Abstract
Sugar-sweetened beverage (SSB) consumption is disproportionately high among rural Appalachian adults, with intakes double the national average and nearly four times the recommended amount. This trial _targets this major dietary risk factor and addresses notable gaps in the rural digital health intervention literature. iSIPsmarter is a technology-based behavior and health literacy intervention aimed at improving SSB behaviors. It is comprised of six Internet-delivered, interactive Cores delivered weekly, an integrated short message service (SMS) strategy to engage users in tracking and reporting SSB behaviors, and a cellular-enabled scale for in-home weighing. iSIPsmarter is adapted from an evidence-based intervention and is grounded by the Theory of Planned Behavior and health literacy, numeracy, and media literacy concepts. The RCT is guided by the RE-AIM framework and _targets 244 rural Appalachian adults. The goal is to examine the efficacy of iSIPsmarter to reduce SSB in a two-group design [iSIPsmarter vs. static Participant Education website] with four assessment points. Changes in secondary outcomes (e.g., diet quality, weight, quality of life) and maintenance of outcomes will also be evaluated. Additional secondary aims are to examine reach and representativeness, patterns of user engagement, and cost. Two tertiary aims are exploratory mediation analyses and a systems-level, participatory evaluation to understand context for future organizational-level adoption of iSIPsmarter. The long-term goal is to sustain an effective, scalable, and high reach behavioral intervention to reduce SSB-related health inequities and related chronic conditions (i.e., obesity, diabetes, some obesity-related cancers, heart disease, hypertension, dental decay) in rural Appalachia and beyond.
Keywords: Beverages, Behavioral research, Digital technology, Randomized controlled trial, Health literacy, Rural population
1. Introduction
In the United States, sugar-sweetened beverages (SSB, e.g., soda/pop, sweet tea, sports and energy drinks, fruit drinks, sweetened coffee) are the largest single food source of calories, contributing approximately 7% of total energy intake for adults.1 There are strong and consistent data documenting relationships among high SSB consumption and numerous health issues, including obesity, diabetes, some obesity-related cancers, heart disease, hypertension, and dental decay.2–12 The intake of SSB is disproportionately high in the southwest Virginia region of Appalachia. Specifically, adults drink ~38 ounces (~475 calories) of SSB per day13 that contributes to about 14% of total daily energy intake.14,15 This intake is more than double national average intakes1 and more than four times the recommended amount of 8 ounces or less per day.16,17
Further compounding the challenges of SSB, the Appalachian region lacks access to medical services and evidence-based behavioral prevention programs.18–20 Historically, extending evidence-based interventions into Appalachia has been hindered by lack of providers, geographical dispersion and limited transportation resources, and a digital divide.18,21 In recent years, progress has been made in shrinking the digital divide.22–25 Rural adults are becoming increasingly connected through mobile phones with short message service (SMS) capability; nationally, mobile phone ownership is 91% in rural areas23 with dramatic increases in smartphone ownership.22 Similar adoption rates are found in Appalachia Virginia. Estimates indicate that approximately 85% of southwest Virginians have access to Internet and 99.9% of Virginians have mobile coverage.24,25 This digital expansion offers an opportunity to address challenges that have remained relatively static in Appalachia, including provider shortages and transportation barriers.
Although there is a large body of literature documenting the effectiveness of health-related Internet-based interventions, including for nutrition-related outcomes,26–32 there is limited data on Internet-based interventions in medically-underserved rural regions, especially in Appalachia. Because of this gap, there is a great need to understand how rural, Appalachian adults may engage with technology-based behavioral programs.
Previous research findings document the effectiveness of SIPsmartER, a behavioral and health literacy intervention, at improving SSB behaviors in rural, Appalachian adults.33,34 Furthermore, SIPsmartER significantly decreased weight,33 as well as improved overall dietary and beverage quality,15,35 delta13C biomarker (i.e., a biomarker of added sugar),36 and quality of life (QOL).33 A meta-analysis of 12 controlled interventions _targeting SSB intake among adults found that SIPsmartER demonstrated the largest effects and significantly improved SSB behaviors relative to the matched contact control condition focused on physical activity (−413.98 mL SSB, 95% CI −665.32, −162.64).37 Despite promising effects, in a follow-up pilot dissemination and implementation trial of SIPsmartER, the small group class modality limited the reach and scalability of this effective intervention.38
The current iSIPsmarter trial was conceptualized to address the need for scalable and effective SSB reduction strategies that can reach large numbers of low SES, rural residents with the highest SSB consumption rates. This study builds on prior SSB trials in rural Appalachia and is adapted from an evidence-based SSB reduction program for adults.
2. Materials and methods
2.1. Study overview and objectives
iSIPsmarter is a randomized-controlled trial (RCT) guided by the RE-AIM (reach, efficacy/effectiveness, adoption, implementation, maintenance) planning and evaluation framework.39,40 The primary objective is to examine the efficacy of an Internet-based intervention aimed at decreasing SSB consumption (iSIPsmarter) in a two-group [iSIPsmarter vs. static Participant Education (PE) website] design with four assessment time points including baseline (pre-intervention), week 9 (post-intervention), 6-months post-intervention, and 18-months post-intervention. The primary hypothesis is that iSIPsmarter will be more efficacious at reducing SSB consumption than a PE website at the week 9 post-intervention. Secondary objectives are to determine efficacy on secondary outcomes (e.g., diet quality, weight, QOL, behavioral theory constructs) and maintenance of outcomes at 6- and 18-months post intervention. Additional secondary aims include evaluating reach and representativeness of enrolled participants and describing patterns of user engagement. Exploratory aims are to explore the influence of engagement on efficacy outcomes and explore mediators to engagement and efficacy outcomes. Finally, to inform future organizational-level adoption and implementation, costs will be estimated and factors that influence sustainable SSB screening and referral processes among rural, Appalachian systems will be explored.
2.2. Study region and population
This study _targets adults living in and around the rural southwest Virginia region of Appalachia. In this region, about 94% of adults are white, 56% have beyond a high school education, the median income is around $40,200, and the poverty rate is approximately 19%.18 The region is disproportionately burdened by health disparities and has among the poorest scores for health behaviors in the state,41 with the majority of the region scoring low in terms of health opportunity level.42 The Appalachian region has high prevalence and mortality from numerous SSB-related chronic conditions (i.e., obesity, diabetes, some obesity-related cancers, heart disease, hypertension, dental decay) and limited access to medical care.18,43 This disproportionate burden is compounded by compromised determinants of health: high poverty rates,44 low educational attainment,45 and low health literacy.46
2.3. Intervention development and adaptation
The iSIPsmarter intervention was adapted from the effective SIPsmartER intervention focused on SSB behaviors.33 Both interventions _target rural Appalachian adults. SIPsmartER is a 6-month intervention with three in-person group classes and 11 interactive voice response (IVR) calls. It also includes a 12-month maintenance phase with monthly IVR calls. Alternatively, iSIPsmarter is a 9-week intervention with six Internet-based Cores and a recurring maintenance Core lasting 18-months post intervention. SSB self-monitoring, action planning, and feedback are key features of both programs.
