.pbiomolbio.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chatterjee S., Kundu S., Sengupta S., Bhattacharyya A. Divergence to Apoptosis from ROS Induced Cell Cycle Arrest: Effect of Cadmium. Mutat. Res. 2009;663:22–31. doi: 10.1016/j.mrfmmm.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 115.Victorelli S., Passos J.F. Reactive Oxygen Species Detection in Senescent Cells. Methods Mol. Biol. 2019;1896:21–29. doi: 10.1007/978-1-4939-8931-7_3. [DOI] [PubMed] [Google Scholar]
- 116.Benkafadar N., François F., Affortit C., Casas F., Ceccato J.-C., Menardo J., Venail F., Malfroy-Camine B., Puel J.-L., Wang J. ROS-Induced Activation of DNA Damage Responses Drives Senescence-Like State in Postmitotic Cochlear Cells: Implication for Hearing Preservation. Mol. Neurobiol. 2019;56:5950–5969. doi: 10.1007/s12035-019-1493-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Davalli P., Mitic T., Caporali A., Lauriola A., D’Arca D. ROS, Cell Senescence, and Novel Molecular Mechanisms in Aging and Age-Related Diseases. Oxidative Med. Cell. Longev. 2016;2016:3565127. doi: 10.1155/2016/3565127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bertram C., Hass R. Cellular Responses to Reactive Oxygen Species-Induced DNA Damage and Aging. Biol. Chem. 2008;389:211–220. doi: 10.1515/BC.2008.031. [DOI] [PubMed] [Google Scholar]
- 119.Gilliam L.A.A., Moylan J.S., Patterson E.W., Smith J.D., Wilson A.S., Rabbani Z., Reid M.B. Doxorubicin Acts via Mitochondrial ROS to Stimulate Catabolism in C2C12 Myotubes. Am. J. Physiol. Cell Physiol. 2012;302:C195–C202. doi: 10.1152/ajpcell.00217.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Goormaghtigh E., Huart P., Praet M., Brasseur R., Ruysschaert J.M. Structure of the Adriamycin-Cardiolipin Complex. Role in Mitochondrial Toxicity. Biophys. Chem. 1990;35:247–257. doi: 10.1016/0301-4622(90)80012-V. [DOI] [PubMed] [Google Scholar]
- 121.Gorini S., De Angelis A., Berrino L., Malara N., Rosano G., Ferraro E. Chemotherapeutic Drugs and Mitochondrial Dysfunction: Focus on Doxorubicin, Trastuzumab, and Sunitinib. Oxidative Med. Cell. Longev. 2018;2018:7582730. doi: 10.1155/2018/7582730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Montalvo R.N., Doerr V., Min K., Szeto H.H., Smuder A.J. Doxorubicin-Induced Oxidative Stress Differentially Regulates Proteolytic Signaling in Cardiac and Skeletal Muscle. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2020;318:R227–R233. doi: 10.1152/ajpregu.00299.2019. [DOI] [PubMed] [Google Scholar]
- 123.Kalivendi S.V., Konorev E.A., Cunningham S., Vanamala S.K., Kaji E.H., Joseph J., Kalyanaraman B. Doxorubicin Activates Nuclear Factor of Activated T-Lymphocytes and Fas Ligand Transcription: Role of Mitochondrial Reactive Oxygen Species and Calcium. Biochem. J. 2005;389:527–539. doi: 10.1042/BJ20050285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhao L., Zhang B. Doxorubicin Induces Cardiotoxicity through Upregulation of Death Receptors Mediated Apoptosis in Cardiomyocytes. Sci. Rep. 2017;7:44735. doi: 10.1038/srep44735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.McSweeney K.M., Bozza W.P., Alterovitz W.-L., Zhang B. Transcriptomic Profiling Reveals P53 as a Key Regulator of Doxorubicin-Induced Cardiotoxicity. Cell Death Discov. 2019;5:102. doi: 10.1038/s41420-019-0182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Zhou S., Palmeira C.M., Wallace K.B. Doxorubicin-Induced Persistent Oxidative Stress to Cardiac Myocytes. Toxicol. Lett. 2001;121:151–157. doi: 10.1016/S0378-4274(01)00329-0. [DOI] [PubMed] [Google Scholar]
- 127.Zhang S., Liu X., Bawa-Khalfe T., Lu L.-S., Lyu Y.L., Liu L.F., Yeh E.T.H. Identification of the Molecular Basis of Doxorubicin-Induced Cardiotoxicity. Nat. Med. 2012;18:1639–1642. doi: 10.1038/nm.2919. [DOI] [PubMed] [Google Scholar]
- 128.Wang Z., Wang J., Xie R., Liu R., Lu Y. Mitochondria-Derived Reactive Oxygen Species Play an Important Role in Doxorubicin-Induced Platelet Apoptosis. Int. J. Mol. Sci. 2015;16:11087–11100. doi: 10.3390/ijms160511087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kim S.-Y., Kim S.-J., Kim B.-J., Rah S.-Y., Chung S.M., Im M.-J., Kim U.-H. Doxorubicin-Induced Reactive Oxygen Species Generation and Intracellular Ca2+ Increase Are Reciprocally Modulated in Rat Cardiomyocytes. Exp. Mol. Med. 2006;38:535–545. doi: 10.1038/emm.2006.63. [DOI] [PubMed] [Google Scholar]
- 130.Ma J., Wang Y., Zheng D., Wei M., Xu H., Peng T. Rac1 Signalling Mediates Doxorubicin-Induced Cardiotoxicity through Both Reactive Oxygen Species-Dependent and -Independent Pathways. Cardiovasc. Res. 2013;97:77–87. doi: 10.1093/cvr/cvs309. [DOI] [PubMed] [Google Scholar]
- 131.Asensio-López M.C., Soler F., Pascual-Figal D., Fernández-Belda F., Lax A. Doxorubicin-Induced Oxidative Stress: The Protective Effect of Nicorandil on HL-1 Cardiomyocytes. PLoS ONE. 2017;12:e0172803. doi: 10.1371/journal.pone.0172803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Antonucci S., Di Sante M., Tonolo F., Pontarollo L., Scalcon V., Alanova P., Menabò R., Carpi A., Bindoli A., Rigobello M.P., et al. The Determining Role of Mitochondrial Reactive Oxygen Species Generation and Monoamine Oxidase Activity in Doxorubicin-Induced Cardiotoxicity. Antioxid. Redox Signal. 2021;34:531–550. doi: 10.1089/ars.2019.7929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Songbo M., Lang H., Xinyong C., Bin X., Ping Z., Liang S. Oxidative Stress Injury in Doxorubicin-Induced Cardiotoxicity. Toxicol. Lett. 2019;307:41–48. doi: 10.1016/j.toxlet.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 134.Olson R.D., Mushlin P.S. Doxorubicin Cardiotoxicity: Analysis of Prevailing Hypotheses. FASEB J. 1990;4:3076–3086. doi: 10.1096/fasebj.4.13.2210154. [DOI] [PubMed] [Google Scholar]