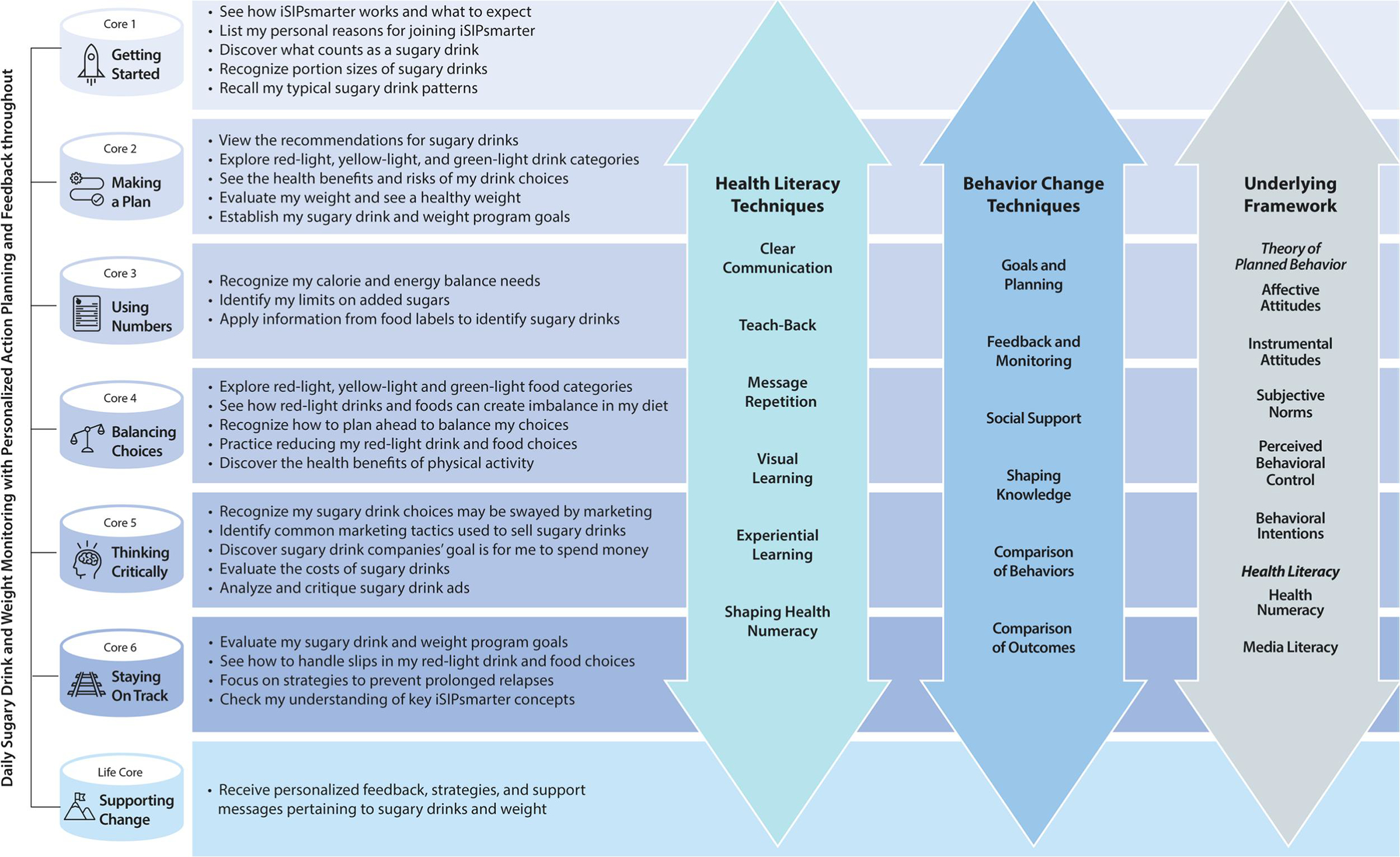
Like SIPsmartER, iSIPsmarter is also grounded by the Theory of Planned Behavior (TPB) and health literacy, numeracy and media literacy concepts (Figure 1). The TPB is one of the most well-studied and useful theories for understanding and improving health behaviors. This theory postulates that an individual’s behavioral intentions are shaped by attitudes, subjective norms, and perceived behavioral control.47,48 iSIPsmarter integrates skill-based health literacy concepts, such as numeracy and media literacy. This focus on health literacy is important because low SES and rural residents are more likely to have low health literacy. Further, low health literacy has consistently been linked with adverse health outcomes, and low numeracy has been shown to influence chronic disease management and correlate with nutrition- and weight-related outcomes.49–55 iSIPsmarter integrates health numeracy skills to help participants use and apply SSB nutrition facts label information. Media literacy skills are _targeted to mitigate the overexposure and negative influence of SSB marketing, to foster skepticism toward advertising, and to develop critical thinking skills needed to identify misclaims in SSB advertising.56–61
Figure 1.
iSIPsmarter Overview
The core content of SIPsmartER and iSIPsmarter are remarkably similarly. The main exception is the addition of evidence-based weight related strategies that were incorporated into iSIPsmarter during the adaptation process. Specifically, behavioral content related to the specific role of SSB in energy balance, weight self-monitoring as an additional self-regulation strategy, and personalized action planning and feedback pertaining to weight were added.
A user-centered development process was employed to adapt SIPsmartER to iSIPsmarter. An iSIPsmarter Advisory Team was established at the outset to engage individuals who represent the user population and get their feedback during the adaptation process. Researchers conducted field study and usability interview sessions to inform development efforts. Twelve 1-hour telephone calls were conducted with seven Advisory Team members. Sessions were focused on three main areas: 1) accessibility (e.g., Internet access, device and mobile phone ownership, computer literacy, SMS use), 2) Core content, and 3) usability and functionality. From the Advisory Team calls, improvements to the iSIPsmarter dashboard were made in order to increase usability and functionality for participants. Further, Advisory Team members provided important feedback on stories (modeled from past SIPsmartER participants) that are woven throughout the Cores. Members identified stories that were relevant and described situations related to setting SSB goals, making behavioral changes, and overcoming barriers to drinking less SSB. Feedback from Advisory Team members was integral in developing relevant, culturally-sensitive Core content. Likewise, member feedback helped inform the development of iSIPsmarter technology components, including built-in flexibility to account for varying Internet and SMS accessibility among participants.
2.4. Study design
2.4.1. Design and randomization
This RCT includes a two-group by four assessment design. After the baseline assessment, a simple randomization process with a 1:1 allocation ratio is used to assign participants to the iSIPsmarter or PE conditions. Participants will be emailed a unique link to set their password in order to log on and securely access their assigned program.
All study procedures have been approved by the University of Virginia Institutional Review Board. Prior to enrollment, participants will be made aware of the random allocation process to iSIPsmarter or PE groups and provide their informed consent to participate in the study. To compensate their time to complete the data assessments, online gift cards in the amount of $50, $50, and $100 will be provided at the week 9, 6-month, and 18-month post-intervention assessments, respectively. Additionally, participants will be mailed an electronic cellular-enabled scale (valued at $110) for data collection which is theirs to keep.
2.4.2. Eligibility criteria
Study eligibility criteria includes English-speaking adults 18 years of age and older, who live in Southwest Virginia or surrounding Appalachian counties. Eligible adults must consume >200 SSB calories per day, as assessed by a validated beverage intake questionnaire.62–64 Additional eligibility criteria include the ability and willingness to access an Internet-enabled computer or tablet at least one time per week to check and receive email and willingness to receive SMS-based stepped care reminders.
2.4.3. Recruitment
This study will recruit, enroll, and randomize 244 participants. An iSIPsmarter Leadership Council was formed to engage stakeholders in proactively addressing recruitment and sustainability planning. The Leadership Council is comprised of four organizations that service Southwest Virginia, including two Federally-Qualified Health Center networks, the Virginia Department of Health, and a multi-service community agency.
Recruitment strategies will include a variety of different approaches within each partnering organization and across the broader Southwest Virginia. Examples include distribution of study brochures, provider referrals, and flyers with information directing individuals to an interest website. A participant interest website will include information on the study, eligibility, incentives, privacy, and how to join. Adults who are interested in the study will complete a brief online interest screener which will be available on the study website. The screener is used to determine initial eligibility in the study.
2.5. Interventions Overview
iSIPsmarter and the PE websites both include the provision of scientifically accurate and evidence-based SSB behavioral content as well as the ability to track SSB and weight diaries. All content within iSIPsmarter and the PE website is written using clear communication strategies and at or below an 8th grade reading level. The digital interventions are built on a proprietary Research Infrastructure Containing ehealth (RICE) platform and the website structure is modeled off an evidenced-based behavioral intervention for adults with insomnia.65,66
2.5.1. Participant Education (PE) website
The PE website control condition includes relevant content from the iSIPsmarter intervention. The website provides users with self-guided information that is presented all at once, allowing the user to complete the website at their own pace. The PE website is organized by pages and includes information about SSB recommendations, types of SSB and portion size, SSB-related health risks, energy balance information, identifying motivators and barriers to reducing SSB intake, interpreting SSB nutrition labels, and recognizing media influences and misclaims about SSB advertisements. Printable forms are available in order to assist participants in tracking their SSB and weight; however, this data is not entered or stored on the website. Also, PE participants do not set SSB or weight goals or have personalized feedback.
2.5.2. iSIPsmarter
iSIPsmarter is a highly interactive, structured, and self-guided program. It is comprised of six Internet-based Cores and a recurring maintenance Core, personalized action planning, and behavioral tracking. The Cores include an interactive and media rich format of text, audio, graphics, animation, and video. The Cores utilize stories and testimonials modeled from past SIPsmartER participants in the region to make the content more relevant. Each of the six Cores are be metered out to the user, with a new Core unlocked and available seven days after completion of the previous Core. Anticipated time to complete the program is less than one hour each week. Because iSIPsmarter Cores are delivered online, users have convenient access to the program from anywhere the Internet is available. And, while it is not a native mobile application, it is usable through a smartphone browser, making it functional on a mobile device. Automated email reminders alert users when new Cores are available in order to promote Core completion. Users receive up to two automated email reminders to complete the Cores.
As shown in Figure 1, iSIPsmarter integrates numerous skill-building and evidence-based strategies across the Cores: behavior change techniques (e.g., goal setting, action planning, feedback and monitoring, comparison of outcomes)67 and health literacy techniques (e.g., clear communication, message repetition, visual learning, experiential learning, building health numeracy skills, media message critiques).57,68–71 As guided by the TPB, iSIPsmarter _targets participants’ SSB-related attitudes, subjective norms, and perceived behavioral control to improve behavioral intentions and SSB behaviors. A few TPB application examples include: 1) attitudes - participants examine the health and financial implication of their SSB behaviors, 2) subjective norms - participants consider the influence of family and friends on their SSB behaviors, 3) perceived behavioral control - participants are encouraged to work on two self-selected SSB barriers per week and to achieve small weekly goals (i.e., decrease SSB by 20–50% per week), and 4) behavioral intentions - participants set week goals and develop a personalized action plan.
Each iSIPsmarter Core includes behavioral content, personalized action planning pertaining to both SSB behaviors and weight, and personalized follow-up and feedback. Participants complete personalized action planning throughout iSIPsmarter, starting with Core 2. Action planning is specifically designed to provide behavioral support to users and help troubleshoot behavioral barriers. All participants are encouraged to work towards the recommendation of drinking less than 8 ounces of SSB per day. However, participants set their own program and weekly SSB goals based on their current SSB intake. While participants are encouraged to set a weekly goal of a 20–50% SSB ounce decrease from their previous week’s average (until they meet recommendations), they are allowed to choose a goal outside of the recommended range. Participants have the option of setting personal goals to ‘maintain weight’ or ‘lose weight’, and Core content (e.g., personalized recommendations for calories and added sugar) is customized to their goals.
SSB tracking is a key component of iSIPsmarter. The program will provide daily prompts for users to report SSB intake (in ounces) from the previous day. Participants have the option of receiving daily prompts by email only or by both email and SMS; participants do not have to opt into daily SMS prompts for tracking. The email directs participants to enter their ounces by logging into the website. The SMS prompts users to respond with their number of SSB ounces and an encouraging and/or confirmation SMS will be sent back. When users log into the website, personalized SSB feedback will be provided. Further, users are provided a cellular enabled ©BodyTrace scale along with encouragement via e-mail, SMS, and Dashboard content to weigh daily to track progress towards weight loss or maintenance goals. Weigh-ins from the ©BodyTrace scale are synced with iSIPsmarter. For participants who are unable to sync their scales, they may also log into the website and enter their weight on the Dashboard. Similar to SSB, personalized weight feedback is provided when users log into the website.
2.5.2.1. iSIPsmarter stepped care engagement strategy
Engagement and retention issues are prevalent in technology-based interventions,72–75 including those pertaining to lifestyle habits and weight.30 Therefore, iSIPsmarter uses a human-supported stepped care engagement strategy to provide support and encouragement to complete each of the six Cores. The timing of the delivery of stepped care coincides with the Core timing and participants will be identified as either adherent or non-adherent in completing their assigned Core. When participants complete their assigned Core, no additional support will be provided, and the participant will continue to the next Core. When participants fail to complete a Core, they will receive a human-supported text. The text message includes: 1) content stating that the user did not complete the Core; 2) encouragement to log back in and complete the Core as soon as possible; and 3) support by asking if there were any concerns or obstacles to completing the assigned task for that week. If participants have not completed the Core by the following week, they will be stepped-up to receive a phone call. Research staff will call the participant to provide encouragement, technical assistance, and strategies to promote task completion. When possible, reasons for non-adherence will be documented. If the participant still does not complete the Core, they will be considered non-adherent. To encourage reengagement, non-adherent participants will continue to weekly receive automated email reminders to complete Cores and daily prompt reminders to track.
2.5.3. Interventions Summary
Although there is overlap between groups, iSIPsmarter is a multi-component intervention that differs from standard PE websites in the following ways: 1) individually tailored SSB and weight recommendations based on user input; 2) high levels of interactivity to increase user engagement; 3) structured implementation of the program through use of metered (distributed) content over the intervention period rather than content presented all at once; and 4) provision of comprehensive user-specific content rather than more general information. Also, participants randomized to the iSIPsmarter condition will complete behavioral tracking using SMS and online tools whereas the PE website provides printable forms. Finally, both interventions are fully digital, with the exception of iSIPsmarter human-supported stepped care engagement strategies to promote Core completion. The PE website was chosen as the control condition to provide evidence-based SSB behavioral content and some potential benefit to all eligible Appalachian adults who join the trial, while also maximizing web program differentiation to appropriately test our hypotheses.
2.6. Data collection and measures
Data collection to assess efficacy of the intervention will be managed by research team members. An overview of the measures used at each of the four time points are illustrated in Table 1.
Table 1.
Outcome measures for each aim and the assessment timing schedule
| Measures | Pre | Post | 6 M | 18 M | Aim | Description |
|---|---|---|---|---|---|---|
| Eligibility Screener | X | SA2 | SSB screener, demographics, subjective health literacy,76–78 and access to and use of Internet and text messaging | |||
| Beverage Intake, BEV-Q 15 | X | X | X | X | PA, SA1 | Frequency and portion sizes of 15 beverage categories over the past month, including 5 SSB specific categories (e.g., regular soft drinks, sweetened juice drinks, tea with sugar, coffee with sugar, energy drinks)62–64 |
| 24-hour Dietary Recalls | X | X | X | X | SA1 | Two unannounced 24-hour dietary recalls (one weekend and one weekday) using state-of-the-art Nutrition Data System for Research (NDSR) software and multiple pass methods79 |
| Weight | X | X | X | X | SA1 | Assessed via study provided cellular/WIFI enabled in-home digital scale |
| Height | X | SA1 | Self-reported | |||
| QOL | X | X | X | X | SA1 | Assessed using 4-item Centers for Disease Control Healthy Days core questions80 |
| SSB TPB | X | X | X | X | SA1 | SSB-related TPB with 4 subscales: attitudes, subjective norms, perceived behavioral control, and behavioral intentions13 |
| SSB Media Literacy | X | X | X | X | SA1 | Perceptions of SSB-related media and advertisements with 3 subscales: authors and audience, messages and meanings, and representation and reality81 |
| Health Literacy | X | X | X | X | SA1 | Assessed using the Newest Vital Sign, an objective health literacy & numeracy, based off 6 questions from nutrition facts panel82 |
| eHealth Literacy | X | X | X | X | Assessed using the eHealth Literacy Scale (eHEALS)83 | |
| SSB Home Environment | X | X | X | X | SA1 | Home availability frequency of 15 beverage categories from the BEVQ-15 (modeled from home food availability measures)84–86 |
| Other Health Habits | X | X | X | X | SA1 | Weighing frequency, weight perceptions,87 and weight and SSB avoidance adapted from the Information Avoidance Scale88,89; Physical activity using Stanford Leisure-Time Activity Categorical Item (L-Cat)90–92; Sleep quality using the Pittsburgh Sleep Quality Index (PSQI)93; Tobacco history87 |
| Health History, Medication, & Health care access | X | X | X | X | SA1 | History of chronic disease and medication use; Health access to care variables such as: health insurance, unmet health needs, usual source health care, routine check-up, delayed or missed care due to cost87 |
Pre = baseline (pre-intervention); Post = week 9 (post-intervention); 6 M = 6-months post-intervention; 18 M = 18-months post-intervention
PA = Primary Aim; SA = Secondary Aim; QOL = quality of life; SSB = sugar-sweetened beverages; TPB = Theory of Planned Behavior
2.6.1. Efficacy and maintenance measures
Before enrollment, the online interest screener will collect information on potential participant demographics and SSB intake. Two 24-hour telephone dietary recalls and an online questionnaire are administered at baseline. At the initial telephone call, participants who consent to join the study are asked to complete their first telephone 24-hour dietary recall. After the first recall, participants will be emailed a link to complete the online baseline survey and mailed a cellular-enabled ©BodyTrace scale with instructions. After the baseline survey is complete, research staff will call participants for a second dietary recall and then participants will be randomized into the iSIPsmarter or PE conditions. Participants will be emailed a unique link to set their password in order to log on and securely access their assigned program.