- 135.Dos Santos Arruda F., Tomé F.D., Miguel M.P., de Menezes L.B., Nagib P.R.A., Campos E.C., Soave D.F., Celes M.R.N. Doxorubicin-Induced Cardiotoxicity and Cardioprotective Agents: Classic and New Players in the Game. Curr. Pharm. Des. 2019;25:109–118. doi: 10.2174/1381612825666190312110836. [DOI] [PubMed] [Google Scholar]
- 136.Cappetta D., De Angelis A., Sapio L., Prezioso L., Illiano M., Quaini F., Rossi F., Berrino L., Naviglio S., Urbanek K. Oxidative Stress and Cellular Response to Doxorubicin: A Common Factor in the Complex Milieu of Anthracycline Cardiotoxicity. Oxidative Med. Cell. Longev. 2017;2017:1521020. doi: 10.1155/2017/1521020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Guo Z., Kozlov S., Lavin M.F., Person M.D., Paull T.T. ATM Activation by Oxidative Stress. Science. 2010;330:517–521. doi: 10.1126/science.1192912. [DOI] [PubMed] [Google Scholar]
- 138.Xie X., Zhang Y., Wang Z., Wang S., Jiang X., Cui H., Zhou T., He Z., Feng H., Guo Q., et al. ATM at the Crossroads of Reactive Oxygen Species and Autophagy. Int. J. Biol. Sci. 2021;17:3080–3090. doi: 10.7150/ijbs.63963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sarkar A., Gandhi V. Activation of ATM Kinase by ROS Generated during Ionophore-Induced Mitophagy in Human T and B Cell Malignancies. Mol. Cell. Biochem. 2021;476:417–423. doi: 10.1007/s11010-020-03917-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tsang W.P., Chau S.P.Y., Kong S.K., Fung K.P., Kwok T.T. Reactive Oxygen Species Mediate Doxorubicin Induced P53-Independent Apoptosis. Life Sci. 2003;73:2047–2058. doi: 10.1016/S0024-3205(03)00566-6. [DOI] [PubMed] [Google Scholar]
- 141.Pilco-Ferreto N., Calaf G.M. Influence of Doxorubicin on Apoptosis and Oxidative Stress in Breast Cancer Cell Lines. Int. J. Oncol. 2016;49:753–762. doi: 10.3892/ijo.2016.3558. [DOI] [PubMed] [Google Scholar]
- 142.Navarro R., Busnadiego I., Ruiz-Larrea M.B., Ruiz-Sanz J.I. Superoxide Anions Are Involved in Doxorubicin-Induced ERK Activation in Hepatocyte Cultures. Ann. N. Y. Acad. Sci. 2006;1090:419–428. doi: 10.1196/annals.1378.045. [DOI] [PubMed] [Google Scholar]
- 143.Filippova M., Filippov V., Williams V.M., Zhang K., Kokoza A., Bashkirova S., Duerksen-Hughes P. Cellular Levels of Oxidative Stress Affect the Response of Cervical Cancer Cells to Chemotherapeutic Agents. Biomed. Res. Int. 2014;2014:574659. doi: 10.1155/2014/574659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Luanpitpong S., Chanvorachote P., Nimmannit U., Leonard S.S., Stehlik C., Wang L., Rojanasakul Y. Mitochondrial Superoxide Mediates Doxorubicin-Induced Keratinocyte Apoptosis through Oxidative Modification of ERK and Bcl-2 Ubiquitination. Biochem. Pharmacol. 2012;83:1643–1654. doi: 10.1016/j.bcp.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Aries A., Paradis P., Lefebvre C., Schwartz R.J., Nemer M. Essential Role of GATA-4 in Cell Survival and Drug-Induced Cardiotoxicity. Proc. Natl. Acad. Sci. USA. 2004;101:6975–6980. doi: 10.1073/pnas.0401833101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Doroshow J.H. Mechanisms of Anthracycline-Enhanced Reactive Oxygen Metabolism in Tumor Cells. Oxidative Med. Cell. Longev. 2019;2019:9474823. doi: 10.1155/2019/9474823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Voulgaridou G.-P., Anestopoulos I., Franco R., Panayiotidis M.I., Pappa A. DNA Damage Induced by Endogenous Aldehydes: Current State of Knowledge. Mutat. Res. 2011;711:13–27. doi: 10.1016/j.mrfmmm.2011.03.006. [DOI] [PubMed] [Google Scholar]
- 148.Antonowicz S., Bodai Z., Wiggins T., Markar S.R., Boshier P.R., Goh Y.M., Adam M.E., Lu H., Kudo H., Rosini F., et al. Endogenous Aldehyde Accumulation Generates Genotoxicity and Exhaled Biomarkers in Esophageal Adenocarcinoma. Nat. Commun. 2021;12:1454. doi: 10.1038/s41467-021-21800-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nakamura J., Nakamura M. DNA-Protein Crosslink Formation by Endogenous Aldehydes and AP Sites. DNA Repair. 2020;88:102806. doi: 10.1016/j.dnarep.2020.102806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hlaváčová M., Gumulec J., Stračina T., Fojtů M., Raudenská M., Masařík M., Nováková M., Paulová H. Different Doxorubicin Formulations Affect Plasma 4-Hydroxy-2-Nonenal and Gene Expression of Aldehyde Dehydrogenase 3A1 and Thioredoxin Reductase 2 in Rat. Physiol. Res. 2015;64:S653–S660. doi: 10.33549/physiolres.933223. [DOI] [PubMed] [Google Scholar]
- 151.Luo X., Evrovsky Y., Cole D., Trines J., Benson L.N., Lehotay D.C. Doxorubicin-Induced Acute Changes in Cytotoxic Aldehydes, Antioxidant Status and Cardiac Function in the Rat. Biochim. Biophys. Acta. 1997;1360:45–52. doi: 10.1016/s0925-4439(96)00068-3. [DOI] [PubMed] [Google Scholar]
- 152.Hrelia S., Fiorentini D., Maraldi T., Angeloni C., Bordoni A., Biagi P.L., Hakim G. Doxorubicin Induces Early Lipid Peroxidation Associated with Changes in Glucose Transport in Cultured Cardiomyocytes. Biochim. Biophys. Acta. 2002;1567:150–156. doi: 10.1016/S0005-2736(02)00612-0. [DOI] [PubMed] [Google Scholar]
- 153.Minotti G., Menna P., Salvatorelli E., Cairo G., Gianni L. Anthracyclines: Molecular Advances and Pharmacologic Developments in Antitumor Activity and Cardiotoxicity. Pharmacol. Rev. 2004;56:185–229. doi: 10.1124/pr.56.2.6. [DOI] [PubMed] [Google Scholar]
- 154.Senchenkov A., Litvak D.A., Cabot M.C. _targeting Ceramide Metabolism--a Strategy for Overcoming Drug Resistance. J. Natl. Cancer Inst. 2001;93:347–357. doi: 10.1093/jnci/93.5.347. [DOI] [PubMed] [Google Scholar]
- 155.Kawase M., Watanabe M., Kondo T., Yabu T., Taguchi Y., Umehara H., Uchiyama T., Mizuno K., Okazaki T. Increase of Ceramide in Adriamycin-Induced HL-60 Cell Apoptosis: Detection by a Novel Anti-Ceramide Antibody. Biochim. Biophys. Acta. 2002;1584:104–114. doi: 10.1016/S1388-1981(02)00301-3. [DOI] [PubMed] [Google Scholar]
- 156.Doroshow J.H., Synold T.W., Somlo G., Akman S.A., Gajewski E. Oxidative DNA Base Modifications in Peripheral Blood Mononuclear Cells of Patients Treated with High-Dose Infusional Doxorubicin. Blood. 2001;97:2839–2845. doi: 10.1182/blood.V97.9.2839. [DOI] [PubMed] [Google Scholar]