The 9 week post-intervention assessment time point allows participants a reasonable amount of time to complete all six Cores. At the start of week 9, regardless of intervention progress or intervention group, participants will be instructed to complete the online post-assessment battery, weigh-in, and two 24-hour dietary recalls. After completing the assessments, individuals will have continued access to their assigned online program. The same assessment procedures will be followed again at the 6- and 12-months post-intervention maintenance assessments.
2.6.2. Reach and engagement measures
Participation reach will be determined by dividing the total number of enrolled participants by the total number eligible to enroll. The process engagement variables are automatically collected and stored in the database (e.g., number of logins, time/date of use, average session length, content viewed, completion and mode of SSB and weight tracking). The Internet Intervention Evaluation Measure94,95 and Internet Intervention Adherence Measure94,96 will be adapted and administered at week 9 post assessment to examine users’ experiences with and perceived efficacy of the programs.
2.6.3. Adoption and implementation measures
Process data include meeting minute notes from the Leadership Council and process notes on recruitment strategies. Leadership Council members will be interviewed at the conclusion of active recruitment in order to identify strategies for sustainability and improve recruitment and enrollment protocols. To determine costs, research staff use a real-time tracking process to document time spent for the stepped care components, including texts and phone calls.97
2.6.4. Power calculation
The iSIPsmarter power calculation is based on the existing SIPsmartER effectiveness trial that found an effect size of 0.55 for the primary 6-month SSB reduction. It is expected that iSIPsmarter will also lead to significant improvements given the added enhancements of stepped care, daily SSB tracking, and the shorter time to follow-up assessment. However, given the remote delivery, more limited human exchange, and less discrepancy of provision of content provided between the experimental and control conditions (PE website provides SSB content), a smaller iSIPsmarter ES may be found. Based on these considerations, the current study is powered to detect a reasonably conservative effect size of 0.4. To achieve 80% power with a 0.05 type I error rate, 97 participants/condition are needed. Accounting for 20% attrition at the post intervention assessment, a total of 122 participants/condition will be enrolled (Total enrolled = 244).
2.7. Data analysis
The efficacy analysis will be on the individual level and will address potential self-selection occurrence across program participation, engagement, and stepped care provision. Descriptive, parametric, and non-parametric statistical methods will be used to summarize continuous and categorical variables between the intervention conditions at baseline. Data will be examined for the presence of outliers, violations of normality (for continuous variables), and missing data. Major violations of normality will be corrected with an appropriate transformation procedure. All analyses will use county-level, cluster-robust standard error adjustment to account for correlation of behavioral outcomes within the county who are likely to share similar food and beverage preferences, food environments, and SSB consumption norms.
2.7.1. Efficacy and maintenance
A general linear mixed model (GLMM) will be used to control errors of non-independence and heteroscedasticity caused by individual and county heterogeneity, and potential covariates identified a priori based on the existing literature and theory that are relevant to SSB consumption outcome, and include: age, gender, race/ethnicity, income level, education level, health literacy level.98–101 We will also model attrition specifically in GLMM and estimate it through full-information maximum likelihood as one approach for conducting intention-to-treat analysis.
2.7.2. Reach and engagement
The multi-level mixed effect model used for the primary aim will be modified to assess secondary outcomes and maintenance time points. For those discrete outcomes, nonlinear mixed effect models will be used with appropriate link functions chosen to capture the nonlinear outcomes’ distribution; additional time indicators will be added to the model that will capture 6- and 18-months follow-up assessment time points. Due to the multiple outcomes treatment effect analysis, we will follow the multiple testing correction procedures in mixed models proposed in Joo et al.102 and examine the potential efficiency gained through hierarchical Bayesian procedure in Gelman et al.103
Reach will be analyzed following recommendations of Glasgow et al.104 Participation rate will be determined by dividing the total number of enrolled participants by the total number of eligible inquiries. Representativeness will be assessed by comparing demographics of those enrolled to: 1) those screened, eligible, and not enrolled, and 2) the demographics of the _targeted Appalachia Virginia region using county-level Census Bureau data.105 We will report descriptive statistics and qualitative findings on patterns of user engagement (e.g., number of log-ins, number of Cores completed, diary entries), requirement for stepped care, and participants’ perceptions of the intervention (e.g., usability, satisfaction, and barriers to web program use).
To explore how engagement influences efficacy outcomes, the GLMM will be expanded to include engagement variables (e.g., number of log-ins/Core completion). Furthermore, the GLMM will be modified to explore potential mediating effects of variables (e.g., behavioral theory constructs) on engagement and efficacy outcomes. The procedure for testing mediation will closely follow suggestions of Zhao et al.106 and Imai et al.107 Although not specifically powered for these exploratory mediation analyses, findings will provide necessary preliminary results to inform a future effectiveness trial in terms of block randomization, potential stratification, and _targeted power calculation.
2.7.3. Adoption and implementation
Data sources will include meeting artifacts (e.g., agendas, minutes, memos) and key informant interview transcripts. Aided by NVivo software, a hybrid deductive (i.e., utilizing RE-AIM39,40 and Consolidated Framework for Implementation Research108 constructs as coding categories) and inductive (i.e., identifying specific emergent codes within each category) qualitative analysis approach will be used.109–112 Coding will occur in pairs, and 80% agreement will be sought. In an iterative process, meaning units will be reduced into emerging themes then organized back to the guiding frameworks. To facilitate a deeper understanding of our processes, organizational-level data will be triangulated to check for consistency between and within sources.111,113 When feasible, efforts will be made to draw out distinctions by organizational site.
Implementation costs will be assessed as the incremental cost of delivering iSIPsmarter with stepped care relative to the PE website. Since the primary cost additions are due to the added stepped care component of iSIPsmarter, we will focus on those associated added costs, including time to construct and send texts and time to prepare for and talk on the phone.97 Beyond those incremental costs, we will also capture costs per participant and explore marginal costs per SSB kcal reduction. Non-research-related intervention resource use will be valued at competitive market rates (e.g., the labor costs of stepped care will be valued at the market wage rate for the associated occupation). All costs will be estimated and evaluated in the constant dollars adjusted by appropriate index. Recognizing that we do not have a second treatment group without stepped care enhancement, we will use Monte Carlo simulations to alter adherence rate and changes in characteristics of the participants in order to simulate changes in stepped care demands.114 This will provide necessary parameters for a future full-scale effectiveness trial that assess cost-effectiveness of iSIPsmarter in rural systems.
3. Discussion
Despite the pervasive SSB problem in Appalachia and nationally, as well as clear obesity and health consequences, solutions surrounding excessive consumption of SSB intake remain a critical public health challenge. While emerging evidence from enacted policy-level SSB taxation strategies are promising,115–117 SSB taxation also remains highly debated and resisted.118–121 Likewise, culturally engrained SSB behaviors will not be solved solely from a top-down, macro-level approach. Our RCT is the first known study to test the efficacy and reach of a behavioral and technology-based SSB reduction intervention in rural communities, while also seeking to understand the context for potential future organizational-level adoption and implementation.