- 157.Gajewski E., Gaur S., Akman S.A., Matsumoto L., van Balgooy J.N.A., Doroshow J.H. Oxidative DNA Base Damage in MCF-10A Breast Epithelial Cells at Clinically Achievable Concentrations of Doxorubicin. Biochem. Pharmacol. 2007;73:1947–1956. doi: 10.1016/j.bcp.2007.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.García-Ruiz C., Colell A., Marí M., Morales A., Fernández-Checa J.C. Direct Effect of Ceramide on the Mitochondrial Electron Transport Chain Leads to Generation of Reactive Oxygen Species. Role of Mitochondrial Glutathione. J. Biol. Chem. 1997;272:11369–11377. doi: 10.1074/jbc.272.17.11369. [DOI] [PubMed] [Google Scholar]
- 159.Chang Y.C., Fong Y., Tsai E.-M., Chang Y.-G., Chou H.L., Wu C.-Y., Teng Y.-N., Liu T.-C., Yuan S.-S., Chiu C.-C. Exogenous C8-Ceramide Induces Apoptosis by Overproduction of ROS and the Switch of Superoxide Dismutases SOD1 to SOD2 in Human Lung Cancer Cells. Int. J. Mol. Sci. 2018;19:3010. doi: 10.3390/ijms19103010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Siskind L.J. Mitochondrial Ceramide and the Induction of Apoptosis. J. Bioenerg. Biomembr. 2005;37:143–153. doi: 10.1007/s10863-005-6567-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Woodcock J. Sphingosine and Ceramide Signalling in Apoptosis. IUBMB Life. 2006;58:462–466. doi: 10.1080/15216540600871118. [DOI] [PubMed] [Google Scholar]
- 162.Mullen T.D., Obeid L.M. Ceramide and Apoptosis: Exploring the Enigmatic Connections between Sphingolipid Metabolism and Programmed Cell Death. Anticancer Agents Med. Chem. 2012;12:340–363. doi: 10.2174/187152012800228661. [DOI] [PubMed] [Google Scholar]
- 163.Khodadust R., Alpsoy A., Ünsoy G., GÜndÜz U. Poly (I:C)- and Doxorubicin-Loaded Magnetic Dendrimeric Nanoparticles Affect the Apoptosis-Related Gene Expressions in MCF-7 Cells. Turk. J. Biol. 2020;44:133–144. doi: 10.3906/biy-1912-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Bojko A., Czarnecka-Herok J., Charzynska A., Dabrowski M., Sikora E. Diversity of the Senescence Phenotype of Cancer Cells Treated with Chemotherapeutic Agents. Cells. 2019;8:1501. doi: 10.3390/cells8121501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hu X., Zhang H. Doxorubicin-Induced Cancer Cell Senescence Shows a Time Delay Effect and Is Inhibited by Epithelial-Mesenchymal Transition (EMT) Med. Sci. Monit. 2019;25:3617–3623. doi: 10.12659/MSM.914295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hernandez-Segura A., Nehme J., Demaria M. Hallmarks of Cellular Senescence. Trends Cell. Biol. 2018;28:436–453. doi: 10.1016/j.tcb.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 167.Dodig S., Čepelak I., Pavić I. Hallmarks of Senescence and Aging. Biochem. Med. 2019;29:030501. doi: 10.11613/BM.2019.030501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Joyner D.E., Bastar J.D., Randall R.L. Doxorubicin Induces Cell Senescence Preferentially over Apoptosis in the FU-SY-1 Synovial Sarcoma Cell Line. J. Orthop. Res. 2006;24:1163–1169. doi: 10.1002/jor.20169. [DOI] [PubMed] [Google Scholar]
- 169.Strzeszewska A., Alster O., Mosieniak G., Ciolko A., Sikora E. Insight into the Role of PIKK Family Members and NF-KB in DNAdamage-Induced Senescence and Senescence-Associated Secretory Phenotype of Colon Cancer Cells. Cell Death Dis. 2018;9:44. doi: 10.1038/s41419-017-0069-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Roninson I.B. Tumor Cell Senescence in Cancer Treatment. Cancer Res. 2003;63:2705–2715. [PubMed] [Google Scholar]
- 171.Yang L., Fang J., Chen J. Tumor Cell Senescence Response Produces Aggressive Variants. Cell Death Discov. 2017;3:17049. doi: 10.1038/cddiscovery.2017.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sliwinska M.A., Mosieniak G., Wolanin K., Babik A., Piwocka K., Magalska A., Szczepanowska J., Fronk J., Sikora E. Induction of Senescence with Doxorubicin Leads to Increased Genomic Instability of HCT116 Cells. Mech. Ageing Dev. 2009;130:24–32. doi: 10.1016/j.mad.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 173.Karabicici M., Alptekin S., Fırtına Karagonlar Z., Erdal E. Doxorubicin-Induced Senescence Promotes Stemness and Tumorigenicity in EpCAM-/CD133- Nonstem Cell Population in Hepatocellular Carcinoma Cell Line, HuH-7. Mol. Oncol. 2021;15:2185–2202. doi: 10.1002/1878-0261.12916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Yang M.-Y., Lin P.-M., Liu Y.-C., Hsiao H.-H., Yang W.-C., Hsu J.-F., Hsu C.-M., Lin S.-F. Induction of Cellular Senescence by Doxorubicin Is Associated with Upregulated MiR-375 and Induction of Autophagy in K562 Cells. PLoS ONE. 2012;7:e37205. doi: 10.1371/journal.pone.0037205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Bientinesi E., Lulli M., Becatti M., Ristori S., Margheri F., Monti D. Doxorubicin-Induced Senescence in Normal Fibroblasts Promotes in Vitro Tumour Cell Growth and Invasiveness: The Role of Quercetin in Modulating These Processes. Mech. Ageing Dev. 2022;206:111689. doi: 10.1016/j.mad.2022.111689. [DOI] [PubMed] [Google Scholar]
- 176.Marques L., Johnson A.A., Stolzing A. Doxorubicin Generates Senescent Microglia That Exhibit Altered Proteomes, Higher Levels of Cytokine Secretion, and a Decreased Ability to Internalize Amyloid β. Exp. Cell Res. 2020;395:112203. doi: 10.1016/j.yexcr.2020.112203. [DOI] [PubMed] [Google Scholar]
- 177.Piegari E., De Angelis A., Cappetta D., Russo R., Esposito G., Costantino S., Graiani G., Frati C., Prezioso L., Berrino L., et al. Doxorubicin Induces Senescence and Impairs Function of Human Cardiac Progenitor Cells. Basic Res. Cardiol. 2013;108:334. doi: 10.1007/s00395-013-0334-4. [DOI] [PubMed] [Google Scholar]
- 178.Spallarossa P., Altieri P., Aloi C., Garibaldi S., Barisione C., Ghigliotti G., Fugazza G., Barsotti A., Brunelli C. Doxorubicin Induces Senescence or Apoptosis in Rat Neonatal Cardiomyocytes by Regulating the Expression Levels of the Telomere Binding Factors 1 and 2. Am. J. Physiol. Heart Circ. Physiol. 2009;297:H2169–H2181. doi: 10.1152/ajpheart.00068.2009. [DOI] [PubMed] [Google Scholar]
- 179.Mitry M.A., Laurent D., Keith B.L., Sira E., Eisenberg C.A., Eisenberg L.M., Joshi S., Gupte S., Edwards J.G. Accelerated Cardiomyocyte Senescence Contributes to Late-Onset Doxorubicin-Induced Cardiotoxicity. Am. J. Physiol. Cell Physiol. 2020;318:C380–C391. doi: 10.1152/ajpcell.00073.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Bashiri Dezfouli A., Salar-Amoli J., Pourfathollah A.A., Yazdi M., Nikougoftar-Zarif M., Khosravi M., Hassan J. Doxorubicin-Induced Senescence through NF-ΚB Affected by the Age of Mouse Mesenchymal Stem Cells. J. Cell. Physiol. 2020;235:2336–2349. doi: 10.1002/jcp.29140. [DOI] [PubMed] [Google Scholar]
- 181.Sultana R., Di Domenico F., Tseng M., Cai J., Noel T., Chelvarajan R.L., Pierce W.D., Cini C., Bondada S., St Clair D.K., et al. Doxorubicin-Induced Thymus Senescence. J. Proteome Res. 2010;9:6232–6241. doi: 10.1021/pr100465m. [DOI] [PubMed] [Google Scholar]
- 182.Mathew R., Karantza-Wadsworth V., White E. Role of Autophagy in Cancer. Nat. Rev. Cancer. 2007;7:961–967. doi: 10.1038/nrc2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zhao D., Yuan H., Yi F., Meng C., Zhu Q. Autophagy Prevents Doxorubicin-induced Apoptosis in Osteosarcoma. Mol. Med. Rep. 2014;9:1975–1981. doi: 10.3892/mmr.2014.2055. [DOI] [PubMed] [Google Scholar]
- 184.Guo B., Tam A., Santi S.A., Parissenti A.M. Role of Autophagy and Lysosomal Drug Sequestration in Acquired Resistance to Doxorubicin in MCF-7 Cells. BMC Cancer. 2016;16:762. doi: 10.1186/s12885-016-2790-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sishi B.J.N., Loos B., van Rooyen J., Engelbrecht A.-M. Autophagy Upregulation Promotes Survival and Attenuates Doxorubicin-Induced Cardiotoxicity. Biochem. Pharmacol. 2013;85:124–134. doi: 10.1016/j.bcp.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 186.Loh J.S., Rahim N.A., Tor Y.S., Foo J.B. Simultaneous Proteasome and Autophagy Inhibition Synergistically Enhances Cytotoxicity of Doxorubicin in Breast Cancer Cells. Cell Biochem. Funct. 2022;40:403–416. doi: 10.1002/cbf.3704. [DOI] [PubMed] [Google Scholar]
- 187.Aydinlik S., Erkisa M., Cevatemre B., Sarimahmut M., Dere E., Ari F., Ulukaya E. Enhanced Cytotoxic Activity of Doxorubicin through the Inhibition of Autophagy in Triple Negative Breast Cancer Cell Line. Biochim. Biophys. Acta Gen. Subj. 2017;1861:49–57. doi: 10.1016/j.bbagen.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 188.Hu C., Gu F., Gong C., Xia Q., Gao Y., Gao S. Co-Delivery of the Autophagy Inhibitor Si-Beclin1 and the Doxorubicin Nano-Delivery System for Advanced Prostate Cancer Treatment. J. Biomater. Appl. 2022;36:1317–1331. doi: 10.1177/08853282211060252. [DOI] [PubMed] [Google Scholar]
- 189.Christidi E., Brunham L.R. Regulated Cell Death Pathways in Doxorubicin-Induced Cardiotoxicity. Cell Death Dis. 2021;12:339. doi: 10.1038/s41419-021-03614-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Yang R., Li Y., Wang X., Yan J., Pan D., Xu Y., Wang L., Yang M. Doxorubicin Loaded Ferritin Nanoparticles for Ferroptosis Enhanced _targeted Killing of Cancer Cells. RSC Adv. 2019;9:28548–28553. doi: 10.1039/C9RA04478G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Xue C.-C., Li M.-H., Zhao Y., Zhou J., Hu Y., Cai K.-Y., Zhao Y., Yu S.-H., Luo Z. Tumor Microenvironment-Activatable Fe-Doxorubicin Preloaded Amorphous CaCO3 Nanoformulation Triggers Ferroptosis in _target Tumor Cells. Sci. Adv. 2020;6:eaax1346. doi: 10.1126/sciadv.aax1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Yang Y., Zuo S., Li L., Kuang X., Li J., Sun B., Wang S., He Z., Sun J. Iron-Doxorubicin Prodrug Loaded Liposome Nanogenerator Programs Multimodal Ferroptosis for Efficient Cancer Therapy. Asian J. Pharm. Sci. 2021;16:784–793. doi: 10.1016/j.ajps.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Ji P., Wang X., Yin J., Yao Y., Du W. Amplification of Ferroptosis with a Liposomal Nanoreactor Cooperates with Low-Toxicity Doxorubicin Apoptosis for Enhanced Tumor Chemotherapy. Biomater. Sci. 2022;10:1544–1553. doi: 10.1039/D2BM00079B. [DOI] [PubMed] [Google Scholar]
- 194.Bano I., Horky P., Abbas S.Q., Majid M., Bilal A.H.M., Ali F., Behl T., Shams ul Hassan S., Bungau S. Ferroptosis: A New Road towards Cancer Management. Molecules. 2022;27:2129. doi: 10.3390/molecules27072129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Wang L., Qin X., Liang J., Ge P. Induction of Pyroptosis: A Promising Strategy for Cancer Treatment. Front. Oncol. 2021;11:635774. doi: 10.3389/fonc.2021.635774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Xia X., Wang X., Cheng Z., Qin W., Lei L., Jiang J., Hu J. The Role of Pyroptosis in Cancer: Pro-Cancer or pro-“Host”? Cell Death Dis. 2019;10:650. doi: 10.1038/s41419-019-1883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Meng L., Lin H., Zhang J., Lin N., Sun Z., Gao F., Luo H., Ni T., Luo W., Chi J., et al. Doxorubicin Induces Cardiomyocyte Pyroptosis via the TINCR-Mediated Posttranscriptional Stabilization of NLR Family Pyrin Domain Containing 3. J. Mol. Cell. Cardiol. 2019;136:15–26. doi: 10.1016/j.yjmcc.2019.08.009. [DOI] [PubMed] [Google Scholar]