Importantly, our study builds on an existing evidence-based intervention and utilizes an individual-level behavioral, health literacy, and technology-based approach. In distinction from the other SSB studies that have been found ineffective among adults,37 we attribute SIPsmartER’s effectiveness to the underlying conceptual and theoretical approach, use of evidence-based behavioral change techniques, as well as our _targeted strategy focused exclusively on SSB. Each of these attributes have been carried forward in the adaption process and user-centered development of iSIPsmarter. Despite strong intervention evidence in both the health literacy and behavioral medicine fields, there remains a dearth of lifestyle interventions guided, implemented, and evaluated within both behavioral change theory and a health literacy framework49,50,54,55,122 (e.g., only 3 of 74 recently reviewed community-based health literacy studies used behavior change theory).122 iSIPsmarter’s comprehensive integration of evidence from both disciplines, including behavioral change and skill-build techniques, is a unique approach.
The shrinking digital divide among rural communities presents an opportunity for the use of technology-based interventions in rural areas, as a means to overcome barriers (e.g., transportation, small population sizes) that have limited evidence-based lifestyle interventions in rural areas. However, to fully capitalize on this opportunity, it is important to explore how rural residents engage with the technology. The integrated SMS tracking of daily SSB behaviors and remote weight tracking are additional innovative iSIPsmarter components designed to further augment real-time personalization of Internet-based Cores. There is a clear lack of data in the literature on these components in rural regions, especially in Appalachia. Furthermore, engagement and retention issues are prevalent in technology-based interventions.30,72–75 However, the literature on engagement in digital behavior change interventions is complex and lacks clear and consistent solutions.72–75 Our stepped care strategies will provide important data on promoting engagement in technology-based behavioral interventions, in rural and lower SES regions.
4. Limitations
Several limitations of this study should be noted. First, the _targeted rural Appalachia region and exclusion of non-English speakers may limit the generalizability of findings. Second, given this study is an Internet-based intervention, the inclusion criterion limits the sample to those with access to technology. Third, the primary outcome is self-report SSB, which may suffer from reporting errors. However, our findings are based on comparative efficacy (i.e., comparing iSIPsmarter and PE). Therefore, as long as the reporting errors are randomly distributed across the two groups, the comparative efficacy findings will not be subject to this limitation. Despite these limitations, our RCT _targets a high-need rural Appalachia region with documented excessive SSB intake, is adapted from an evidence-based intervention, applies innovative technology and a stepped care approach to optimize participant engagement, uses state-of-the art dietary assessment approaches to evaluate outcomes, and is being implemented with guidance from four local health and community-based service organizations to identify sustainable recruitment and implement strategies.
5. Conclusions
Clearly missing from the literature are scalable and effective SSB reduction strategies that can reach large numbers of low SES, rural residents with the highest consumption rates. Moreover, the prevention and treatment of chronic diseases are typically most successful when paired with other multi-level strategies and systems-oriented approches.123,124 If iSIPsmarter is found to be efficacious, and reach and engagement shows strong potential, a future goal will be to integrate this intervention within healthcare systems and with higher macro-level approaches (e.g., policies to limit access, taxation). Given the magnitude of excessive SSB consumption and consequences, this future work would be applicable in rural Appalachia and beyond.
6. Funding sources
This study was funded by the National Institutes of Health (NIH), National Institute on Minority Health and Health Disparities [R01MD015033]. NIH was not involved in the design of this study or writing of this manuscript.
Abbreviations:
- SSB
sugar-sweetened beverages
- SMS
short service message
- RE-AIM
reach, adoption, effectiveness, implementation, and maintenance
- TPB
Theory of Planned Behavior
- RCT
randomized controlled trial
- PE
participant education
- GLMM
general linear mixed model
Footnotes
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Dr. Deborah Tate serves on the scientific advisory board for Weight Watchers and WondrHealth.
Yet, all other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ClinicalTrial registry: NCT05030753
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kit BK, Fakhouri THI, Park S, Nielsen SJ, Ogden CL. Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999–2010. Am J Clin Nutr. 2013. May 13;98(1):180–188. doi: 10.3945/ajcn.112.057943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bes-Rastrollo M, Schulze MB, Ruiz-Canela M, Martinez-Gonzalez MA. Financial conflicts of interest and reporting bias regarding the association between sugar-sweetened beverages and weight gain: a systematic review of systematic reviews. PLoS Curr. 2013. December 31;10(12). doi: 10.1371/journal.pmed.1001578.s003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am J Clin Nutr.. 2013. August 21;98(4):1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Imamura F, O’Connor L, Ye Z, et al. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ Open Sport Exerc Med. 2015. July 21;351:h3576. doi: 10.1136/bmj.h3576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang M, Yu M, Fang L, Hu RY. Association between sugar-sweetened beverages and type 2 diabetes: a meta-analysis. J Diabetes Ivestig. 2015. May;6(3):360–366. doi: 10.1111/jdi.12309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makarem N, Bandera EV, Nicholson JM, Parekh N. Consumption of sugars, sugary foods, and sugary beverages in relation to cancer risk: a systematic review of longitudinal studies. Annu Rev Nutr. 2018. August 21;38(1):17–39. doi: 10.1158/1940-6207 [DOI] [PubMed] [Google Scholar]
- 7.Makarem N, Bandera EV, Lin Y, Jacques PF, Hayes RB, Parekh N. Consumption of sugars, sugary foods, and sugary beverages in relation to adiposity-related cancer risk in the framingham offspring cohort (1991–2013). Cancer Prev Res. 2018. June;11(6):347–358. doi: 10.1158/1940-6207.CAPR-17-0218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta-analysis of prospective studies. Atherosclerosis. 2014. May 1;234(1):11–16. doi: 10.1016/j.atherosclerosis.2014.01.037 [DOI] [PubMed] [Google Scholar]
- 9.Malik AH, Akram Y, Shetty S, Malik SS, Njike VY. Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol. 2014. May 1;113(9):1574–1580. doi: 10.1016/j.amjcard.2014.01.437 [DOI] [PubMed] [Google Scholar]
- 10.Xi B, Huang Y, Reilly KH, et al. Sugar-sweetened beverages and risk of hypertension and CVD: a dose-response meta-analysis. Br J Nutr. 2015. March 14;113(5):709–717. doi: 10.1017/S0007114514004383 [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Park S, Lin M. Permanent tooth loss and sugar-sweetened beverage intake in U.S. young adults. J Public Health Dent. 2017. March;77(2):148–154. doi: 10.1111/jphd.12192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bernabe E, Vehkalahti MM, Sheiham A, Aromaa A, Suominen AL. Sugar-sweetened beverages and dental caries in adults: a 4-year prospective study. J Dent. 2014. May 9;42(8):952–958. doi: 10.1016/j.jdent.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 13.Zoellner J, Estabrooks P, Davy B, Chen Y, You W. Exploring the theory of planned behavior to explain sugar-sweetened beverage consumption. J Nutr Ed Behav. 2012. Mar-Apr;44(2):172–177. doi: 10.1016/j.jneb.2011.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuhas M, Zoellner J, Hedrick V. Consumption of added sugars by rural residents of Southwest Virginia. J Appalach Health. 2020; 2(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hedrick VE, Davy BM, You W, Porter KJ, Estabrooks PA, Zoellner JM. Dietary quality changes in response to a sugar-sweetened beverage–reduction intervention: results from the talking health randomized controlled clinical trial. Am J Clin Nutr. 2017. March 1;105(4):824–833. doi: 10.3945/ajcn.116.144543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popkin BM, Armstrong LE, Bray GM, Caballero B, Frei B, Willett WC. A new proposed guidance system for beverage consumption in the United States. Am J Clin Nutr. 2006. March;83(3):529–542. doi: 10.1093/ajcn.83.3.529 [DOI] [PubMed] [Google Scholar]