- 198.Dessouki F.B.A., Kukreja R.C., Singla D.K. Stem Cell-Derived Exosomes Ameliorate Doxorubicin-Induced Muscle Toxicity through Counteracting Pyroptosis. Pharmaceuticals. 2020;13:450. doi: 10.3390/ph13120450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zhang Z., Zhang H., Li D., Zhou X., Qin Q., Zhang Q. Caspase-3-Mediated GSDME Induced Pyroptosis in Breast Cancer Cells through the ROS/JNK Signalling Pathway. J. Cell. Mol. Med. 2021;25:8159–8168. doi: 10.1111/jcmm.16574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Yu P., Wang H.-Y., Tian M., Li A.-X., Chen X.-S., Wang X.-L., Zhang Y., Cheng Y. Eukaryotic Elongation Factor-2 Kinase Regulates the Cross-Talk between Autophagy and Pyroptosis in Doxorubicin-Treated Human Melanoma Cells in Vitro. Acta Pharmacol. Sin. 2019;40:1237–1244. doi: 10.1038/s41401-019-0222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Konstantinidou M., Zarganes-Tzitzikas T., Magiera-Mularz K., Holak T.A., Dömling A. Immune Checkpoint PD-1/PD-L1: Is There Life Beyond Antibodies? Angew. Chem. Int. Ed. Engl. 2018;57:4840–4848. doi: 10.1002/anie.201710407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Terenzi A., Pirker C., Keppler B.K., Berger W. Anticancer Metal Drugs and Immunogenic Cell Death. J. Inorg. Biochem. 2016;165:71–79. doi: 10.1016/j.jinorgbio.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 203.Kythreotou A., Siddique A., Mauri F.A., Bower M., Pinato D.J. PD-L1. J. Clin. Pathol. 2018;71:189–194. doi: 10.1136/jclinpath-2017-204853. [DOI] [PubMed] [Google Scholar]
- 204.Galluzzi L., Buqué A., Kepp O., Zitvogel L., Kroemer G. Immunological Effects of Conventional Chemotherapy and _targeted Anticancer Agents. Cancer Cell. 2015;28:690–714. doi: 10.1016/j.ccell.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 205.Mattarollo S.R., Loi S., Duret H., Ma Y., Zitvogel L., Smyth M.J. Pivotal Role of Innate and Adaptive Immunity in Anthracycline Chemotherapy of Established Tumors. Cancer Res. 2011;71:4809–4820. doi: 10.1158/0008-5472.CAN-11-0753. [DOI] [PubMed] [Google Scholar]
- 206.Park J.Y., Jang M.J., Chung Y.H., Kim K.Y., Kim S.S., Lee W.B., You S., Choi Y.S., Hur D.Y., Kim D. Doxorubicin Enhances CD4(+) T-Cell Immune Responses by Inducing Expression of CD40 Ligand and 4-1BB. Int. Immunopharmacol. 2009;9:1530–1539. doi: 10.1016/j.intimp.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 207.Zirakzadeh A.A., Kinn J., Krantz D., Rosenblatt R., Winerdal M.E., Hu J., Hartana C.A., Lundgren C., Bergman E.A., Johansson M., et al. Doxorubicin Enhances the Capacity of B Cells to Activate T Cells in Urothelial Urinary Bladder Cancer. Clin. Immunol. 2017;176:63–70. doi: 10.1016/j.clim.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 208.Bedi D., Henderson H.J., Manne U., Samuel T. Camptothecin Induces PD-L1 and Immunomodulatory Cytokines in Colon Cancer Cells. Medicines. 2019;6:51. doi: 10.3390/medicines6020051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gilad Y., Eliaz Y., Yu Y., Han S.J., O’Malley B.W., Lonard D.M. Drug-Induced PD-L1 Expression and Cell Stress Response in Breast Cancer Cells Can Be Balanced by Drug Combination. Sci. Rep. 2019;9:15099. doi: 10.1038/s41598-019-51537-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Voorwerk L., Slagter M., Horlings H.M., Sikorska K., van de Vijver K.K., de Maaker M., Nederlof I., Kluin R.J.C., Warren S., Ong S., et al. Immune Induction Strategies in Metastatic Triple-Negative Breast Cancer to Enhance the Sensitivity to PD-1 Blockade: The TONIC Trial. Nat. Med. 2019;25:920–928. doi: 10.1038/s41591-019-0432-4. [DOI] [PubMed] [Google Scholar]
- 211.Wang J., Hu C., Wang J., Shen Y., Bao Q., He F., Wang H., Gong L., Liu Z., Hu F., et al. Checkpoint Blockade in Combination With Doxorubicin Augments Tumor Cell Apoptosis in Osteosarcoma. J. Immunother. 2019;42:321–330. doi: 10.1097/CJI.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 212.Iwai T., Sugimoto M., Wakita D., Yorozu K., Kurasawa M., Yamamoto K. Topoisomerase I Inhibitor, Irinotecan, Depletes Regulatory T Cells and up-Regulates MHC Class I and PD-L1 Expression, Resulting in a Supra-Additive Antitumor Effect When Combined with Anti-PD-L1 Antibodies. Onco_target. 2018;9:31411–31421. doi: 10.18632/onco_target.25830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Zhu X., Xu J., Cai H., Lang J. Carboplatin and Programmed Death-Ligand 1 Blockade Synergistically Produce a Similar Antitumor Effect to Carboplatin Alone in Murine ID8 Ovarian Cancer Model. J. Obstet. Gynaecol. Res. 2018;44:303–311. doi: 10.1111/jog.13521. [DOI] [PubMed] [Google Scholar]
- 214.Wahba J., Natoli M., Whilding L.M., Parente-Pereira A.C., Jung Y., Zona S., Lam E.W.-F., Smith J.R., Maher J., Ghaem-Maghami S. Chemotherapy-Induced Apoptosis, Autophagy and Cell Cycle Arrest Are Key Drivers of Synergy in Chemo-Immunotherapy of Epithelial Ovarian Cancer. Cancer Immunol. Immunother. 2018;67:1753–1765. doi: 10.1007/s00262-018-2199-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Fournel L., Wu Z., Stadler N., Damotte D., Lococo F., Boulle G., Ségal-Bendirdjian E., Bobbio A., Icard P., Trédaniel J., et al. Cisplatin Increases PD-L1 Expression and Optimizes Immune Check-Point Blockade in Non-Small Cell Lung Cancer. Cancer Lett. 2019;464:5–14. doi: 10.1016/j.canlet.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 216.Tran L., Allen C.T., Xiao R., Moore E., Davis R., Park S.-J., Spielbauer K., Van Waes C., Schmitt N.C. Cisplatin Alters Antitumor Immunity and Synergizes with PD-1/PD-L1 Inhibition in Head and Neck Squamous Cell Carcinoma. Cancer Immunol. Res. 2017;5:1141–1151. doi: 10.1158/2326-6066.CIR-17-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Ock C.-Y., Kim S., Keam B., Kim S., Ahn Y.-O., Chung E.-J., Kim J.-H., Kim T.M., Kwon S.K., Jeon Y.K., et al. Changes in Programmed Death-Ligand 1 Expression during Cisplatin Treatment in Patients with Head and Neck Squamous Cell Carcinoma. Onco_target. 2017;8:97920–97927. doi: 10.18632/onco_target.18542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Tsai T.-F., Lin J.-F., Lin Y.-C., Chou K.-Y., Chen H.-E., Ho C.-Y., Chen P.-C., Hwang T.I.-S. Cisplatin Contributes to Programmed Death-Ligand 1 Expression in Bladder Cancer through ERK1/2-AP-1 Signaling Pathway. Biosci. Rep. 2019;39:BSR20190362. doi: 10.1042/BSR20190362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Qin X., Liu C., Zhou Y., Wang G. Cisplatin Induces Programmed Death-1-Ligand 1(PD-L1) over-Expression in Hepatoma H22 Cells via Erk /MAPK Signaling Pathway. Cell. Mol. Biol. 2010;56:1366–1372. [PubMed] [Google Scholar]