- 17.Johnson RK, Appel LJ, Brands M, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circ AHA. 2009. August 24;120(11):1011–1020. doi: 10.1161/circulationaha.109.192627 [DOI] [PubMed] [Google Scholar]
- 18.Marshall J, Thomas L, Lane N, et al. Health disparities in Appalachia. Appalachian Regional Commission Website. https://www.arc.gov/report/health-disparities-in-appalachia/. Published August 23, 2017. Accessed April 16, 2019. 2017. [Google Scholar]
- 19.Halverson JA, Friedell GH, Cantrell SE, Behringer BA. Health Care Systems. In: Ludke RL, Obermiller PJ, eds. Appalachian Health and Well-Being. Lexington, KY: University Press of Kentucky; 2012. [Google Scholar]
- 20.McGarvey EL, Leon-Verdin M, Killos LF, Guterbock T, Cohn WF. Health disparities between Appalachian and non-Appalachian counties in Virginia USA. J Community Health. 2011. June;36(3):348–356. doi: 10.1007/s10900-010-9315-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Behringer B, Friedell GH. Appalachia: where place matters in health. Prev Chronic Dis. 2006. October;3(4): Centers for Disease Control and Prevention Website. http://www.cdc.gov/pcd/issues/2006/oct/06_0067.htm. Accessed April 29, 2019. [PMC free article] [PubMed] [Google Scholar]
- 22.Perrin A A digital gap between rural and nonrural America persists. Pew Research Center Website. https://www.pewresearch.org/fact-tank/2019/05/31/digital-gap-between-rural-and-nonrural-america-persists/. Accessed April 29, 2019. [Google Scholar]
- 23.Middleton G, Henderson H, Evans D. Implementing a community-based obesity prevention programme: experiences of stakeholders in the north east of England. Health Promot Int. 2014. June;29(2):201–211. doi: 10.1093/heapro/das072 [DOI] [PubMed] [Google Scholar]
- 24.Reese N Internet access in Virginia: stats & figures. Broad Band Now Website. https://broadbandnow.com/Virginia. Accessed April 29, 2019. [Google Scholar]
- 25.Virginia broadband availability map and integrated broadband planning and analysis toolbox. Broad Band Website. 2009. https://broadband.cgit.vt.edu/IntegratedToolbox/. [Google Scholar]
- 26.Wieland LS, Falzon L, Sciamanna CN, et al. Interactive computer-based interventions for weight loss or weight maintenance in overweight or obese people. Cochrane Database Syst Rev. 2012. August 15(8). doi: 10.1002/14651858.CD007675.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sherrington A, Newham JJ, Bell R, Adamson A, McColl E, Araujo-Soares V. Systematic review and meta-analysis of internet-delivered interventions providing personalized feedback for weight loss in overweight and obese adults. Obes Rev. 2016. June;17(6):541–551. doi: 10.1111/obr.12396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rogers MA, Lemmen K, Kramer R, Mann J, Chopra V. Internet-delivered health interventions that work: systematic review of meta-analyses and evaluation of website availability. J. Med. Internet Res. 2017. March 24;19(3):e90–e90. doi: 10.2196/jmir.7111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sorgente A, Pietrabissa G, Manzoni GM, et al. Web-based interventions for weight loss or weight loss maintenance in overweight and obese people: a systematic review of systematic reviews. J. Med. Internet Res. 2017. June 26;19(6):e229–e229. doi: 10.2196/jmir.6972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beleigoli AM, Andrade AQ, Cancado AG, Paulo MN, Diniz MFH, Ribeiro AL. Web-based digital health interventions for weight loss and lifestyle habit changes in overweight and obese adults: systematic review and meta-analysis. J. Med. Internet Res. 2019. January 8;21(1):e298. doi: 10.2196/jmir.9609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Afshin A, Babalola D, McLean M, et al. Information technology and lifestyle: a systematic evaluation of internet and mobile interventions for improving diet, physical activity, obesity, tobacco, and alcohol use. J Am Heart Assoc. 2016. August 31;5(9). doi: 10.1161/JAHA.115.003058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Olson CM. behavioral nutrition interventions using e- and m-health communication technologies: a narrative review. Annu Rev Nutr. 2016. July;36:647–664. doi: 10.1146/annurev-nutr-071715-050815 [DOI] [PubMed] [Google Scholar]
- 33.Zoellner J, Hedrick V, You W, et al. Effects of a behavioral and health literacy intervention to reduce sugar-sweetened beverages: a randomized-controlled trial. Int J Behav Nutr Phys Act. 2016. March 22;13(38). doi: 10.1186/s12966-016-0362-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zoellner JM, You W, Estabrooks PA, et al. Supporting maintenance of sugar-sweetened beverage reduction using automated versus live telephone support: findings from a randomized control trial. Int J Behav Nutr Phys Act. 2018. October 4;15(1):97. doi: 10.1186/s12966-018-0728-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hedrick VE, Davy BM, Myers EA, You W, Zoellner JM. Changes in the healthy beverage index in response to an intervention _targeting a reduction in sugar-sweetened beverage consumption as compared to an intervention _targeting improvements in physical activity: results from the talking health trial. Nutrients. 2015. December 4;7(12):10168–10178. doi: 10.3390/nu7125525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davy BM, Jahren AH, Hedrick VE, You W, Zoellner JM. Influence of an intervention _targeting a reduction in sugary beverage intake on the delta13C sugar intake biomarker in a predominantly obese, health-disparate sample. Public Health Nutr. 2017. January;20(1):25–29. doi: 10.1017/S1368980016001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vargas-Garcia EJ, Evans CEL, Prestwich A, Sykes-Muskett BJ, Hooson J, Cade JE. Interventions to reduce consumption of sugar-sweetened beverages or increase water intake: evidence from a systematic review and meta-analysis. Obes Rev. 2017. July 18;18(11):1350–1363. doi: 10.1111/obr.12580 [DOI] [PubMed] [Google Scholar]
- 38.Porter KJ, Brock DJ, Estabrooks PA, et al. SIPsmartER delivered through rural, local health districts: adoption and implementation outcomes. BMC Public Health. 2019. September 18;19(1):1273–1273. doi: 10.1186/s12889-019-7567-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999. September;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004. February;27(1):3–12. doi: 10.1207/s15324796abm2701_2 [DOI] [PubMed] [Google Scholar]
- 41.Robert Wood Johnson Foundation. County health rankings and road maps: Virginia 2015. 2015; http://www.countyhealthrankings.org/app/virginia/2015/overview. Accessed January 10, 2015.
- 42.Virginia Department of Health Office of Health Equity. Virginia Health Opportunity Index. 2016; https://www.vdh.virginia.gov/health-equity/. Accessed February 8, 2017.
- 43.Krause D, Cossman J, May W. Oral health in Appalachia: regional, state, sub-state, and national comparisons. J Appalach Stud. 2016. April;22(1):80–102. doi: 10.5406/jappastud.22.1.0080 [DOI] [Google Scholar]
- 44.Relative poverty rates in Appalachia, 2009–2013. Appalachian Regional Commission Website. 2015; http://www.arc.gov/research/MapsofAppalachia.asp?MAP_ID=115. Accessed 20 October, 2015.
- 45.Education – high school and college completion rates, 2009–2013: Appalachian Virginia. Appalachian Regional Commission Website. 2015; http://www.arc.gov/reports/custom_report.asp?REPORT_ID=61. Accessed 10 January, 2016.
- 46.Health literacy data map. The University of North Carolina at Chapel Hill Website. 2014; http://healthliteracymap.unc.edu/#. Accessed May 11, 2019.