- 220.Wu X., Li Y., Liu X., Chen C., Harrington S.M., Cao S., Xie T., Pham T., Mansfield A.S., Yan Y., et al. _targeting B7-H1 (PD-L1) Sensitizes Cancer Cells to Chemotherapy. Heliyon. 2018;4:e01039. doi: 10.1016/j.heliyon.2018.e01039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Sato H., Niimi A., Yasuhara T., Permata T.B.M., Hagiwara Y., Isono M., Nuryadi E., Sekine R., Oike T., Kakoti S., et al. DNA Double-Strand Break Repair Pathway Regulates PD-L1 Expression in Cancer Cells. Nat. Commun. 2017;8:1751. doi: 10.1038/s41467-017-01883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Doi T., Ishikawa T., Okayama T., Oka K., Mizushima K., Yasuda T., Sakamoto N., Katada K., Kamada K., Uchiyama K., et al. The JAK/STAT Pathway Is Involved in the Upregulation of PD-L1 Expression in Pancreatic Cancer Cell Lines. Oncol. Rep. 2017;37:1545–1554. doi: 10.3892/or.2017.5399. [DOI] [PubMed] [Google Scholar]
- 223.Chen B., Hu J., Hu X., Chen H., Bao R., Zhou Y., Ye Y., Zhan M., Cai W., Li H., et al. DENR Controls JAK2 Translation to Induce PD-L1 Expression for Tumor Immune Evasion. Nat. Commun. 2022;13:2059. doi: 10.1038/s41467-022-29754-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zhao T., Li Y., Zhang J., Zhang B. PD-L1 Expression Increased by IFN-γ via JAK2-STAT1 Signaling and Predicts a Poor Survival in Colorectal Cancer. Oncol. Lett. 2020;20:1127–1134. doi: 10.3892/ol.2020.11647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Zhu J., Li Y., Lv X. IL4I1 Enhances PD-L1 Expression through JAK/STAT Signaling Pathway in Lung Adenocarcinoma. Immunogenetics. 2022;75:17–25. doi: 10.1007/s00251-022-01275-4. [DOI] [PubMed] [Google Scholar]
- 226.Black M., Barsoum I.B., Truesdell P., Cotechini T., Macdonald-Goodfellow S.K., Petroff M., Siemens D.R., Koti M., Craig A.W.B., Graham C.H. Activation of the PD-1/PD-L1 Immune Checkpoint Confers Tumor Cell Chemoresistance Associated with Increased Metastasis. Onco_target. 2016;7:10557–10567. doi: 10.18632/onco_target.7235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Seetharamu N., Preeshagul I.R., Sullivan K.M. New PD-L1 Inhibitors in Non-Small Cell Lung Cancer—Impact of Atezolizumab. Lung Cancer. 2017;8:67–78. doi: 10.2147/LCTT.S113177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Liu X., Guo C.-Y., Tou F.-F., Wen X.-M., Kuang Y.-K., Zhu Q., Hu H. Association of PD-L1 Expression Status with the Efficacy of PD-1/PD-L1 Inhibitors and Overall Survival in Solid Tumours: A Systematic Review and Meta-Analysis. Int. J. Cancer. 2020;147:116–127. doi: 10.1002/ijc.32744. [DOI] [PubMed] [Google Scholar]
- 229.Liu S., Chen S., Yuan W., Wang H., Chen K., Li D., Li D. PD-1/PD-L1 Interaction up-Regulates MDR1/P-Gp Expression in Breast Cancer Cells via PI3K/AKT and MAPK/ERK Pathways. Onco_target. 2017;8:99901–99912. doi: 10.18632/onco_target.21914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Emami F., Banstola A., Vatanara A., Lee S., Kim J.O., Jeong J.-H., Yook S. Doxorubicin and Anti-PD-L1 Antibody Conjugated Gold Nanoparticles for Colorectal Cancer Photochemotherapy. Mol. Pharm. 2019;16:1184–1199. doi: 10.1021/acs.molpharmaceut.8b01157. [DOI] [PubMed] [Google Scholar]
- 231.Bailly C., Thuru X., Quesnel B. Combined Cytotoxic Chemotherapy and Immunotherapy of Cancer: Modern Times. NAR Cancer. 2020;2:zcaa002. doi: 10.1093/narcan/zcaa002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yang M., Liu P., Wang K., Glorieux C., Hu Y., Wen S., Jiang W., Huang P. Chemotherapy Induces Tumor Immune Evasion by Upregulation of Programmed Cell Death Ligand 1 Expression in Bone Marrow Stromal Cells. Mol. Oncol. 2017;11:358–372. doi: 10.1002/1878-0261.12032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Lammers T., Kiessling F., Hennink W.E., Storm G. Drug _targeting to Tumors: Principles, Pitfalls and (Pre-) Clinical Progress. J. Control. Release. 2012;161:175–187. doi: 10.1016/j.jconrel.2011.09.063. [DOI] [PubMed] [Google Scholar]
- 234.Coimbra M., Crielaard B.J., Storm G., Schiffelers R.M. Critical Factors in the Development of Tumor-_targeted Anti-Inflammatory Nanomedicines. J. Control. Release. 2012;160:232–238. doi: 10.1016/j.jconrel.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 235.Akbarzadeh A., Rezaei-Sadabady R., Davaran S., Joo S.W., Zarghami N., Hanifehpour Y., Samiei M., Kouhi M., Nejati-Koshki K. Liposome: Classification, Preparation, and Applications. Nanoscale Res. Lett. 2013;8:102. doi: 10.1186/1556-276X-8-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Liu P., Chen G., Zhang J. A Review of Liposomes as a Drug Delivery System: Current Status of Approved Products, Regulatory Environments, and Future Perspectives. Molecules. 2022;27:1372. doi: 10.3390/molecules27041372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Mishra P., Nayak B., Dey R.K. PEGylation in Anti-Cancer Therapy: An Overview. Asian J. Pharm. Sci. 2016;11:337–348. doi: 10.1016/j.ajps.2015.08.011. [DOI] [Google Scholar]
- 238.Hussain Z., Khan S., Imran M., Sohail M., Shah S.W.A., de Matas M. PEGylation: A Promising Strategy to Overcome Challenges to Cancer-_targeted Nanomedicines: A Review of Challenges to Clinical Transition and Promising Resolution. Drug Deliv. Transl. Res. 2019;9:721–734. doi: 10.1007/s13346-019-00631-4. [DOI] [PubMed] [Google Scholar]
- 239.Eavarone D.A., Yu X., Bellamkonda R.V. _targeted Drug Delivery to C6 Glioma by Transferrin-Coupled Liposomes. J. Biomed. Mater. Res. 2000;51:10–14. doi: 10.1002/(SICI)1097-4636(200007)51:1<10::AID-JBM2>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 240.Paszko E., Senge M.O. Immunoliposomes. Curr. Med. Chem. 2012;19:5239–5277. doi: 10.2174/092986712803833362. [DOI] [PubMed] [Google Scholar]
- 241.Sapra P., Moase E.H., Ma J., Allen T.M. Improved Therapeutic Responses in a Xenograft Model of Human B Lymphoma (Namalwa) for Liposomal Vincristine versus Liposomal Doxorubicin _targeted via Anti-CD19 IgG2a or Fab’ Fragments. Clin. Cancer Res. 2004;10:1100–1111. doi: 10.1158/1078-0432.CCR-03-0041. [DOI] [PubMed] [Google Scholar]
- 242.Sapra P., Allen T.M. Internalizing Antibodies Are Necessary for Improved Therapeutic Efficacy of Antibody-_targeted Liposomal Drugs. Cancer Res. 2002;62:7190–7194. [PubMed] [Google Scholar]
- 243.Cheng W.W.K., Allen T.M. _targeted Delivery of Anti-CD19 Liposomal Doxorubicin in B-Cell Lymphoma: A Comparison of Whole Monoclonal Antibody, Fab’ Fragments and Single Chain Fv. J. Control. Release. 2008;126:50–58. doi: 10.1016/j.jconrel.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 244.Tedder T.F., Poe J.C., Haas K.M. CD22: A Multifunctional Receptor That Regulates B Lymphocyte Survival and Signal Transduction. Adv. Immunol. 2005;88:1–50. doi: 10.1016/S0065-2776(05)88001-0. [DOI] [PubMed] [Google Scholar]
- 245.Tuscano J.M., Martin S.M., Ma Y., Zamboni W., O’Donnell R.T. Efficacy, Biodistribution, and Pharmacokinetics of CD22-_targeted Pegylated Liposomal Doxorubicin in a B-Cell Non-Hodgkin’s Lymphoma Xenograft Mouse Model. Clin. Cancer Res. 2010;16:2760–2768. doi: 10.1158/1078-0432.CCR-09-3199. [DOI] [PubMed] [Google Scholar]
- 246.O’Donnell R.T., Martin S.M., Ma Y., Zamboni W.C., Tuscano J.M. Development and Characterization of CD22-_targeted Pegylated-Liposomal Doxorubicin (IL-PLD) Investig. New Drugs. 2010;28:260–267. doi: 10.1007/s10637-009-9243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Batist G., Barton J., Chaikin P., Swenson C., Welles L. Myocet (Liposome-Encapsulated Doxorubicin Citrate): A New Approach in Breast Cancer Therapy. Expert. Opin. Pharmacother. 2002;3:1739–1751. doi: 10.1517/14656566.3.12.1739. [DOI] [PubMed] [Google Scholar]
- 248.Swenson C.E., Bolcsak L.E., Batist G., Guthrie T.H., Tkaczuk K.H., Boxenbaum H., Welles L., Chow S.-C., Bhamra R., Chaikin P. Pharmacokinetics of Doxorubicin Administered i.v. as Myocet (TLC D-99; Liposome-Encapsulated Doxorubicin Citrate) Compared with Conventional Doxorubicin When given in Combination with Cyclophosphamide in Patients with Metastatic Breast Cancer. Anticancer Drugs. 2003;14:239–246. doi: 10.1097/00001813-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 249.Mross K., Niemann B., Massing U., Drevs J., Unger C., Bhamra R., Swenson C.E. Pharmacokinetics of Liposomal Doxorubicin (TLC-D99; Myocet) in Patients with Solid Tumors: An Open-Label, Single-Dose Study. Cancer Chemother. Pharmacol. 2004;54:514–524. doi: 10.1007/s00280-004-0825-y. [DOI] [PubMed] [Google Scholar]
- 250.Dell’Olio M., Scalzulli R.P., Sanpaolo G., Nobile M., Mantuano F.S., La Sala A., D’Arena G., Miraglia E., Lucania A., Mastrullo L., et al. Non-Pegylated Liposomal Doxorubicin (Myocet®) in Patients with Poor-Risk Aggressive B-Cell Non-Hodgkin Lymphoma. Leuk. Lymphoma. 2011;52:1222–1229. doi: 10.3109/10428194.2011.572321. [DOI] [PubMed] [Google Scholar]
- 251.Viale M., Bertone V., Maric I., Cilli M., Emionite L., Bocchini V., Ponzoni M., Fontana V., De Luca F., Rocco M. Enhanced Therapeutic Index of Liposomal Doxorubicin Myocet Locally Delivered by Fibrin Gels in Immunodeficient Mice Bearing Human Neuroblastoma. Pharmacol. Res. 2021;163:105294. doi: 10.1016/j.phrs.2020.105294. [DOI] [PubMed] [Google Scholar]
- 252.Burade V., Bhowmick S., Maiti K., Zalawadia R., Ruan H., Thennati R. Lipodox® (Generic Doxorubicin Hydrochloride Liposome Injection): In Vivo Efficacy and Bioequivalence versus Caelyx® (Doxorubicin Hydrochloride Liposome Injection) in Human Mammary Carcinoma (MX-1) Xenograft and Syngeneic Fibrosarcoma (WEHI 164) Mouse Models. BMC Cancer. 2017;17:405. doi: 10.1186/s12885-017-3377-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Smith J.A., Costales A.B., Jaffari M., Urbauer D.L., Frumovitz M., Kutac C.K., Tran H., Coleman R.L. Is It Equivalent? Evaluation of the Clinical Activity of Single Agent Lipodox® Compared to Single Agent Doxil® in Ovarian Cancer Treatment. J. Oncol. Pharm. Pract. 2016;22:599–604. doi: 10.1177/1078155215594415. [DOI] [PubMed] [Google Scholar]
- 254.Smith J.A., Mathew L., Burney M., Nyshadham P., Coleman R.L. Equivalency Challenge: Evaluation of Lipodox® as the Generic Equivalent for Doxil® in a Human Ovarian Cancer Orthotropic Mouse Model. Gynecol. Oncol. 2016;141:357–363. doi: 10.1016/j.ygyno.2016.02.033. [DOI] [PubMed] [Google Scholar]
- 255.Sehouli J., Camara O., Schmidt M., Mahner S., Seipelt G., Otremba B., Schmalfeldt B., Tesch H., Lorenz-Schlüter C., Oskay-Ozcelik G., et al. Pegylated Liposomal Doxorubicin (CAELYX) in Patients with Advanced Ovarian Cancer: Results of a German Multicenter Observational Study. Cancer Chemother. Pharmacol. 2009;64:585–591. doi: 10.1007/s00280-008-0909-1. [DOI] [PubMed] [Google Scholar]
- 256.Dellapasqua S., Trillo Aliaga P., Munzone E., Bagnardi V., Pagan E., Montagna E., Cancello G., Ghisini R., Sangalli C., Negri M., et al. Pegylated Liposomal Doxorubicin (Caelyx®) as Adjuvant Treatment in Early-Stage Luminal B-like Breast Cancer: A Feasibility Phase II Trial. Curr. Oncol. 2021;28:433. doi: 10.3390/curroncol28060433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Dou Y., Hynynen K., Allen C. To Heat or Not to Heat: Challenges with Clinical Translation of Thermosensitive Liposomes. J. Control. Release. 2017;249:63–73. doi: 10.1016/j.jconrel.2017.01.025. [DOI] [PubMed] [Google Scholar]