- 47.McDermott MS, Oliver M, Simnadis T, et al. The theory of planned behaviour and dietary patterns: a systematic review and meta-analysis. Prev Med. 2015. September 5;81:150–156. doi: 10.1016/j.ypmed.2015.08.020 [DOI] [PubMed] [Google Scholar]
- 48.Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996. Nov-Dec;11(2):87–98. doi: 10.4278/0890-1171-11.2.87 [DOI] [PubMed] [Google Scholar]
- 49.Berkman N, DeWalt D, Pignone M, et al. Literacy and Health Outcomes Rockville, MD: Agency for Healthcare Research and Quality: RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290–02-0016; 2004. [Google Scholar]
- 50.Berkman N, Sheridan S, Donahue K, et al. Health literacy interventions and outcomes: An update of the literacy and health outcomes systematic review of the literature. Chapel Hill, NC: RTI International-University of North Carolina Evidence-based Practice Center; 2011. [Google Scholar]
- 51.Allen K, Zoellner J, Motley M, Estabrook P. Understanding the internal and external validity of health literacy interventions: a systematic literature review using the RE-AIM framework. J Health Commun 2011. September;16(Suppl 3):55–72. doi: 10.1080/10810730.2011.604381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huizinga MM, Beech BM, Cavanaugh KL, Elasy TA, Rothman RL. Low numeracy skills are associated with higher BMI. Obesity. 2008. June 5;16(8):1966–1968. doi: 10.1038/oby.2008.294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care. 2009. April 28;32(9):1614–1619. doi: 10.2337/dc09-0425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taggart J, Williams A, Dennis S, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Family Practice. 2012. June 1;13(49). doi: 10.1186/1471-2296-13-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promotion Int. 2018. October 1;33(5):901–911. doi: 10.1093/heapro/dax015 [DOI] [PubMed] [Google Scholar]
- 56.Aufderheide P Part II: Conference Proceedings and Next Steps. Washington, D.C.: Communications and Society Program of the Aspen Institute; 1993. [Google Scholar]
- 57.Porter KJ, Chen Y, Lane HG, Zoellner JM. Implementation of media production activities in an intervention designed to reduce sugar-sweetened beverage intake among adults. J Nutr Educ Behav. 2017. February;50(2):173–179. doi: 10.1016/j.jneb.2017.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mills SD, Tanner LM, Adams J. Systematic literature review of the effects of food and drink advertising on food and drink-related behaviour, attitudes and beliefs in adult populations. Obes Rev. 2013. January 9;14(4):303–314. doi: 10.1111/obr.12012 [DOI] [PubMed] [Google Scholar]
- 59.Higgins JW, Begoray D. Exploring the borderlands between media and health: conceptualizing ‘critical media health literacy’. J Media Lit Educ. 2013;42(2). [Google Scholar]
- 60.Bergsma LJ, Carney ME. Effectiveness of health-promoting media literacy education: a systematic review. Health Educ Res. 2008. January 17;23(3):522–542. doi: 10.1093/her/cym084 [DOI] [PubMed] [Google Scholar]
- 61.Martens H Evaluating media literacy education: concepts, theories and future directions. J Media Lit Educ. 2013;2(1). [Google Scholar]
- 62.Hedrick V, Comber D, Estabrook P, Savla J, Davy B. The beverage intake questionnaire: determining initial validity and reliablity. J Am Diet Assoc. 2010. August;110(8):1227–1232. doi: 10.1016/j.jada.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hedrick VE, Comber DL, Ferguson KE, et al. A rapid beverage intake questionnaire can detect changes in beverage intake. Eat Behav. 2013. January;14(1):90–94. doi: 10.1016/j.eatbeh.2012.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hedrick VE, Savla J, Comber DL, et al. Development of a brief questionnaire to assess habitual beverage intake (BEVQ-15): sugar-sweetened beverages and total beverage energy intake. J Acad Nutr Diet. 2012. June;112(6):840–849. doi: 10.1016/j.jand.2012.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ritterband LM, Thorndike FP, Ingersoll KS, et al. Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: a randomized clinical trial. JAMA Psychiatry. 2017. January 1;74(1):68–75. doi: 10.1001/jamapsychiatry.2016.3249 [DOI] [PubMed] [Google Scholar]
- 66.Ritterband LM, Thorndike FP, Gonder-Frederick LA, et al. Efficacy of an internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009. July;66(7):692–698. doi: 10.1001/archgenpsychiatry.2009.66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008. May;27(3):379–387. doi: 10.1037/0278-6133.27.3.379 [DOI] [PubMed] [Google Scholar]
- 68.Health literacy. US Department of Health and Human Services website https://health.gov/our-work/health-literacy. Accessed February 28, 2021.
- 69.Sherman B, Gilliland G, Speckman J, Freund K. The effect of a primary care exercise intervention for rural women. Prev Med. 2007. March;44(3):198–201. doi: 10.1016/j.ypmed.2006.10.009 [DOI] [PubMed] [Google Scholar]
- 70.Porter K, Alexander R, Kružliakova N, Perzynski K, Zoellner J. Using the clear communications index to improve materials for a behavioral intervention. Health Commun. 2018. June;8:1–7. doi: 10.1080/10410236.2018.1436383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Porter K, Chen Y, Estabrooks P, Noel L, Baily A, Zoellner J. Using teach-back to understand participant behavioral self-monitoring skills across health literacy levels and behavioral condition. J Nutr Educ Behav. 2015. December 10;48(1):20–26. doi: 10.1016/j.jneb.2015.08.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alkhaldi G, Hamilton FL, Lau R, Webster R, Michie S, Murray E. The effectiveness of prompts to promote engagement with digital interventions: a systematic review. J. Med. Internet Res. 2016. August 1;18(1):e6–e6. doi: 10.2196/jmir.4790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barello S, Triberti S, Graffigna G, et al. eHealth for Patient Engagement: A Systematic Review. Front Psychol. 2016. January 8;6(2013). doi: 10.3389/fpsyg.2015.02013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Michie S, Perski O, Blandford A, West R. Conceptualising engagement with digital behaviour change interventions: a systematic review using principles from critical interpretive synthesis. Transl Behav Med. 2016. June;7(2):254–267. doi: 10.1007/s13142-016-0453-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yardley L, Spring BJ, Riper H, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016. November;51(5):833–842. doi: 10.1016/j.amepre.2016.06.015 [DOI] [PubMed] [Google Scholar]
- 76.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss BD. Screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006. August;21(8):874–877. doi: 10.1111/j.1525-1497.2006.00532.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jeppesen KM, Coyle JD, Miser WF. Screening questions to predict limited health literacy: a cross-sectional study of patients with diabetes mellitus. Ann Fam Med. 2009. Jan-Feb;7(1):24–31. doi: 10.1370/afm.919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morris N, MacLean C, Chew L, Littenberg B. The single item literacy screener: evaluation of a brief instrument to identify limited reading ability. BMC Fam Pract. 2006. March 24;7(1):21. doi.org/10.1186/1471–2296-7–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen Y, Porter K, You W, Estabrooks P, Zoellner J. A health/media literacy intervention improves adults’ interpretations of sugar-sweetened beverage advertising. J Media Lit Educ. 2020. April 28;12(1):30–38. doi: 10.23860/JMLE2020-12-1-6 [DOI] [Google Scholar]
- 80.Healthy Days Core Module: HRQOL-14 Measure. Centers for Disease Control and Prevention. https://www.cdc.gov/hrqol/hrqol14_measure.htm. Last Edited October 31, 2018. Accessed October 17, 2017.