- 258.Besse H.C., Barten-van Rijbroek A.D., van der Wurff-Jacobs K.M.G., Bos C., Moonen C.T.W., Deckers R. Tumor Drug Distribution after Local Drug Delivery by Hyperthermia, In Vivo. Cancers. 2019;11:1512. doi: 10.3390/cancers11101512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Rajappa S., Joshi A., Doval D.C., Batra U., Rajendranath R., Deo A., Biswas G., Bajpai P., Tilak T.V.S., Kane S., et al. Novel Formulations of Docetaxel, Paclitaxel and Doxorubicin in the Management of Metastatic Breast Cancer. Oncol. Lett. 2018;16:3757–3769. doi: 10.3892/ol.2018.9057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Li J., Zhang B., Yue C., Wu J., Zhao L., Sun D., Wang R. Strategies to Release Doxorubicin from Doxorubicin Delivery Vehicles. J. Drug _target. 2018;26:9–26. doi: 10.1080/1061186X.2017.1363209. [DOI] [PubMed] [Google Scholar]
- 261.Birngruber T., Raml R., Gladdines W., Gatschelhofer C., Gander E., Ghosh A., Kroath T., Gaillard P.J., Pieber T.R., Sinner F. Enhanced Doxorubicin Delivery to the Brain Administered through Glutathione PEGylated Liposomal Doxorubicin (2B3-101) as Compared with Generic Caelyx,(®)/Doxil(®)--a Cerebral Open Flow Microperfusion Pilot Study. J. Pharm. Sci. 2014;103:1945–1948. doi: 10.1002/jps.23994. [DOI] [PubMed] [Google Scholar]
- 262.Gaillard P.J., Appeldoorn C.C.M., Dorland R., van Kregten J., Manca F., Vugts D.J., Windhorst B., van Dongen G.A.M.S., de Vries H.E., Maussang D., et al. Pharmacokinetics, Brain Delivery, and Efficacy in Brain Tumor-Bearing Mice of Glutathione Pegylated Liposomal Doxorubicin (2B3-101) PLoS ONE. 2014;9:e82331. doi: 10.1371/journal.pone.0082331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Mehrabian A., Vakili-Ghartavol R., Mashreghi M., Shokooh Saremi S., Badiee A., Arabi L., Alavizadeh S.H., Moosavian S.A., Jaafari M.R. Preparation, Characterization, and Biodistribution of Glutathione PEGylated Nanoliposomal Doxorubicin for Brain Drug Delivery with a Post-Insertion Approach. Iran. J. Basic Med. Sci. 2022;25:302–312. doi: 10.22038/IJBMS.2022.60306.13369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Fraguas-Sánchez A.I., Lozza I., Torres-Suárez A.I. Actively _targeted Nanomedicines in Breast Cancer: From Pre-Clinal Investigation to Clinic. Cancers. 2022;14:1198. doi: 10.3390/cancers14051198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Makwana V., Karanjia J., Haselhorst T., Anoopkumar-Dukie S., Rudrawar S. Liposomal Doxorubicin as _targeted Delivery Platform: Current Trends in Surface Functionalization. Int. J. Pharm. 2021;593:120117. doi: 10.1016/j.ijpharm.2020.120117. [DOI] [PubMed] [Google Scholar]
- 266.Luo R., Li Y., He M., Zhang H., Yuan H., Johnson M., Palmisano M., Zhou S., Sun D. Distinct Biodistribution of Doxorubicin and the Altered Dispositions Mediated by Different Liposomal Formulations. Int. J. Pharm. 2017;519:1–10. doi: 10.1016/j.ijpharm.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 267.Mastria E.M., Cai L.Y., Kan M.J., Li X., Schaal J.L., Fiering S., Gunn M.D., Dewhirst M.W., Nair S.K., Chilkoti A. Nanoparticle Formulation Improves Doxorubicin Efficacy by Enhancing Host Antitumor Immunity. J. Control. Release. 2018;269:364–373. doi: 10.1016/j.jconrel.2017.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Hannesdóttir L., Tymoszuk P., Parajuli N., Wasmer M.-H., Philipp S., Daschil N., Datta S., Koller J.-B., Tripp C.H., Stoitzner P., et al. Lapatinib and Doxorubicin Enhance the Stat1-Dependent Antitumor Immune Response. Eur. J. Immunol. 2013;43:2718–2729. doi: 10.1002/eji.201242505. [DOI] [PubMed] [Google Scholar]
- 269.Eggleton P., Bremer E., Dudek E., Michalak M. Calreticulin, a Therapeutic _target? Expert Opin. Ther. _targets. 2016;20:1137–1147. doi: 10.1517/14728222.2016.1164695. [DOI] [PubMed] [Google Scholar]
- 270.Kawano M., Tanaka K., Itonaga I., Iwasaki T., Miyazaki M., Ikeda S., Tsumura H. Dendritic Cells Combined with Doxorubicin Induces Immunogenic Cell Death and Exhibits Antitumor Effects for Osteosarcoma. Oncol. Lett. 2016;11:2169–2175. doi: 10.3892/ol.2016.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Bell C.W., Jiang W., Reich C.F., Pisetsky D.S. The Extracellular Release of HMGB1 during Apoptotic Cell Death. Am. J. Physiol. Cell Physiol. 2006;291:C1318–C1325. doi: 10.1152/ajpcell.00616.2005. [DOI] [PubMed] [Google Scholar]
- 272.Schiller M., Heyder P., Ziegler S., Niessen A., Claßen L., Lauffer A., Lorenz H.-M. During Apoptosis HMGB1 Is Translocated into Apoptotic Cell-Derived Membranous Vesicles. Autoimmunity. 2013;46:342–346. doi: 10.3109/08916934.2012.750302. [DOI] [PubMed] [Google Scholar]
- 273.Lee J.-J., Park I.H., Rhee W.J., Kim H.S., Shin J.-S. HMGB1 Modulates the Balance between Senescence and Apoptosis in Response to Genotoxic Stress. FASEB J. 2019;33:10942–10953. doi: 10.1096/fj.201900288R. [DOI] [PubMed] [Google Scholar]
- 274.Yang S., Shim M.K., Kim W.J., Choi J., Nam G.-H., Kim J., Kim J., Moon Y., Kim H.Y., Park J., et al. Cancer-Activated Doxorubicin Prodrug Nanoparticles Induce Preferential Immune Response with Minimal Doxorubicin-Related Toxicity. Biomaterials. 2021;272:120791. doi: 10.1016/j.biomaterials.2021.120791. [DOI] [PubMed] [Google Scholar]
- 275.Merino M., Lozano T., Casares N., Lana H., Troconiz I.F., Ten Hagen T.L.M., Kochan G., Berraondo P., Zalba S., Garrido M.J. Dual Activity of PD-L1 _targeted Doxorubicin Immunoliposomes Promoted an Enhanced Efficacy of the Antitumor Immune Response in Melanoma Murine Model. J. Nanobiotechnol. 2021;19:102. doi: 10.1186/s12951-021-00846-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Wang W., Zhang L., Sun Z. Eliciting Pyroptosis to Fuel Cancer Immunotherapy: Mechanisms and Strategies. Cancer Biol. Med. 2022;19:948–964. doi: 10.20892/j.issn.2095-3941.2022.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Zhu L., Lin M. The Synthesis of Nano-Doxorubicin and Its Anticancer Effect. Anti-Cancer Agents Med. Chem. 2021;21:2466–2477. doi: 10.2174/1871520621666201229115612. [DOI] [PubMed] [Google Scholar]
- 278.Ibrahim M., Abuwatfa W.H., Awad N.S., Sabouni R., Husseini G.A. Encapsulation, Release, and Cytotoxicity of Doxorubicin Loaded in Liposomes, Micelles, and Metal-Organic Frameworks: A Review. Pharmaceutics. 2022;14:254. doi: 10.3390/pharmaceutics14020254. [DOI] [PMC free article] [PubMed] [Google Scholar]