- 81.Chen Y, Porter KJ, Estabrooks PA, Zoellner J. Development and evaluation of the sugar-sweetened beverages media literacy (SSB-ML) scale and its relationship with SSB consumption. Health Commun. 2016. October 3;32(10):1–8. doi: 10.1080/10410236.2016.1220041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Weiss B, Mays M, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005. Nov-Dec;3(6):514–522. doi: 10.1370/afm.405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Norman CD, Skinner HA. eHEALS: The eHealth Literacy Scale. J Med Internet Res. 2006. November 14;8(4):e27. doi: 10.2196/jmir.8.4.e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Patterson RE, Kristal AR, Shannon J, Hunt JR, White E. Using a brief household food inventory as an environmental indicator of individual dietary practices. Am J Public Health. 1997. February;87(2):272–275. doi: 10.2105/ajph.87.2.272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.National health and nutrition examination survey. NCHS. 2021. Jun 14: Center for Disease Control Website. https://www.cdc.gov/nchs/nhanes/index.htm. [Google Scholar]
- 86.Boles RE, Burdell A, Johnson SL, Gavin WJ, Davies PL, Bellows LL. Home food and activity assessment. Development and validation of an instrument for diverse families of young children. Appetite. 2014. May 2;80:23–27. doi: 10.1016/j.appet.2014.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.CDC - BRFSS - Questionnaires. Centers for Disease Control and Prevention. http://www.cdc.gov/brfss/questionnaires/index.htm. Last Edited January 14, 2021. Accessed February 28, 2021
- 88.Howell JL, Shepperd JA. Establishing an Information Avoidance Scale. Psychol Assess. 2016. April 21;28(12):1695–1708. doi: 10.1037/pas0000315 [DOI] [PubMed] [Google Scholar]
- 89.Schumacher LM, Martinelli MK, Convertino AD, Forman EM, Butryn ML. Weight-related information avoidance prospectively predicts poorer self-monitoring and engagement in a behavioral weight loss intervention. Ann Behav Med. 2021. June 3;55(2):103–111. doi: 10.1093/abm/kaaa034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kiernan M, Schoffman DE, Lee K, et al. The Stanford leisure-time activity categorical item (L-Cat): a single categorical item sensitive to physical activity changes in overweight/obese women. Int J Obes. 2013. April 16;37(12):1597–602. doi: 10.1038/ijo.2013.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kruzliakova N, Estabrooks PA, You W, et al. The relationship between the stanford leisure-time activity categorical item and the Godin leisure-time exercise questionnaire among rural intervention participants of varying health literacy status. J Phys Act Health. 2018. April 1;15(4):269–278. doi: 10.1123/jpah.2017-0284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ross KM, Leahey TM, Kiernan M. Validation of the stanford leisure-time activity categorical item (L-Cat) using armband activity monitor data. Obes Sci Pract. 2018. February 7;4(3):276–282. doi: 10.1002/osp4.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989. May;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 94.Ritterband LM, Ardalan K, Thorndike FP, et al. Real world use of an Internet intervention for pediatric encopresis. J Med Internet Res. 2008. June 30;10(2):e16. doi: 10.2196/jmir.1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Thorndike FP, Saylor DK, Bailey ET, Gonder-Frederick L, Morin CM, Ritterband LM. Development and perceived utility and impact of an internet intervention for insomnia. E J Appl Psychol. 2008;4(2):32–42. doi: 10.7790/ejap.v4i2.133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ritterband LM, Borowitz S, Cox DJ, et al. Using the internet to provide information prescriptions. Pediatrics. 2005. November;116(5):e643–647. doi: 10.1542/peds.2005-0404 [DOI] [PubMed] [Google Scholar]
- 97.Tan SS, Bouwmans CA, Rutten FF, Hakkaart-van Roijen L. Update of the Dutch Manual for Costing in Economic Evaluations. Int J Technol Assess. 2012. April;28(2):152–158. doi: 10.1017/S0266462312000062 [DOI] [PubMed] [Google Scholar]
- 98.Thompson FE, McNeel TS, Dowling EC, Midthune D, Morrissette M, Zeruto CA. Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in adults in the United States: National Health Interview Survey, 2005. J Am Diet Assoc. 2009. August;109(8):1376–1383. doi: 10.1016/j.jada.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Park S, Xu F, Town M, Blanck HM. Prevalence of sugar-sweetened beverage intake among adults−−23 states and the district of columbia, 2013. MMWR. 2016. February 26;65(7):169–174. doi: 10.15585/mmwr.mm6507a1 [DOI] [PubMed] [Google Scholar]
- 100.Zoellner J, You W, Connell C, et al. Health literacy is associated with healthy eating index scores and sugar-sweetened beverage intake: findings from the rural lower Mississippi Delta. J Am Diet Assoc. 2011. July;111:1012–1020. doi: 10.1016/j.jada.2011.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. adults, 2011–2014. NCHS Data Brief. 2017. January(270):1–8. [PubMed] [Google Scholar]
- 102.Joo JW, Hormozdiari F, Han B, Eskin E. Multiple testing correction in linear mixed models. Genome Biol. 2016. April 1;17:62. doi: 10.1186/s13059-016-0903-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Gelman A, Hill J, Yajima M. Why we (usually) don’t have to worry about multiple comparisons. J Res Educ Eff. 2012. April 3;5:189–211. doi: 10.1080/19345747.2011.618213 [DOI] [Google Scholar]
- 104.Glasgow RE, Klesges LM, Dzewaltowski DA, Estabrooks PA, Vogt TM. Evaluating the impact of health promotion programs: using the RE-AIM framework to form summary measures for decision making involving complex issues. Health Educ Res. 2006. August 31;21(5):688–694. doi: 10.1093/her/cyl081 [DOI] [PubMed] [Google Scholar]
- 105.US Census Bureau. http://www.census.gov/, Accessed October 25, 2010.
- 106.Zhao X, Lynch JG, Chen Q. Reconsidering Baron and Kenny: myths and truths about mediation analysis. J Assoc Consum Res. 2010. February 15;37:197–206. doi: 10.1086/651257 [DOI] [Google Scholar]
- 107.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010. October;15(4):309–334. doi: 10.1037/a0020761 [DOI] [PubMed] [Google Scholar]
- 108.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009. August 7;4(1):1–15. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Graneheim U, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004. February;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001 [DOI] [PubMed] [Google Scholar]
- 110.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008. April;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 111.Patton M Qualitative Reserach & Evaluation Methods. 3rd ed. Thousands Oak: Sage Pulblication, Inc.; 2002. [Google Scholar]
- 112.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005. November;15(9):1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 113.Creswell J, Plano Clark V. Designing and Conducting Mixed Methods Research. Thousands Oaks, CA: Sage Publication, Inc.; 2007. [Google Scholar]
- 114.Keena L, Labbe L, Barrett J, Pfister M. Modeling and simulation of adhearance: approached and applications in therapeutics. AAPS J. 2005. October 5;7(2):E390–E407. doi: 10.1208/aapsj070240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lee MM, Falbe J, Schillinger D, Basu S, McCulloch CE, Madsen KA. Sugar-sweetened beverage consumption 3 years after the Berkeley, California, sugar-sweetened beverage tax. Am J Public Health. 2019. February 21;109(4):637–639. doi: 10.2105/AJPH.2019.304971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Silver LD, Ng SW, Ryan-Ibarra S, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: A before-and-after study. PLoS Med. 2017. April 18;14(4):e1002283. doi: 10.1371/journal.pmed.1002283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhong Y, Auchincloss AH, Lee BK, Kanter GP. The short-term impacts of the Philadelphia Beverage Tax on beverage consumption. Am J Prev Med. 2018. July;55(1):26–34. doi: 10.1016/j.amepre.2018.02.017 [DOI] [PubMed] [Google Scholar]
- 118.Chriqui JF, Chaloupka FJ, Powell LM, Eidson SS. A typology of beverage taxation: multiple approaches for obesity prevention and obesity prevention-related revenue generation. J Public Health Policy. 2013. May 23;34(3):403–423. doi: 10.1057/jphp.2013.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Backholer K, Sarink D, Beauchamp A, et al. The impact of a tax on sugar-sweetened beverages according to socio-economic position: a systematic review of the evidence. Public Health Nutr. 2016. May 16;19(17):3070–3084. doi: 10.1017/S136898001600104X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hagenaars LL, Jeurissen PPT, Klazinga NS. The taxation of unhealthy energy-dense foods (EDFs) and sugar-sweetened beverages (SSBs): an overview of patterns observed in the policy content and policy context of 13 case studies. Health Policy (Amst). 2017. July 8;121(8):887–894. doi: 10.1016/j.healthpol.2017.06.011 [DOI] [PubMed] [Google Scholar]
- 121.Tamir O, Cohen-Yogev T, Furman-Assaf S, Endevelt R. Taxation of sugar sweetened beverages and unhealthy foods: a qualitative study of key opinion leaders’ views. Isr J Health Policy Res. 2018. July 31;7(1):43. doi: 10.1186/s13584-018-0240-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.National Academy of Sciences, Engineering and Medicine. 2018 Community-Based Health Literacy Interventions: Proceedings of a Workshop. Washington DC, 2018: The National Academies Press. doi: 10.17226/24917 [DOI] [PubMed] [Google Scholar]
- 123.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. Health Behav Health Educ. 2008;5(43–64). [Google Scholar]
- 124.Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009. July 15;6(3):A82–A82. [PMC free article] [PubMed] [Google Scholar]


